Dave Bunting
The results of a YouGov survey of surgeons commissioned by the Royal College of Surgeons of England was published last week reporting that 68% surgeons are considering early retirement due to pensions tax regulations, 64% surgeons have been advised to work fewer hours in the NHS and 69% consultant surgeons have reduced the amount of time spent working in the NHS as a result of pension tax rules. Aa a result, NHS waiting lists will inevitable increase. It is vital therefore that day case surgery services - which account for the vast majority of procedures performed in the UK – are utilised effectively to maximise productivity within an environment of reduced operating sessions. In addition, the Royal College of Emergency Medicine recently published an analysis suggesting the NHS will require 4000 additional beds this winter to avoid ‘corridor care’ and keep bed occupancy at a safe level. It is well understood that effective use of day case surgery is one way of reducing the demand on inpatient beds, therefore, it is vital we prioritise and protect day surgery services.
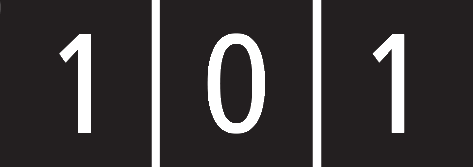
BADS continues to work closely with a number of national organisations including the Royal Colleges, Getting it Right First Time (GiRFT), the Model Hospital. BADS also co-hosts a number of national and regional meetings in association with external organisations such as Health Care Conferences UK (HCUK). A conference on Developing Your Daycase General Surgery Service (BADS/HCC) is being held at the Studio Conference Centre, Birmingham on Tuesday 21st January and a conference on Daycase hip replacement surgery is being held at the De Vere Conference Centre, London on Monday 27th January. Further details can be found in this edition of JODS. BADS members are eligible for a 25% discount on registration fees for these events.
It is a pleasure of mine to be able to introduce several new members of the BADS Council. I welcome Mr Adam Kimble, Mrs Karen Harries, Mr Shaun Clee, Mr Edward Dunstan, Mr Stamatios Karavolos and Mr Richard Parkinson. Please take the time to find out more about them and the qualities they bring to BADS Council in the New Council Members section of this edition.
JODS has been working with the BADS legal advisers to strengthen its position with regards to copyright of published material to provide the necessary protection for the benefit of authors and the journal alike. All future submissions must now be accompanied by the copyright transfer agreements for each named author. Full details can be found in the guidelines for authors included in this publication and accessible via the BADS website here:
https://daysurgeryuk.net/en/resources/guidelines-for-authors/
This edition of JODS contains scientific articles on regional anaesthesia provided by Anaesthesia Associates in day case hysterectomy; a case report of a subcapsular liver haematoma following day case laparoscopic cholecystectomy together with review of differential diagnoses and a report of a completed audit cycle demonstrating improvement in the documentation of operation notes with the use of a dedicated operation note proforma.
Finally, preparations for the Annual Conference being held at the Cardiff City Hall on 25th and 26th June are progressing well. Please put the dates in your diary and book your study leave now! Abstract submissions will open on 1st January so now is the time to think about getting your project data recorded and analysed in preparation to submit your work.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/30717/29-4-editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse0

Kim Russon
In September the Anaesthesia and Perioperative Medicine GIRFT (Get It Right First Time) team visited my Trust, which was very enlightening. For those of you not familiar with GIRFT, it began as a pilot within Orthopaedics led by Professor Tim Briggs an orthopaedic surgeon. Variation in practice was identified which was thought to be impacting on quality of care and patient outcomes, so the programme was rolled out nationally with the intention to “identify areas of good practice and agree where changes can be made”. GIRFT is working through the specialities and has published a number of specialty reports available via their website. Day surgery has been identified as an area with significant national variation.
From the perspective of having GIRFT visit my Trust it was a positive experience. GIRFT expect representation from clinicians, managers and the Executive team. The data presented was little bit out of date, but it was based on the Trust’s HES data so needed to be considered. If the data is not presenting what you are expecting, then you need to look at how it is being recorded and how it is being submitted. It is your Trust’s data.
Based on GIRFT data and Model Hospital data, BADS has identified there is wide national variation in day case rates for Anterior Cruciate Ligament reconstruction and thus are planning a joint BADS / HCC conference “From ACLr to Total Knee replacement as day case” on 30th April 2020 in London. Members of the GIRFT team will be presenting at our Joint BADS /HCC conference on Day case General Surgery in Birmingham on 21st January 2020 and our annual conference in June in Cardiff, discussing variation and how it might be addressed. I am looking forward to hearing from them and hope you will consider joining us.
The Model Hospital is a way of monitoring your hospital’s day case rates. This is provided by NHS Improvement and is accessible by anyone who has an NHS email address. Dr Mary Stocker, past president of BADS, has been working very closely with the Model Hospital team and the latest version has been launched this week which maps to the BADS Directory of Procedures 6th Edition. The day surgery module can show your overall rates, by speciality, by procedure and show how your rates compare nationally. This information is based on HES data so ensuring you Trust data is correct is key. Are your patients planned / listed as a day case and then successfully go home the same day and recorded as such?
In the last couple of months BADS has received the very sad news of the deaths of Dr Lawrence Rowe, who was pivotal in the development of the current BADS website and Professor Paul Jarrett, who was a founder member of the society and a past president. BADS is hugely indebted to them and further detail of their remarkable work can be found on the BADS website. My thanks to Dr Anna Lipp who has written Dr Rowe’s obituary published in this edition of JODS which is to be shared with SIVA (Society of Intravenous Anaesthesia) where he also had a huge involvement. Professor Jarrett’s obituary will be published in the next edition of JODS. I extend my condolences to their families at this sad time.
In addition to the new council members whose biographies you can read in this edition of JODS, I would like to welcome 3 co-opted members: Mr Richard Parkinson (British Orthopaedic Association), Dr Stamatios Karavolos (Royal College of Obstetrics & Gynaecology) and Mr. Andrei Tanase (Association of Surgeons in Training).
My thanks to everyone for promoting and progressing day surgery and all the best for the rest of 2019.
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse1
Click on the image to be taken to the HCUK page about the conference.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/30730/hcuk-breast-day-surgery-feb-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse4
Howard Cox Heart of England NHS Foundation Trust
Abstract: Anaesthesia Associates (AA) formally known as Anaesthesia Practitioner (AP) and up until 1st of July 2019 Physicians’ Assistants’ in Anaesthesia (PA(A)) have been working in a qualified capacity within the National Health Service (NHS) since January 2007. This group of anaesthetic professionals can now take on a number of extended roles beyond qualification such as regional anaesthesia. One such enhanced role includes delivery of spinal anaesthesia within a day case and short stay surgical care setting. Anaesthesia Associates are involved in spinal anaesthesia for short stay elective Gynaecology cases. This study focuses on AA clinical work and outcome measures for Length of Stay (LOS) in conjunction with anaesthetic and surgical complications, at a single centre NHS Hospital.
Introduction
Qualified Anaesthesia Associates (AAs) have been working in the National Health Service (NHS) since January 2007. The scope of practice has been governed by the Royal College of Anaesthetists (RCoA) ‘Supervision statements’ [1]. It is acknowledged by the RCoA that AA scope of practice has change and diversified following robust local governance and educational frameworks (seen here is the example of the ‘Spinal Anaesthesia’ Governance and education policy within Heartlands, Good Hope and Solihull [HGS] formally known as Heart of England Trust {HEFT}). This group of anaesthetic professionals can now take on a number of extended roles such as regional anaesthesia. One such enhanced role includes delivery of spinal anaesthesia within a day case and sort stay surgical care setting. Anaesthesia Associates administer spinal anaesthesia for short stay elective Gynaecology cases within the University Hospital Birmingham (UHB) Trust and at Good Hope Hospital (GHH) site. This study focuses on AA clinic work and outcome measures of length of stay (LOS), as well as anaesthetic and surgical complication for elective hysterectomy patients.
Aims
To identify if LOS for elective gynaecology hysterectomy patients and anaesthetic/surgical complication rates are adversely affected when patients receive an anaesthetic administered by an AA. Identifying if the patient receiving the anaesthetic, either under spinal or general anaesthesia (GA) and or a combination of the both had any effect on outcome measures.
PA-(A) Spinal governance and training package within HGS:
Methods
Once the researcher’s data clearance was authorised the study period determined ran from 1st of January 2017 until the 31st of December 2018. It focused on the gynaecology theatres at GHH and the three sessions each week where the AA cover working in a 2 to1 model. The 2 to1 model allows one consultant anaesthetist to supervise two AAs in adjacent theatres in the delivery of anaesthesia [2].
Using the hospitals electronic theatre logbook known as ‘Concerto’, the researcher was able to identify if the AA was the primary anaesthetic provider and if the list was covered in a 2 to1 supervising capacity. The researcher could obtain the patients procedure and two groups were identified, one for laparoscopic hysterectomy and the other for open hysterectomy cases. A further detail on the type of hysterectomy performed was not determined in this study. The patients recruited for this study were all elective patients, who had received pre-operative assessment in the nurse-led clinic. All patients had capacity to consent for procedures themselves and were over 18 years of age.
The researcher then utilised the electronic discharge summery to obtain the LOS and identify if there were any surgical or anaesthetic complication which contributed to an increase in LOS. Re-admission rates were not recorded in this study as these were classed as separate episodes.
In total the researcher recruited 93 patients undergoing hysterectomy, receiving their anaesthetic from an AA within the study period time frame. The American Society of Anaesthesiologist (ASA) grade of the 93 recruit patients was as such; ASA 1, 15 cases, ASA 2, 59 cases and ASA 3, 19 cases.
The researcher undertook a literature review and reviewed text over a 10-year period from 2009 to present using EMBASE, MEDLINE, NICE guidelines and Royal College of Obstetricians and Gynaecologists data bases.
Results
Open Hysterectomy
To consider the open hysterectomy procedure first, of the 40 cases 15 had a GA only and 25 had a combination of spinal and GA the mean LOS for GA only was 53 hours with and the mean LOS in the spinal and GA group was 48 hours. The ASA breakdown for this cohort ASA 1, 2 cases, ASA 2, 23 cases and ASA 3, 15 cases. Patient information literature in the NHS suggests patients should expect on average a 1 – 4 day LOS in hospital [3].
Complication rates in the open hysterectomy group identified 4 cases where discharge was delayed above 53 hours. The complications were 2 cases, who had post-operative infection and 2 had post-operative bleeding. This identified a complication rate of 1.6%. Research from ‘The International journal of Obstetrics & Gynaecology’ [4] Suggests In a study of 239 patients the mean LOS for open hysterectomy could be 96 hours and the complication rate of 4.9%. Such findings are also supported by a study of 181 patient’s states with a mean LOS of 72 hours for abdominal hysterectomy and 48 hours for vaginal hysterectomy [5].
There were no reported anaesthetic complications in this patient cohort and no evidence to suggest that the use of AA had led to an increase in LOS or complication.
Laparoscopic Hysterectomy
The analysis of the patients who were converted from laparoscopic to open hysterectomy was considered separately. There were 53 patients in this cohort, of which 41 patients had a GA + Spinal and 12 patients had just a GA. Mean LOS for the GA + Spinal group was 18 hours and the mean LOS for the GA only group was 16 hours.
There were two complications including one case of post-operative nausea and vomiting (PONV) resulting in a LOS of 24 hours and one wound infection resulting in a LOS of 54 hours.
There is little difference in LOS when complaining anaesthetic types. The review of literature identified the laparoscopic technique associated with the shortest LOS [5],[6] & [7]. There was however one anaesthetic complication of PONV which demonstrated and anaesthetic complication rate of 2.3% or 1.8% if the laparoscopic converted cases are counted within that figure
Conversion from Laparoscopic to open Hysterectomy
Of the total number of patients undergoing laparoscopic hysterectomy (53), 11 of these were converted to an open hysterectomy. All patients in this group had a GA + Spinal combination.
The mean LOS for this group was 20 hours with one significant post-operative complication of wound infection which resulted in a LOS of 40 hours. The conversion rate from laparoscopic to open hysterectomy during the study time period was 5.8%.
In a study of laparoscopic hysterectomy reviewing 1051 cases, a conversion rate of 5% is described [8] and further study of 1534 patients suggests a conversion rate of 4.6% [9] & [10].
Conclusions
The researcher did identify one anaesthetic complication relating to PONV within the laparoscopic group. Looking at this complication and relating this to the total number of patients is the study this represent a complication rate of 1.07%.
The researcher on reviewing the electric discharge information did not identify any procedural complication from the Spinal and GA techniques. The researcher did not review each written anaesthetic record for each study patient so potential records of anaesthetic procedural difficulties could have been missed by the researcher. It is also understood by the researcher that potentially all the spinals were not administered by the AA. This acknowledgement is balanced against the researcher’s ability to identify intermediate and major anaesthetic complications which were documented in the electronic discharge information.
The supervision of AA within this study timeframe follows guidelines laid down by the RCoA [1]. The AA workings within HGS also adhere to locally developed supervision and calling criteria guidelines which govern AA practice which is included in the conclusion. Seen here is the example of the, [‘Guidance for Consultant Anaesthetist supervising Anaesthetic Practitioner.’ policy within Heartlands, Good Hope and Solihull [HGS] formally known as Heart of England Trust {HEFT}].
 This study helps to identify and showcase the versatility of the AA profession in the delivery of extended anaesthetic services and how the 2 to 1 model of working as suggested by the RCoA [1] is both a safe and effective workforce solution.
This study helps to identify and showcase the versatility of the AA profession in the delivery of extended anaesthetic services and how the 2 to 1 model of working as suggested by the RCoA [1] is both a safe and effective workforce solution.
The study also supported existing literature trends that laparoscopic hysterectomy is associated with reduced LOS which is not anaesthetic technique dependent.
References
- PA-(A) Supervision and limitation of scope of Practice (May 2011 revision) http://www.rcoa.ac.uk
- Planning the introduction and training for Physician’s’ Assistant (Anaesthesia) 2016 https://www.rcoa.ac.uk
- Hysterectomy NHS2019. .
- Length of stay for hysterectomies in one large DGH-what role does this have in enhanced recovery? Haldane K. BJOG: An International Journal of Obstetrics and Gynaecology 2016;123:201.
- Using international data to set benchmarks for morbidity outcomes after hysterectomy. Pandit Meghana J. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 2016;133(1):84-88.
- A retrospective benchmark audit to evaluate length of stay by route of hysterectomy Tomlinson F. Gynaecological Surgery 2015;12(1).
- Predictors of length of stay after vaginal hysterectomy Kruger P.F. Journal of Minimally Invasive Gynaecology 2015;22(6):-.
- Minilaparotomy vs. laparoscopic hysterectomy: comparison of length of hospital stay. Perron-Burdick Misa Journal of minimally invasive gynaecology 2014;21(4):619-623.
- J Keurentjes, J M Briet, H Geertruida and J.E>.Mouritis. (2018)Surgical Endoscopy (2018) Volume 32(2) pages 1021-1026.
- The Journal of Minimally Invasive Gynaecology A R H Andries, D Mathijis, M D Blikkendaal, W V Z Erik & F W Jansen (2012) https://doi.org/10.1016/j.jmig.2012.09.06.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/30714/29-4-cox.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse5
Louise Dunphy Frimley Health NHS Foundation Trust
Email: louise.dunphy1@nhs.net
Laparoscopic cholecystectomy is the gold standard treatment for symptomatic cholelithiasis. Complications can occur including haemorrhage, iatrogenic bile duct injury, gallbladder perforation, conversion to an open procedure and choledocholithiasis postoperatively. Subcapsular liver haematoma is a rare, life-threatening complication occurring after laparoscopic cholecystectomy. Anatomical variations, pseudoaneurysms, the use of NSAIDs, haemangioma and iatrogenic liver damage have been suggested as possible risk factors. There is a paucity of cases reported. Depending on the time of onset of the patient’s symptoms, treatment can vary from expectant to surgical management. The authors present the case of a 79-year-old female presenting to the Emergency Department one day following a laparoscopic cholecystectomy with right upper quadrant abdominal pain and hypovolaemic shock. Further investigation with a CT confirmed the diagnosis of a subcapsular liver haematoma. She underwent right hepatic artery embolization. This paper will provide an overview of the aetiology, risk factors, clinical presentation, investigations and management of a subcapsular liver haematoma. It offers an important clinical reminder of maintaining a high index of clinical suspicion in patients presenting with acute onset abdominal pain and hypovolaemic shock following a laparoscopic cholecystectomy. A cystic duct stump leak due to improper clip placement, spontaneous clip displacement, ischaemic necrosis and elevated common bile duct pressures should also be considered in the differential diagnosis in patients presenting with hypovolaemic shock following cholecystectomy. An infected haematoma should also be considered in patients presenting to the Emergency Department a few weeks after surgery with abdominal pain and signs of sepsis.
Subcapsular liver haematoma, described as a blood collection under the Glisson capsule is a rare life-threatening occurrence after laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography [ERCP] or colonoscopy. It can also occur in pregnancies complicated by HELLP Syndrome [haemolysis, elevated liver enzymes and low platelets] and pre-eclampsia. It is also associated with trauma, coagulopathies, hypoxia, maternal diseases and placental lesions. Patients typically present with right upper quadrant pain which may include signs of shock if the bleeding is severe. A high index of clinical suspicion is requiring to render the diagnosis to prevent morbidity and mortality.
Presentation
79-year-old female presented to the Emergency Department, with acute onset of right upper quadrant abdominal and epigastric pain. Her medical history included hypertension, GORD, hypothyroidism, chronic renal impairment and hypercholesterolaemia. Her medications included levothyroxine 50mcgs od, lansoprazole 30mg gastro-resistant tablets, pyridoxine 50 mgs od and bendroflumethiazide 10 mgs od. Further investigation with an ultrasound scan of her abdomen showed a thin-walled gallbladder with several mobile gallstones. She underwent an elective day case laparoscopic cholecystectomy, Hem-o-lok clips were used and haemostasis was achieved. Histopathology showed features of chronic cholecystitis with cholelithiasis. One day post-surgery, she presented to the Emergency Department with acute onset confusion, abdominal pain and distension. She was hypotensive [BP 70/50mmHg] and tachycardic [heart rate 110 bpm]. On examination, guarding was elicited in the right upper quadrant.
Investigations
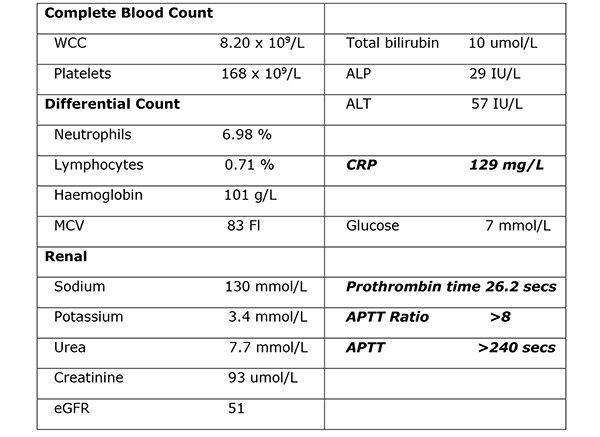
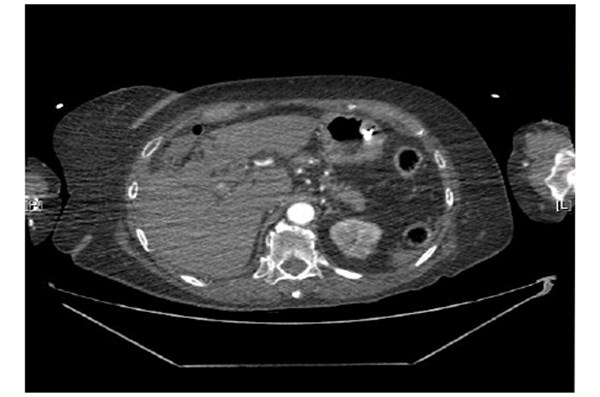
Her venous blood gas confirmed a raised lactate of 4.3mmol/l and a haemoglobin of 104g/l. Haematological investigations confirmed a raised CRP of 129mg/L, Table 1. Her chest radiograph showed atelectasis at the left base with no evidence of sub-diaphragmatic free air. Her urine dip was negative. She commenced treatment with intravenous anti-microbial therapy [amoxicillin, metronidazole, gentamicin] for suspected intra-abdominal sepsis. Further investigation with a CT abdomen and pelvis showed a large haematoma in the gallbladder bed extending down to the right paracolic gutter (Figure 1). There was a linear streak of high attenuation within the porta hepatis at the site of the cystic artery. The appearances were suggestive of a leaking cystic artery stump, although the hepatic artery itself was not clearly visualised. A small volume of fluid was noted in the pelvis. Her clotting was deranged and she received 10mgs of vitamin K IV, tranexamic acid 1g IV and three units of FFP.
Figure 1. Further investigation with a CT abdomen and pelvis showed a large haematoma in the gallbladder bed
extending down to the right paracolic gutter.
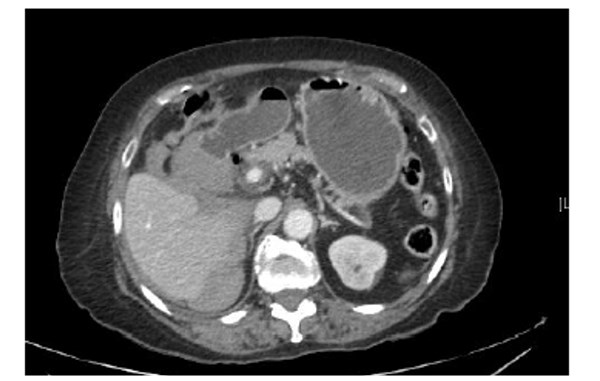
Table 1. Haematological investigations confirmed a raised CRP of 129mg/L.
Differential diagnosis
The clinical impression was of a cystic duct stump leak due to improper clip placement, clip displacement or a subcapsular liver haematoma. Further investigation with a pre-contrast CT was recommended to determine an active bleed as the clips made interpretation difficult. Pre contrast, arterial phase and delayed phase images of her abdomen and pelvis were performed. A large subcapsular collection extending along the medial inferior border of the liver, apparently extending from the gallbladder fossa was noted. Arterial phase images showed the hepatic artery lying close to and abutting the two blushes of contrast again raising the suspicion of active focal bleeding (Figure 2). Note was also made of a variation of the coeliac axis. Two main branches were the left gastric and hepatic artery. The splenic artery appeared to arise off the left gastric artery. There was a tiny accessory vessel just arising after the origin of the coeliac axis. This extended towards the right adrenal gland. Subphrenic fluid represented subcapsular haemorrhage. Two small blushes of contrast were demonstrated suspicious for contrast extravasation from an active bleeding point. A repeat blood gas confirmed a drop in her haemoglobin to 71 g/l. She was transfused two units of packed red blood cells. She was transferred to the Intensive Care Unit for further observation. She required an infusion of metaraminol to maintain her blood pressure. She was self-ventilating and no respiratory support was required. Her haemoglobin remained stable and no further transfusions were required.
Figure 2. Arterial phase images showed the hepatic artery lying close to and abutting the two blushes
of contrast again raising the suspicion of active focal bleeding.
Treatment
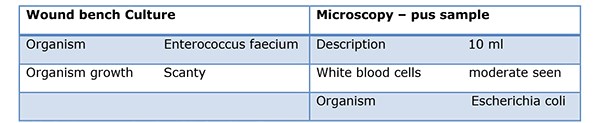
As her intermittent haemorrhage persisted, prophylactic embolization was performed. Under fluoroscopic guidance, a right renal, coeliac and selective hepatic angiogram was performed. The right hepatic artery was embolised with 710-1000 micro polyvinyl alcohol particles until stasis was achieved distal to the point of origin of the gastroduodenal artery. Despite antimicrobial therapy her high inflammatory markers persisted [WCC 17x109/L and CRP 342mg/L]. A CT Abdomen/pelvis with contrast was performed. Compared to her previous CT, an evolving right hepatic large haematoma was observed. Her anti-microbial therapy was changed to ertapenem. Under US guidance, the right hepatic complex collection was punctured using a 19G needle to obtain dark red fluid, a sample of which was sent for MC&S. In view of her sepsis, a 12F drain was inserted and placed on free external drainage. Her pus cultured Escherichia coli, Table 2.
Table 2. His pus sample cultured Escherichia coli.
Outcomes
As her inflammatory markers improved, her anti-microbial therapy was down-stepped to levofloxacin and metronidazole. She developed hypoactive delirium, hyperkalaemia [6.5mmol/L], hyponatraemia [124 mmol/l], hypomagnesemia [0.65 mmol/L] and hypophosphatemia [0.68mmol/l] resulting in a prolonged hospital stay. She was reviewed by the dietician and commenced total parenteral nutrition to maintain her calorie intake. Her electrolyte imbalance was caused by her dehydration and thiazide diuretics. She commenced treatment with melatonin modified release tablets 2mg od. Further investigation with a CT Head showed generalised involutional change predominantly affecting the temporal lobes. Her drain was removed after three weeks and an interval CT of her abdomen and pelvis two months later showed a significant reduction in the size of her haematoma. She was discharged home uneventfully after one month.
Discussion
Approximately 12-15% of the UK adult population have gallstones, with up to 4% becoming symptomatic every year. [1] More than 45,000 cholecystectomies are performed annually in the UK. Since the advent of laparoscopic cholecystectomy in the 1990s, it has become the gold standard for the management of symptomatic cholelithiasis. Large cohort studies have reported complication rates of 2-6% following laparoscopic cholecystectomy. [2] These complications include haemorrhage, gallbladder perforation, common bile duct injuries and conversion to an open procedure. Other risks include a subhepatic abscess, iatrogenic bile duct injury and choledocholithiasis postoperatively. [3] Bleeding occurs in <1%. [2] The anatomical sites most commonly affected include the gallbladder bed after its removal, sites of introduction of trocars, the cystic artery, falciform ligament and haemorrhage from a ruptured liver capsule. [2] In the open cholecystectomy era, cystic duct stump leaks were rarely reported. In the era of LC, improper clip placement, spontaneous clip displacement, ischaemic necrosis and elevated common bile duct pressures have been implicated as the cause, occurring in 0.12% of cases. Cystic duct stump leaks can be prevented by a high index of suspicion for postoperative complications and by prompt and appropriate intervention.
A subcapsular liver haematoma, described as a blood collection under the Glisson capsule is an extremely rare, life-threatening complication after laparoscopic cholecystectomy, with only a few cases reported in the literature. [4] Spontaneous haemorrhage of liver parenchyma following normal manipulation of the gallbladder and liver intraoperatively has also been described. This traction may be adequate to cause haemorrhage of a vulnerable haemangioma or surrounding liver parenchyma. It may occur early [up to 24 hours after surgery], presenting with acute onset upper right quadrant pain and hypovolaemic shock if the liver capsule has ruptured. Peritonism may be elicited on physical examination. It can also occur several weeks after the operation presenting with non-specific abdominal pain and a fluid collection on USS. An infected haematoma may present with pyrexia, abdominal pain and sepsis. Bacterial translocation from the gut is thought to be the cause of this superimposed infection. [5] It also occurs in <2% of pregnancies complicated by HELLP Syndrome [haemolysis, elevated liver enzymes and low platelets] and pre-eclampsia. It is also associated with trauma from a difficult labour or a breech presentation, hypoxia, coagulopathies, maternal diseases and placental lesions. In a neonate, it may present with poor feeding, listlessness, pallor, jaundice, tachypnoea and tachycardia. Other causes may include amyloidosis, rupture of hepatocellular carcinoma, adenoma, focal nodular hyperplasia or a haemorrhagic cyst. It is also a rare complication after endoscopic retrograde cholangiopancreatography [ERCP] with a paucity of cases in the literature. Iatrogenic puncture of a peripheral intrahepatic biliary tree resulting in laceration of small parenchymal vessels by an endoscopic guide wire may explain this phenomenon. [6] Acute onset of abdominal pain associated with hypotension and tachycardia after ERCP should raise the clinical suspicion of intrahepatic bleeding with Glisson’s capsule distension. Acute fascioliasis, a food-borne transmitted zoonosis caused by the liver trematode F. hepatica can manifest with a subcapsular liver haematoma, resulting from destruction of blood vessels during the intra hepatic migration of the immature parasites. Other risk factors for its development include the use of diclofenac, aspirin and ketorolac, a non-steroidal anti-inflammatory injection used for perioperative pain management. [7] Intra-operatively, the capsule of the liver can be damaged when dissecting off the gallbladder. Liver traction should be minimized through careful trocar placement while still allowing a critical view of safety to prevent visceral injury. A hepatic haemangioma has also been suggested as an aetiological risk factor. Anatomical variations involving the hepatic vascular system occurring in 12% of individuals, may result in slow bleeding post operatively. [8] Furthermore, the presence of a pseudoaneurysm is considered a risk factor. They have also been described after a liver biopsy, trauma to the abdomen and following the oral contraceptive pill. [9] CT is the investigation of choice for evaluating liver trauma as it has a high sensitivity [95%] and specificity [99%] for detecting liver injuries. [10] Abdominal ultrasound can also help to delineate the lesion, rule out a rupture and aid in serial follow up.
Displacement of a surgical clip from the cystic duct stump should also be considered in the differential diagnosis in patients presenting with haemorrhagic shock following a cholecystectomy. It has become common practice to place at least 2 clips on the proximal side of the cystic duct [CD] for insurance. Despite this practice, there are numerous reports of laparotomies in which a clipless CD has been identified as the cause of a patient’s bile peritonitis. [11][12] Necrosis of the CD stump proximal to the applied clips has also been reported as a cause of a cystic duct stump leak. Ischaemic necrosis caused by devascularization of the CD has also been implicated. [13] It has also been hypothesized that retained common bile duct stones can lead to excess pressure in the biliary tree leading to either perforation of the CD or displacement of the surgical clips. The average time to detection of a CDSL is 3-4 days post operatively. Individuals present with right upper quadrant abdominal pain [80%], nausea or vomiting [35%] and pyrexia [30%]. A leucocytosis is described in 70%. [14] The most successful imaging modality for correctly diagnosing CDSLs is ERCP, followed by MRCP. Endoscopic retrograde cholangiopancreatography is also the primary treatment modality in most postoperative biliary leaks, diminishing delay in therapy once the diagnosis has been confirmed. If a CDSL is found, a sphincterotomy should be performed and a stent placed, with care taken to evaluate for retained CBD stones. Radiologically guided drainage of the biloma has also been used in treating CDSLs. Percutaneous transhepatic biliary drainage has been demonstrated to be effective in CDSLs in small series. [15] The majority of cystic duct stump leaks heal spontaneously when bile is shunted past the defect. Percutaneous or endoscopic coil embolization, fibrin glue, and gelatin sponge injection are alternative approaches for refractory cases. Immediate development of a subscapular haematoma is a potentially life-threatening event due to hypovolaemic shock. Urgent evacuation of the haematoma using percutaneous drainage under ultra-sound guidance may be required. A relaparotomy or re-laparoscopy is required in haemodynamically unstable patients. In cases of a small haematoma in a stable patient, conservative management is appropriate. Treatment with broad spectrum antibiotics is initiated in cases of an infected haematoma. Although subcapsular haematoma is a very rare occurrence following a laparoscopic cholecystectomy it should be considered in the differential diagnosis in patients presenting with abdominal pain and signs of shock. A prompt diagnosis is required to prevent morbidity and mortality.
References
- Gill MS et al. Cholecystectomy audit: waiting time, readmissions and complications. Gut, 2015, 64 [S1], A402.
- De Castro SM, Reekers JA, Dwars BJ. Delayed intrahepatic subcapsular haematoma after laparoscopic cholecystectomy. Clin Imaging, 2012, 36: 629-31.
- Duca S, Bala O, Al-Hajjar N, Lancu C, Puia JC, Munteanu D et al. Laparoscopic Cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations.
- Liu QF, Bian LL, Sun MQ, Zhang RH, Wang WB, Li YN et al. A rare intrahepatic subcapsular haematoma: a case report and literature review. BMC Surgery, 2019, 19:3.
- Shea JA, Healey MJ, Berlin JA et al. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg 1996, 224:609-20.
- Orellana F, Irarrazaval J, Galindo J, Balbontin P, Manríquez L, Plass R et al. Subcapsular hepatic hematoma post ERCP: a rare or an underdiagnosed complication? Endoscopy, 2012;44, Suppl. 2.
- Vuilleumier H, Halkic N. Ruptured subcapsular haematoma after laparoscopic cholecystectomy attributed to ketorolac-induced coagulopathy. Surg Endosc 2003,17; 659.
- Duric B, Ignjatovic D, Zivanoic V. New aspects in laparoscopic cystic artery anatomy. Acta Chir Iugosl, 2000: 47: 105-7.
- Davis TJ, Berk RN. Benign hepatic lesions in women taking oral contraceptives. Gastrointst, Radiol, 1977, 2, 213-219.
- Ahmed N, Vernick JJ. Management of liver trauma in adults. J Emerg Trauma Shock. 2011;4 [1]: 114-9.
- Hanazaki K, Igarashi J, Sodeyama H, Matsuda Y. Bile leakage resulting from clip displacement of the cystic duct stump: a potential pitfall of laparoscopic cholecystectomy.Surg Endosc. 1999;13(2):168-171.
- Li JH, Liu HT. Diagnosis and management of cystic duct leakage after laparoscopic cholecystectomy: report of 3 cases. Hepatobiliary Pancreat Dis Int. 2005; 4(1):147-151.
- Journe´ S, De Simone P, Laureys M, Le Moine O, Gelin M, Closset J. Right hepatic artery pseudoaneurysm and cystic duct leak after laparoscopic cholecystectomy. Surg Endosc. 2004;18(3):554-556.
- Wise Unger S, Glick GL, Landeros M. Cystic duct leak after laparoscopic cholecystectomy: a multi-institutional study. Surg Endosc. 1996;10(12):1189-1193.
- Cozzi G, Severini A, Civelli E, et al. Percutaneous transhepatic biliary drainage in the management of postsurgical biliary leaks in patients with nondilated intrahepatic bile ducts.Cardiovasc Intervent Radiol. 2006;29(3):380-388
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse6
Matthew Flynn CT2 Surgical Department Mater Infirmorum, Belfast
Samuel Lakey Medical Student, Queens University Belfast
David Dick Specialist Registrar Antrim Area Hospital
Correspondence
Mr Matthew Flynn, ENT Department Craigavon Area Hospital, 68 Lurgan Rd, Portadown, Craigavon BT63 5QQ Email: Matthew.Flynn@southerntrust.hscni.net
Keywords: Operation notes, Documentation, Day Case, Surgical procedures
Conflict of Interests: No conflict of interests or sources of funding to disclose.
Abstract
Aims: Good operation notes are a key component of “Good Surgical Practice,” where specificity can help future treating clinicians and in medico-legal cases. This audit aimed to improve the quality of operation notes against standards set by the Royal College of Surgeons (RCS) in Good Surgical Practice (2014).
Methods: Retrospective review of case notes in a day case procedure unit dealing with local anaesthetic excisions. Change of practice was achieved by dissemination of preliminary audit results, introduction of a checklist at the point of operation note completion and education of relevant clinicians. The audit was repeated following intervention.
Results: Recording of procedure time rose from 0% to 100%, logging of operative findings and operative diagnosis improved from 80% to 100% and a detailed postoperative note from 60% to 94%. Date, name of procedure, closure technique and signature were recorded 100% of the time in both rounds of analysis.
Conclusion: Education and efficient record prompts lead to improvement over time in operation notes, demanding systemic reform of standard proformae currently in use. Further longitudinal studies could be done to determine if the improvement is sustained over time.
Introduction
Medical record keeping has experienced increased scrutiny and quality improvement in recent years driven by increases in medicolegal claims[i], with a total increase from £0.44 billion to £1.98 billion of claims costs between 2006-07 and 2016-17 within the UK[ii]. Procedure records should include site and side where applicable, and the use of diagrams is recommended[iii]. The RCS Good Surgical Practice (GSP) document outlined 18 criteria to be recorded during each operative procedure ranging from date to signature. When well done, these allow another clinician to “assess the care of the patient at any time[iv]”. Such guidelines provide a reference point for local audit and a skeleton for new operation note proformae[v][vi]. This audit aimed to snapshoot the faithfulness with which general surgical day case procedures were recorded in an urban acute hospital, and further outline challenges and learning points to sustain rigour and accuracy.
Methods
Retrospective review of 20 then 17 case notes in 2 separate phases was undertaken from March to July 2018. All were elective day procedure cases under local anaesthetic; predominantly excision of skin lesions. All notes were hand written on a standardized day surgery booklet. A modified list of 10 of the original 18 criteria from good surgical practice were checked for, and any comment addressing these fields were considered sufficient, with the exception of “Detailed operative instructions” were there had to be at least a 2-point plan postoperatively.
The findings of the first collection of data and the guidelines were discussed with all members of the team before the second cycle was commenced. For consistency the operation note proforma was not changed in the interim, but clinicians attempted to meet the standard while working within the existing proforma with an RCS checklist as a guide available at point of writing.
Results
Operations were carried out on 21 men (57%) and 16 (43%) women by 2 registrars, 4 Senior House Officers and 1 foundation doctor.
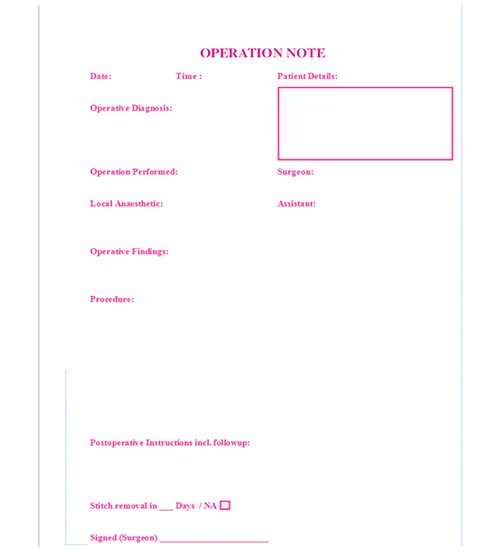
Discussion
Dissemination of the guidelines and aide-memoire led to an improvement in detail. Lack of recording of time of surgery on the operation note itself was significantly improved, but may have been originally recorded elsewhere in the proforma. The operative findings, alterations in tissue and postoperative instructions, are inexhaustible sections of the operation note at any time, but saw notable improvement. The improvement in postoperative care directives betrayed a level of pre-existent clinical thoroughness awaiting more detailed transcription. Potential causes include mental and motivational fatigue (all procedures were carried out after 2pm on a Friday afternoon), an outdated proforma, lack of legibility in some cases and human error. Argument could be and has been made for an electronic record with mandatory fields completed before the document can be saved[vii], however in this approach clinicians suffer the same fatigue as in hand-written notes and without the option to draw diagrams, diagrams which may encompass as many as 5 of this audits’ 10 data points. It is also to be noted that a discharge letter of the entire episode was dictated shortly after, and may have included some otherwise omitted details whilst denoting a time of completion. Overall improvement given correct written prompts led to a redesign of the surgical proforma, with less overall fields and operative diagnosis, details of local anaesthetic and a stitch removal prompt added. The proforma was also reduced from an 8 to a 4 page booklet to consolidate the focus of salient points against fatigue.
Figure 1. Revision of Good Surgical Practice Criteria for Purpose of Audit.
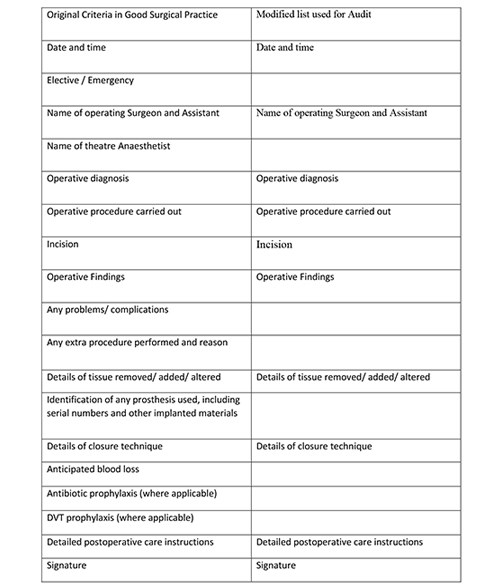
Figure 2. Percentage recording of key operation note findings by category.
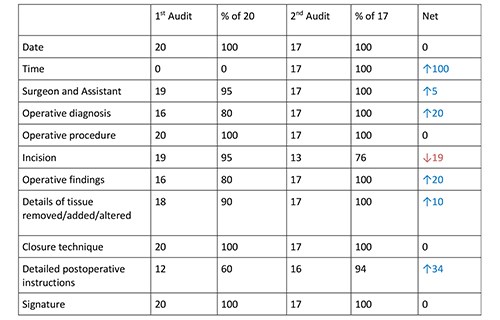
Fig 3 Graphical representation of percentage recording of key operation note findings by category.
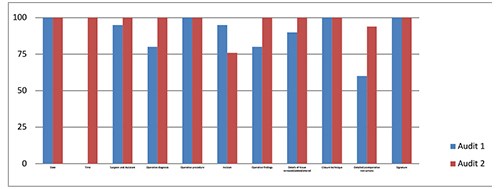
Fig 4 Day Procedure Proforma Redesign.
References
[i] Medical Defence Union Good Practice 2013;1(Vol4);19 Available from: https://www.themdu.com/guidance-and-advice/journals/good-practice-june-2013/increase-in-claims-costs accessed 4/7/19
[ii] National Audit Office. Managing the costs of clinical negligence in trusts HC: 305, 2017-19; 2.2
[iii] Academy of Medical Royal Colleges. Standards for the clinical structure and content of patient records London: HSCIC 2013;16
[iv] General Medical Council. Good Medical Practice 2013;19-21
[v] R. Din, D. Jena, B. N. Muddu, and D. Jennna The use of an aide-memoire to improve the quality of operation notes in an orthopaedic unit. Ann R Coll Surg Engl. 2001 Sep; 83(5): 319–320. PMID: 11806555
[vi] McGregor-Riley J, Ali F, Al Hussainy H, Sukumar S. Proformas can improve the quality of orthopaedic operation notes. J Bone Joint Surg Br 2003; 85 (Supp II):124. PMID 19102825
[vii]Coughlan F, Ellanti P, Moriarty A, McAuley N, Hogan N. Improving the Standard of Orthopaedic Operation Documentation Using Typed Proforma Operation Notes: A Completed Audit Loop Cureus. 2017 Mar; 9(3): e1084. Published online 2017 Mar 7. doi: 10.7759/cureus.1084 PMID: 28405534
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/30716/29-4-flynn.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse7
General Guidelines
The Journal of One-day Surgery considers all articles of relevance to day and short stay surgery. Articles may be in the form of original research, review papers, audits, service improvement reports, case reports, case series, practice development and letters to the editor. Research projects must clearly state that ethics committee approval was sought where appropriate and that patients gave their consent to be included. Patients must not be identifiable unless their written consent has been obtained. If your work was conducted in the UK and you are unsure as to whether it is considered as research requiring approval from an NHS Research Ethics Committee (REC), please consult the NHS Health Research Authority decision tool at http://www.hra-decisiontools.org.uk/ethics/.
Articles should be prepared as Microsoft Word documents with standard line spacing and normal margins. Submissions must be sent by email to the address below.
Copyright transfer agreement and submission
As of 7th November 2019, the JODS copyright transfer agreement must be downloaded from the resources section (tab) via the BADS website:
https://daysurgeryuk.net/en/resources/documentation/
Each named author should complete and sign a copy. Scanned copies/legible photos should be sent via email together with the main manuscript to the JODS editor: davidbunting@nhs.net
Any source of funding should be declared and authors should also disclose any possible conflict of interest that might be relevant to their article.
Submissions are subject to peer review. Proofs will not normally be sent to authors and reprints are not available.
Manuscript preparation
Title Page
The first page should list all authors (including their first names), their job titles, the hospital(s) or unit(s) from where the work originates and should give a current contact address for the corresponding author.
The author should provide three or four keywords describing their article, which should be as informative as possible.
Abstract
An abstract of 250 words maximum summarising the manuscript should be provided and structured as follows: Introduction, Methods, Results, Conclusions.
Main article structure
Manuscripts should be divided into the following sections: Introduction, Methods, Results, Discussion and References. Tables and figures should follow, with each on a separate page. Each table and figure should be accompanied by a legend that should be sufficiently informative as to allow it to be interpreted without reference to the main text.
All figures and graphs are reformatted to the standard style of the journal. If a manuscript includes such submission, particularly if exported from a spreadsheet (for example Microsoft Excel), a copy of the original data (or numbers) would assist the editorial process.
Copies of original photographs, as a JPEG or TIFF file, should be included as a separate enclosure, rather than embedding pictures within the text of the manuscript.
Tables, Figures and Graphs
Please submit any figures, graphs and images as separately attached files rather than embedding non-word files into the word manuscript document. Tables constructed in MS Word can be left in their original MS Word file including the manuscript if this is where they were drawn.
Figures and graphs can be presented in colour but try to avoid 3-d effects, shading etc. Figures and graphs may be redrawn if the quality is not in keeping with the Journal. Please make it clear within the manuscript text where you would like tables, graphs or images to be placed in the finished article with the use of a brief explanatory legend in the manuscript file where you wish the item to be placed, e.g.
Table 1. Patient demographic details.
Figure 1. Proportion of procedures performed as a day-case each year between 2005 and 2018.
Photographs
Photographs can be provided as jpg or tiff files but should be included as a separate enclosure, rather than embedded within the text of the manuscript. This ensures higher quality images. However, we will accept images within Word documents but image quality might suffer!
References
Please follow the Vancouver referencing style:
- References in the reference list should be cited numerically in the order in which they appear in the text using Arabic numerals, e.g. 1, 2, 3, 4 etc.
- The reference list should appear at the end of the paper. Begin your reference list on a new page and title it 'References.'
- Cite articles in the manuscript text using numbers in parentheses and the end of phrases or sentences, e.g. (1,2)
- Abbreviate journal titles in the style used in the NLM Catalogue: https://www.ncbi.nlm.nih.gov/nlmcatalog?Db=journals&Cmd=DetailsSearch&Term=currentlyindexed%5BAll%5D
- The reference list should include all and only those references you have cited in the text. (However, do not include unpublished items such as correspondence).
- Check the reference details against the actual source - you are indicating that you have read a source when you cite it.
- Be consistent with your referencing style across the document.
Example of reference list:
- Ravikumar R, Williams J. The operative management of gallstone ileus. Ann R Coll Surg Engl 2010;92:279–281.
- Dybvig DD, Dybvig M. Det tenkende mennesket. Filosofi- og vitenskapshistorie med vitenskapsteori. 2nd ed. Trondheim: Tapir akademisk forlag; 2003.
- Beizer JL, Timiras ML. Pharmacology and drug management in the elderly. In: Timiras PS, editor. Physiological basis of aging and geriatrics. 2nd ed. Boca Raton: CRC Press; 1994. p. 279-84.
- Kwan I, Mapstone J. Visibility aids for pedestrians and cyclists: a systematic review of randomised controlled trials. Accid Anal Prev. 2004;36(3):305-12.
- Barton CA, McKenzie DP, Walters EH, et al. Interactions between psychosocial problems and management of asthma: who is at risk of dying? J Asthma [serial on the Internet]. 2005 [cited 2005 Jun 30];42(4):249-56. Available from: http://www.tandf.co.uk/journals/.
Mr David Bunting
Editor, Journal of One Day Surgery
Consultant Upper GI Surgeon
North Devon District Hospital
[These guidelines were last revised on 02.11.2019]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/34945/author-guidelines.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse8

It was with great sadness that we learnt of the death of our colleague and friend Lawrence Rowe after an illness which he faced with typical stoicism and courage. Lawrence was a consultant anaesthetist in Norwich where he was greatly valued by his colleagues as someone who was always calm in any crisis, which was particularly appreciated in obstetric anaesthetics which he undertook for most of his career. He was endlessly patient and kind and many trainees benefited from his wisdom and excellent teaching. He was an earlier adopter of totally intravenous anaesthesia (TIVA), member of the Society for Intravenous Anaesthesia (SIVA) and an enthusiast for day surgery. He worked with David Ralphs, a former BADS president to ensure Norfolk and Norwich was at the forefront of developments in day surgery, introducing electronic records for anaesthesia more than 20 years ago. He also supported the purchase of TIVA pumps and was able to teach even the most tech-phobic anaesthetists (such as myself) how to use them!
He was an expert in IT and was generous with his time and skills as an ex- officio member of BADS council for over 10 years for which BADS is enormously grateful. He was webmaster for BADS and also designed a bespoke system for managing submissions and scoring abstracts for the Annual Scientific meeting. The marking process could seem daunting to those of us who volunteered for the job, but typically Lawrence added an important step to the instructions for marking, “pour yourself a glass of wine”; this was an indication of Lawrence’s approach to life, which was to have fun and make the most of every opportunity.
He was a keen sailor and loved sailing his river cruiser on the Norfolk Broads; he was an excellent pianist, had a pilot’s licence and built his own sports car. Since retiring he was able to enjoy travelling with his wife Lindsay who was a great support during his illness; he attended all three of his children’s graduations and was immensely proud of them. Despite becoming ill just before he retired, Lawrence reflected that he had done all he could have hoped for in his life and had no regrets.
Anna Lipp
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/30718/29-4-rowe.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse9
Adam Kimble

Adam is a Consultant General & Colorectal Surgeon at Torbay in South Devon. He was an undergraduate at Guy’s & St Thomas’s Hospitals Medical School, London. His postgraduate training took him along the south coast of England from Hastings to Truro as well as time spent in Australia and demonstrating anatomy in Brighton. His higher specialist training was in the South West, combined with a period of research into perioperative medicine after major abdominal surgery. His post-CCT Fellowship was in laparoscopic rectal surgery at St Richard’s Hospital in Chichester. His clinical interests are laparoscopic colorectal surgery, transanal surgery including TaTME and TAMIS, and day-case pilonidal and haemorrhoidal surgery.
Adam is the new Treasurer of BADS.
Dr Stamatios Karavolos BSc MBBS MD MRCOG

Dr Stam Karavolos is a Consultant Gynaecologist based at Salford Royal Hospital, Greater Manchester. He has a special interest in reproductive surgery and ambulatory gynaecology. He graduated from the Royal Free and University College Medical School, London, in 2004 and completed his training in obstetrics, gynaecology and reproductive medicine in London and Newcastle. He was awarded a postgraduate research degree (Doctor of Medicine) from Newcastle University in 2016.
He is actively involved in both undergraduate and postgraduate education and holds a position as an Honorary Senior Lecturer at the University of Manchester. He has published a number of scientific papers and has been a speaker in national and international medical meetings. He is currently involved in national policy making as a member of the Royal College of Obstetricians and Gynaecologists (RCOG) guidelines committee and RCOG clinical assurance group
Karen Harries

Karen is an Australian trained Registered Nurse who has been in the UK since 1995. She currently the Lead Nurse for Day surgery and Pre-operative assessment at Kings College Hospital NHS Foundation Trust based at Denmark Hill, a role she has held for the past 2 years. Karen has worked in a range of day surgery/23 hour and theatre settings for the past 20 years and is passionate about educating and empowering day surgery nurses to be knowledgeable and expert in their extended role. Karen is delighted to have joined BADs council and to be involved in driving and promoting the profile and importance of day surgery at more than just a local level.
Shaun Clee

An experienced Chief Executive and Chair with a successful track record of significant National and Regional leadership roles. Shaun possesses excellent communication skills, is a seasoned interviewer for Executive roles and has a track record of setting demanding objectives and inspiring people to achieve these.
His ability to read the broader operating environment, political astuteness and people skills have created numerous productive partnerships which continue to deliver enhanced results and business growth in complex and challenging environments.
Considerable strategic and operational management experience results in his ability to visibly lead large scale service and cultural change that inspires staff ownership and pride in the organisation.
Experience
- 11 years as an NHSFT Chief Executive Officer, establishing and leading a successful NHS Foundation Trusts.
- 16 years NHS Executive Board experience in complex health environment.
- Clear grasp of the strategic agenda for Health and Social Care,
- Successful regional leadership having created and led a collaborative between 7 Trusts in the South West of England, the Institute for Healthcare improvement in Boston Massachusetts and the South West Strategic Health Authority substantially improving the quality of services to 5 million people. Expanded this programme to cover the entire South of England, doubled the size of membership organisations and brokered a partnership between 5 Academic Health Science Networks to fund the programme.
- Ambassador and Board member for NHS Benchmarking Network April 201 –2018
- Elected to the NHS Confederation’s National Mental Health Network Board in 2009, became Deputy Chair in 2010 and Chair of the National Network Board from July 2011 – 2015 playing an active role in shaping the provider landscape of the future whilst growing membership market share from 60% to 96% of providers in membership.
- Elected as Trustee and Corporate Board member of the NHS Confederation 2011.
- Became Senior Independent Director of NHS Confederation in April 2015 and led the recruitment of the Right Honourable Stephen Dorrell as Chair.
Richard Parkinson

- School education: St Peter’s School, York then Victoria University of Manchester.
- Post graduate education: North West training scheme including Wrightington Hospital.
- Overseas trauma fellowship: Harbour view Medical Centre Seattle USA
- Knee fellowship: Melbourne Australia with John Bartlett
- Sports medicine fellowship Birmingham Alabama USA
- Consultant appointment: Wirral University Teaching Hospital 1994 - present: special interest Knee
- BASK president 2014-2016
- BOA Council Trustee 2017-2019
- Beyond Compliance and ODEP committee member 2013 -present
- Hobbies: Golf, ornithology, fell walking, travel and all things Yorkshire
Edward Dunstan MB BS BSc FRCS (T&O)

- Consultant NHS Fife 2007-date
- Director of Surgery NHS Fife 2016-2019
- Chair Day Surgery Working Group NHS Fife 2016-2019
- Chair Scottish Committee for Orthopaedics and Trauma 2016-date
- Clinical Lead ERAS NHS Fife 2008-date
- Clinical Lead South East Scotland Trauma Network 2017-date
- Council British Orthopaedic Association 2016-date
- T&O Consultant
- Appraisal Tutor NES Scotland
- Appraisal Lead NHS Fife (acute services)
- Chair: Scottish Committee for Orthopaedics and Trauma
I have a specific interest in Day Case Hip Replacements and after visiting Copenhagen in August 2018 set up a programme in Fife leading to the first successful planned Day Case replacement being performed in Scotland in November of that year. Since then we have hosted several visits from other Health Boards to learn the technique and offer support and guidance.
Recent Presentations
- Day Case Hip Replacement Surgery, BADS, Edinburgh 14/3/19
- Day Case Hip Replacement Surgery, Healthcare Conferences UK, London 5/4/19
- Day Case Hip Replacement Surgery, The Ripple Effect, QIST, London 30/4/19
I believe I have much to offer the council of BADS, especially from an Orthopaedic perspective, when it comes to ERAS together with driving and spreading the best practice that is Day Surgery for the benefit of patients.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/30729/29-4-new-council-members.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse10
Adam Kimble, Consultant Colorectal & General Surgeon, Torbay & South Devon NHS Foundation Trust
Thursday 9th May saw the 2019 joint British Association of Day Surgery (BADS) and Healthcare Conferences UK (HCUK) one-day conference “Developing your Daycase General Surgery Service”. Hosted in the De Vere West One Conference Centre, in central London, it saw delegates and presenters from across the UK from diverse clinical backgrounds relevant to day case and short stay General Surgery for what promised to be a stimulating and informative day.
The meeting was formally opened by Miss Vanessa Cubas, BADS Council Co-opted Association of Surgeons in Training Member, who introduced the first session’s presenters Dr Jane Montgomery, Consultant Anaesthetist from Torbay and BADS Treasurer, who stepped in last minute when BADS President, Dr Mary Stocker was delayed travelling up from Devon. Dr Montgomery gave a comprehensive overview of the day surgery pathway from GP referral to discharge from hospital and recovery at home, including appropriate patient selection. Importance was placed on dedicated facilities separate from inpatient beds to enable expertise to be developed in managing day case patients. Quality improvement, the theme of the day, was introduced as a way of widening the inclusion criteria for day case surgery including those who live alone, the older population, the obese, and more complex surgical procedures. It was also an opportunity to introduce the new Fifth Edition of the BADS Directory of Procedures.
The next part of the first session expanded upon the assertion made by Dr Montgomery that the day case pathway actually starts at (or indeed before) referral from primary care. This part was shared between Professor Gerard Danjoux, Consultant Anaesthetist from South Tees Hospitals NHS Foundation Trust, and Edward Kunonga, the Director of Public Health for Middlesborough Council and was entitled “Prehabilitation and widening thepool for day case surgery”. They talked about the South Tees experience in developing and implementing a cross-sector community-based exercise prehabilitation programme piloted as the PREPWELL study. The premise of which was to improve the fitness of patients in preparation for surgery to improve their outcomes. This has predominantly been in high-risk surgical specialties, but they also outlined the North East’s plans for developing the programme to make it amenable to day case surgery. The key messages were of the effectiveness of collaborative and cross-sector working to achieve system change.
After coffee, Mr Doug Bowley, Head of the West Midlands Paediatric Surgery Network and Consultant Colorectal & General Surgery at the Heart of England NHS Foundation Trust, began the next session with a talk about children and day case general surgery. Mr Bowley explained that for a period of time in the UK there was a push for all paediatric surgery to be carried out by paediatric surgeons in tertiary centres. More recently, however, there has been a recognition that the majority of general paediatric surgery e.g. herniorrhaphy, orchidopexy and circumcision (which can be carried out as day case surgery) can be performed by accredited adult general and urological surgeons. He stressed that these paediatric patients, and their families, should receive high quality care provided locally, with no variation in practice. To underpin this practice requires the development of clinical networks with the appropriate training and education and the provision of child friendly facilities and pathways e.g. “play dates” in the day surgery unit to familiarize the child with what to expect on the day of surgery.
Just before lunch Professor Doug McWhinnie talked about emergency surgery day case pathways. Same Day Emergency Care (SDEC) is a hot topic currently within NHS England. The UK Government and the Royal Colleges have provided impetus to Trusts to improve patient safety and experience, and to improve efficiency for this cohort of patients. Prof McWhinnie defined Ambulatory Emergency Surgery as: “The management of an emergency patient according to an ambulatory pathway, avoiding overnight stay following their surgical procedure”. He showed evidence that by investing in dedicated emergency pathways, patients are seen and treated quicker, wth earlier and more senior input into their management. This enhances the patient experience, and offers hospitals increased efficiency of precious theatre and bed resources, but requires formal recognition and integration of these services to ensure sustainability.
Lunch was followed by a session on Upper GI surgery. Firstly, Mr David Bunting, Consultant Upper GI Surgeon from North Devon Hospital, Barnstaple talked about improving day case laparoscopic cholecystectomy rates and the North Devon experience with the Royal College of Surgeons’ Cholecystectomy Quality Improvement Collaborative (Chole-QuIC) project. Using QI methodology, and empowering teams locally, this initiative highlighted an impressive improvement in the treatment of acute biliary disease requiring surgical intervention. With a shift in North Devon to 71% of patients using an ambulatory care pathway and 47% of patients treated as a day case. This was followed by Mr Paul Super, Consultant Upper GI Surgeon from the Heart of England Foundation Trust in Birmingham talking about day case fundoplication and anti-reflux surgery. Nationally, the day case rate for anti-reflux surgery is about 15%, however the rate at Heartlands is in excess of 80%, with an overwhelmingly positive patient feedback. Mr Super outlined the patient pathway and general principles for day case hiatal surgery that have enabled the unit to achieve these impressive results.
The final session of the day was given by Professor Timothy Rockall, Consultant Colorectal and General Surgeon from the Royal Surrey County Hospital in Guildford. Professor Rockall presented the Guildford experience of 23-hour stay colorectal resection and its acceptability and safety in selected patients undergoing laparoscopic colectomy. Patients followed a modified enhanced recovery program, and of the 10 patients included, all were discharged within 23 hours from the commencement of surgery with no major complications and no readmissions and high patient satisfaction.
Overall the day covered all aspects of day case general surgery and provided all those who attended with food for thought, and no doubt inspiration, to take back to their own Trusts to enable them to improve their own service. A big thank you to all the speakers and all those involved in organizing a successful day conference, and to all the delegates who attended and contributed to the discussion on the day.
Due to excellent feedback from this meeting, it is being held once again in Birmingham on Tuesday 21st January 2020.
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1857#collapse11