Dave Bunting
I write this editorial for the third edition of JODS this year having enjoyed a very successful BADS conference held at the Royal Society of Medicine. You will find a full report of the event written by Fiona Belfield and this edition of the journal is accompanied by a supplementary edition publishing all abstracts presented at the conference. For those of you that missed out on attending the conference, you will be able to see some of the moments captured on camera in the images included in this edition. I would like to take this opportunity to thank all those attending the conference and especially those who submitted their work and presented this at the conference. I would like to remind authors that they are encouraged to submit their work for full publication in JODS subject to successful peer-review. Please see the guidelines for authors included in this publication and accessible via the BADS website here:
https://daysurgeryuk.net/en/resources/guidelines-for-authors/
Since the last edition of JODS, Mary Stocker has stepped down as President of the Association and I would like to take this opportunity to give a warm welcome to Dr Kim Russon who has taken up the position as of the conference in June. Over the past few years undertaken a huge amount of work for BADS including but not limited to conference organisation, hosting national meetings and representing BADs in working with a number of organisations. I am confident she will be able to continue to promote the day surgery agenda and build on the recent successes of the organisation.
After a very successful conference, BADS as an organisation is always keen to consider where we go from here. Plans for another very promising conference in Cardiff next year are already progressing well. The association continues to increase its involvement with benchmarking organisations and improvement initiatives such as the Model Hospital, Getting it right first time (GIRFT), NHS England Best Practice Tariffs, Public Health England and NHS Right Care. It also co-organises a number of regional and national educational events with organisations such as the Royal College of Anaesthetists and Health Care Conferences UK. Looking further to the future, we are investigating the potential role BADS may have in accreditation of Day Surgery Units across the UK.
This edition of JODS contains scientific articles on day case mastectomy, peri-operative gabapentin use in gynaecological day case surgery, day case management of resistant tennis elbow and a report on a service improvement project successfully expanding the scope of day case hand and wrist surgery.
Finally, dates for the annual conference next year have been confirmed, it will take place on 25th & 26th June 2020 in City Hall – why not put the dates in your diary now and book study leave!
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29235/291-editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse0

Kim Russon
As this is my first President’s letter I thought I would introduce myself: I am Kim Russon, Consultant Anaesthetist and Clinical Lead for Day Surgery at The Rotherham FT Hospital in South Yorkshire. It is an honour to have taken over as President of the British Association of Day Surgery at our conference in London in June of this year and I am grateful for the support and guidance of the current council and immediate past presidents, Mary Stocker and Anna Lipp
Joining the British Association of Day Surgery (BADS) council from September 2019 will be Shaun Clee, as a lay representative, Mr. Edward Dunstan, an orthopaedic surgeon from Fife, Mr. Adam Kimble, a colorectal surgeon from Torbay, Ms. Karen Harries, lead nurse for day surgery at King’s College Hospital. Welcome and thank you for giving your time to help the work of BADS.
BADS has been involved with progressing day surgery and excellence in short-stay surgery for over 30 years and we celebrated this at our recent conference with a Presidents’ plenary. I would like to thank all previous Presidents and council for the excellent work that has been achieved. You have left some big shoes to fill! The 6th Edition of the ‘Directory of Procedures’ was launched at 2019 conference along with the 4th edition of ‘Spinal Anaesthesia for Day Surgery Patients: A Practical Guide’. Both have seen significant changes since their first editions were published. Progress in day surgery would not be possible without the support of the BADS membership, for which we are very grateful.
The Royal Society of Medicine in London provided a fabulous venue for our 30th BADS Conference and with over 200 delegates from near and far (Switzerland and China to mention a few of our international delegates) in attendance there was a lively and enthusiastic feel to the conference. The programme was varied covering general surgery, gynaecology, benchmarking and going green in day surgery. For more details please read Fiona Belfield’s conference report. I would like to take this opportunity to thank all delegates and sponsors who attended the meeting and made it a very successful one. If you were unable to attend then, the filming of the lectures should be available in the members’ area of the BADS website very soon.
BADS continues to have a number of work streams and works collaboratively with other organisations
- Getting It Right First Time (GIRFT): BADS continues to build on our collaboration and the importance of day surgery has been recognised.
- NHS England Best Practice Tariffs: Liaison continues to advise which day case procedures should be considered for this.
- Royal College of Anaesthetists: Collaboration continues with regards to the curriculum and Quality Improvement /“Audit recipes”
- Health Care Conferences UK: 21st January 2020 Day case General surgery, Birmingham 27th February 2020 Day case Breast Surgery, London
- Northumbria QISIT - 15th October 2019, Newcastle
For more information about the study days, how to book and further resources, e.g. Presentations on day case topics from the Scottish Government meeting please go to our BADS’ website www.bads.co.uk. We hope you find the BADS’ website a useful resource. We intend to regularly add to the members’ area of the website. If you are not already a member of BADS I hope you will consider joining.
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse1
Emeka Ibem Kalu, Senior registrar, Olubusola Alagbe-Briggs, Consultant, Longinus Ndubuisi Ebirim, Consultant
Department of Anaesthesiology, University of Port Harcourt Teaching Hospital, Port Harcourt, Rivers State, Nigeria
Corresponding author: Dr L N Ebirim, Department of Anaesthesiology, University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria . Tel: +2348033384198 . Email: longinus.ebirim@uniport.edu.ng
Abstract
Introduction: Pre-emptive administration of oral gabapentin may cause a reduction in dose and side effects of analgesic agents needed to achieve adequate postoperative pain relief. This study was therefore aimed at determining if pre-emptive oral gabapentin can attenuate post-operative pain following day case gynaecological surgeries performed under general anaesthesia.
Methods: Fifty-six ASA I or II patients scheduled for day case gynaecological operations were recruited into this prospective, double-blinded study after obtaining informed consent from them. They were randomly allocated into two groups (GG and PG) of 28 patients each, to receive either 300mg of oral Gabapentin (GG) or Placebo capsules (PG) 2 hours before surgery.
The outcome assessed included time to first request for postoperative analgesia, pain intensity, analgesic consumption in the postoperative period before discharge as well as possible side effects.
Results: The time for first analgesic request was significantly prolonged in the Gabapentin group compared to the Placebo group. (p= 0.007). The mean VAS score was significantly lower in the GG than in the PG. (p= 0.001). The mean total dose of analgesic consumed during the study was significantly lower in the GG than in the PG, (p= 0.004). All patients in both groups were discharged between 8 and 10 hours after surgery. The proportions of patients that experienced nausea, vomiting and dizziness were similar in both groups.
Conclusion: Gabapentin 300 mg given orally 2 hours prior to surgery decreased postoperative analgesic requirements and prolonged the time to first rescue analgesic request with minimal side effects.
Keywords: Pre-emptive gabapentin, post-operative analgesia,
Introduction
Pain is defined by the International Association for the Study of Pain (IASP) as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or that can be described in terms of such damage.1
Pain management in day case surgical patients is a major concern to the surgeon and the anaesthetist and a multi-modal approach is ideal to achieve adequate pain control in this group of patients.2
Inadequately treated postoperative pain can lead to patient discomfort, sleep deprivation, prolonged hospital stays, unanticipated hospital readmission and increased costs.3
A day case patient is one who is admitted for a surgical procedure or investigation and discharged within 24 hours following adequate recovery from anaesthesia.4 Discharge criteria for day case patients include ability to sit unaided, achieve good pain relief with oral analgesics, walk in a straight line, ingest fluid and food without nausea and vomiting, as well as void urine.5
A study has shown that under-treatment of pain is common after day case surgery and about 30 - 40% of discharged out-patients may suffer from moderate to severe pain during the first 24 – 48 hours.6
Therefore, optimal post-operative pain control for day-case surgeries should be achieved using drugs with minimal side-effects that facilitate early recovery. For this reason, several pharmacological agents have been employed to control pain in day case patients.7
Opioids have been given by various routes for this purpose. However, the side effects of opioids like nausea, vomiting, and respiratory depression limit their usage and can delay discharge.8 Non-steroidal anti-inflammatory drugs are also being employed especially in the immediate post-operative periods but concerns are raised about their side effects like inhibition of cyclooxygenase which may lead to acute gastritis, stress ulcers and bleeding.9
Different mechanisms are involved in post-operative pain, such as sensitivity to nociceptors and inflammatory component. The process is created by pain receptors (nociceptors) which are sensitive to mechanical, chemical and heat stimulation. These generate nerve messages throughout the brain and spinal cord, leading to pain.10
Therefore, multimodal analgesic techniques utilizing a number of drugs acting on different analgesic mechanisms are becoming increasingly popular.11 Also, the concept of preventing the pain before it starts by desensitizing the central nervous system is being explored with the use of pre-emptive analgesia.
Some studies have been carried out on the use of oral gabapentin for pre-emptive analgesia,12,13 Gabapentin was found to have enhanced the analgesic effect of other pain-relieving agents as evidenced by increase in time to first request for analgesic postoperatively, there was also a significant reduction in total analgesic consumption in the first 24hours.
Commonly reported side effects of gabapentin include dizziness, sedation, ataxia, blurred vision and irritability.12 However, most of the adverse effects following the use of oral gabapentin are dose dependent. Hence, 300mg of oral gabapentin does not cause significant side effects as shown by Montazeri et al13
Some studies have shown that single dose 600mg as well as 300mg oral gabapentin attenuated post-operative pain14, 15 Few of these studies have been done in this sub-region especially in patients undergoing day case gynaecological surgeries. Therefore, oral gabapentin was evaluated for its pre-emptive analgesic efficacy on post-operative pain in patients undergoing day case gynaecological surgeries in this study.
Methods
This randomized, double-blinded, prospective study was carried out at the University of Port Harcourt Teaching Hospital (UPTH) from January 2017–June 2017.
The study population was drawn from patients aged between 20-50 years of ASA physical status I and II, scheduled for day case gynaecological surgeries under general anaesthesia. Excluded from the study were patients who refused to give consent, those who were morbidly obese and those with known allergy to gabapentin, opioids or tramadol. Also excluded were patients on gabapentin or analgesic usage 24 hours prior to surgery, those with chronic pain and those with history of seizures or psychiatric disorder.
Sample size calculation16 showed that a minimum of 50 participants were required for the study. Allowing 10% loss to protocol violation (attrition), a total of 56 patients approximately, 28 for each group were therefore entered for the study. Group I received 300mg of oral gabapentin two hours prior to surgery. Group II received oral placebo two hours prior to surgery.
Study protocol
Ethical clearance was obtained from the institutional Ethics and Research committee and. eligible patients were identified during the preoperative evaluation. The study was explained to them in a language they understood. Written consent was obtained from them. The patients were clinically assessed and fitness for the study verified. The method of pain assessment: using visual analogue scale (VAS) was explained to the patients. They were educated on the VAS which is a single line of 10cm with words at both ends: “no pain” and “worst pain” imaginable. Patients observed 6hours fast before the surgery.
Randomization
Using a balloting technique, with coded papers inside an envelope, the patients were randomly allocated into two groups, Group 1(GG) and Group 2 (PG). Patients in GG (n=28) received 300mg oral gabapentin (Neurontin) while those in PG (n=28) received oral placebo capsule (Astymin) all two hours before surgery.
The researcher who carried out the general anaesthesia procedure was blinded to the content of the envelope and the drug preparation (Neurontin capsule 300mg by Pfizer and matching placebo capsule, an inactive formulation similar to gabapentin in appearance (Astymin).
Study procedure
On the patient's arrival at the operating room a multi-parameter monitor's (Dash 4000; GE Medical System Information Technology International, Wisconsin USA) probes and cuff were attached. Baseline vital signs including heart rate (HR), systolic blood pressure (SPB), diastolic blood pressure (DBP), mean arterial blood pressure (MAP), arterial oxygen saturation (SPO2) and temperature (T°C) were taken and recorded. Electrocardiogram (ECG) monitoring was also established. Intravenous access was secured with 18-gauge cannula in the dorsum of the left hand and each patient was given 0.01mg/kg of midazolam, 0.004mg/kg of glycopyrrolate and 1mg/kg of tramadol pre-induction, all intravenously.
The patients were pre-oxygenated for 5 minutes and anaesthesia was induced with intravenous propofol 1.5mg/kg, while intravenous suxamethonium chloride 1.5mg/kg was given for muscle paralysis. Following adequate muscle relaxation, laryngoscopy was done, an appropriately sized cuffed orotracheal tube was passed, the cuff was inflated and the tube connected to the breathing circuit and anaesthetic machine. Correct tube placement was confirmed with auscultation and capnography. Anaesthesia was maintained with isoflurane (1% -1.5%) in 100% oxygen and muscle paralysis maintained with intravenous atracurium 0.5mg/kg. Non-invasive Blood Pressure, mean arterial Blood Pressure, Heart Rate and Arterial Oxygen Saturation were noted every 5minutes until the surgery was over. Fluid maintenance was achieved with 0.9% normal saline. All intravenous fluids were warmed to 37˚C to reduce the risk of hypothermia and shivering. At the end of the surgery, the residual muscle paralysis was reversed with intravenous neostigmine 0.05mg/kg and glycopyrrolate 0.008mg/kg to obtund its muscarinic effects. The trachea was extubated when the patients became conscious and able to obey commands. The duration of the surgery which is the time from knife on skin to the end of surgery (time of last stitch) was noted. Monitoring was continued post-operatively at the post- anaesthesia care unit where close monitoring of physiologic parameters; heart rate, blood pressure, temperature and respiratory rate was continued.
Patient's level of pain was assessed using the VAS. This was done when patient had recovered fully from anaesthesia as follows, when patient is conscious and obeys command (0hr), hourly for the first 2hours, and two-hourly for the next 4hours post-operatively. At the pain score of more than 3cm, rescue analgesia with intravenous tramadol 1mg/kg was given. Analgesia was maintained at home with 100mg oral tramadol given as required. The time for the first request for analgesia was noted. Occurrence of nausea, vomiting, dizziness, sedation, respiratory depression and other untoward effects among the treatment groups was also noted and recorded while patient was still on the ward and before discharge from hospital.
Patients with minimal or no side effects were discharged home between 8hrs to10hrs post-operatively, none of the patients reported any side effects at home.
The primary outcome was time to request for the first analgesia defined as the time interval from tracheal extubation to time of first analgesic request.
The secondary outcomes were: pain intensity assessed with VAS, the total dose of tramadol given within the first 24 hours after surgery and the side effects documented in the recovery room when patient was fully awake.
- Sedation was assessed in the PACU when the patient had recovered fully from general anaesthesia and graded according to the Ramsay sedation scale17 Sedation was reported as present with scores
- Respiratory depression was said to have occurred in patients in whom respiratory rate decreased to < 8 breaths per minute.
- Dizziness – This was assessed before patient was discharged from the ward using a four-point Likert verbal scale (none, mild, moderate and severe)
- Nausea and vomiting – This was graded on a four point ordinal scale (0–no nausea or vomiting.
1 = nausea but no vomiting. 2 = both nausea and vomiting present. 3 = more than two episodes of vomiting in 30 minutes
Data collection and analysis
Socio-demographic data and peri-operative events were recorded using the proforma.
Data analysis was done with SPSS Version 21. Data presentation included tables and charts. Data were tested for normality using Kolmogorov-Smirnov statistics. Normally distributed variables were summarized using means and standard deviation, and differences in means compared using independent t test while non-normally distributed variables were summarized as medians and non-parametric test of Mann-Whitney U test employed for comparing differences. Categorical variables were compared using Fisher’s exact test or Chi-square as appropriate. A P-value of <0.05 was considered statistically significant.
Results
A total of fifty-six females, aged between 20 and 50 years of ASA physical status I or II were enrolled into this study, with 28 patients in each group. Group I was the gabapentin group while group II was the placebo group. Fifty-six patients completed the study.
Both groups were comparable in terms of age, weight, height, BMI, and the duration of surgery as shown in Table I. The mean age of the patients in the gabapentin group was 35.18±5.76 years while in the placebo group, it was 33.75±5.26 years (p=0.337). The mean weight of patients in the gabapentin and placebo groups were 65.14±5.37kg and 64.46±4.95kg respectively (p=0.625). The mean height in the gabapentin group was 1.63±0.05 metres while in the placebo group, it was 1.64±0.06metres (p=0.890). The mean duration of surgery in the gabapentin group was 56.86±7.18minutes while it was 55.86±7.76minutes in the placebo group, (p=0.619).
Table I. Comparison of mean socio-demographic characteristics across groups in the study
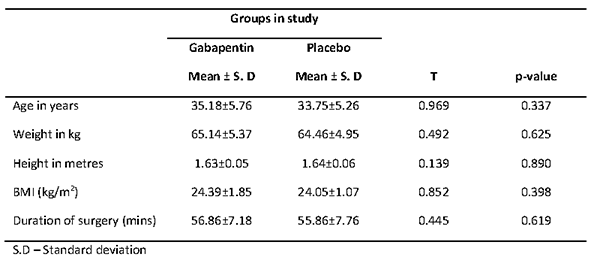
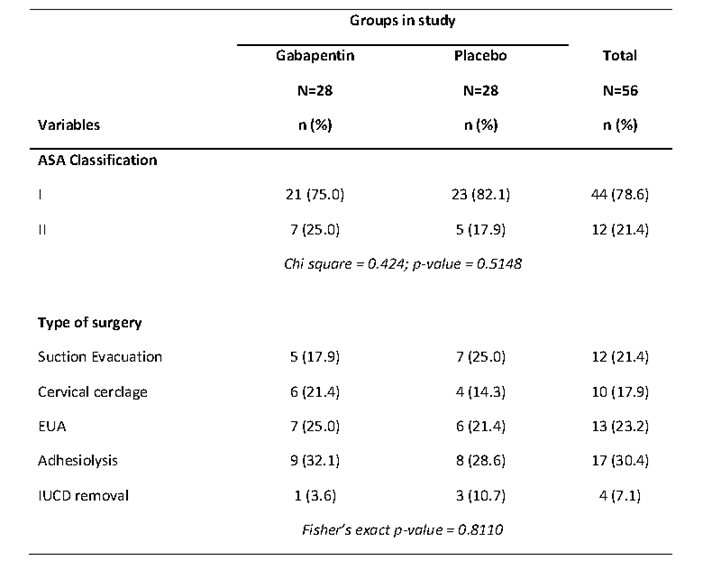
Table II shows the ASA classification and type of surgery across the groups in the study. Majority of the patients in both gabapentin (75.0%) and placebo (82.1%) groups were in ASA physical status I. There were no significant differences in proportions of ASA classification by the groups in the study (p=0.5148). The commonest surgery was adhesiolysis in both gabapentin (32.1%) and placebo (28.5%) groups. This was followed by EUA (25.0%) in the gabapentin group and suction evacuation (25.0%) in the control group. There were no significant differences in the proportions of type of surgery across the gabapentin and placebo groups (p=0.810).
Table II. ASA classification and type of surgery across groups in the study.
The intra-operative haemodynamic variables were stable and similar in both groups as shown in Figures 1 to 3. The differences in haemodynamic variables across groups were not significant (p>0.05). The oxygen saturation ranged between 96 to 100 % in both groups.
Figure 1: Line graph showing the mean systolic and mean diastolic blood pressure values of the
groups in the study during the intra-operative period.
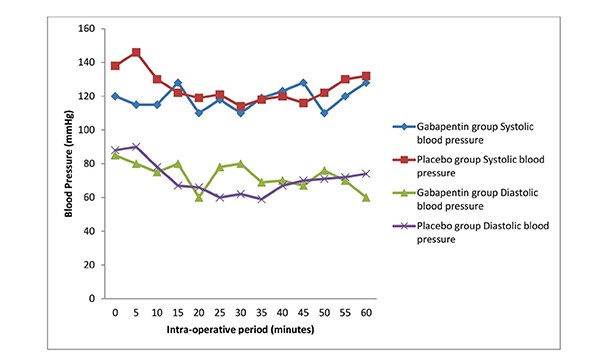
Figure 2: Line graph showing the mean heart rate values of the groups in the study during
the intra-operative period.
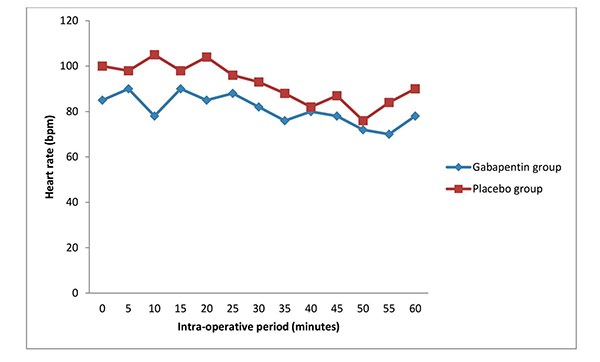
Figure 3: Line graph showing the mean SP02 of the groups in the study during the intra-operative period.
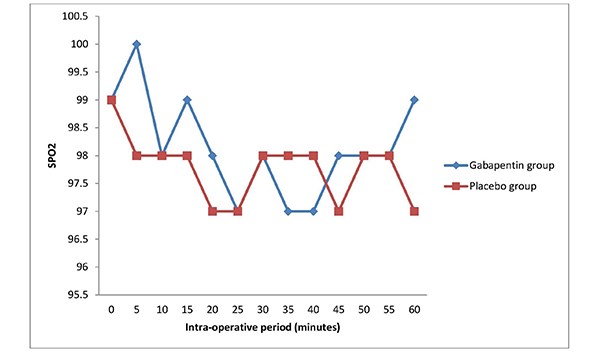
Table III (a) shows the comparison of the pain scores across the groups during the post-operative period. At time 0min (full recovery from anaesthesia and obeys command), the pain score was lower in the gabapentin group (mean score of 2.37) in comparison to the placebo group (mean score of 3.33). This difference in the pain scores was significant (p<0.05). The pain scores were also lower in the gabapentin group compared to the placebo group at 60mins, 120mins, 240mins, 360mins and 480mins respectively. The differences in the pain scores between the two groups were statistically significant (p<0.05) in most of the follow up postoperative periods.
Table III (a). Comparison of pain scores across groups in the study during the post-operative period.
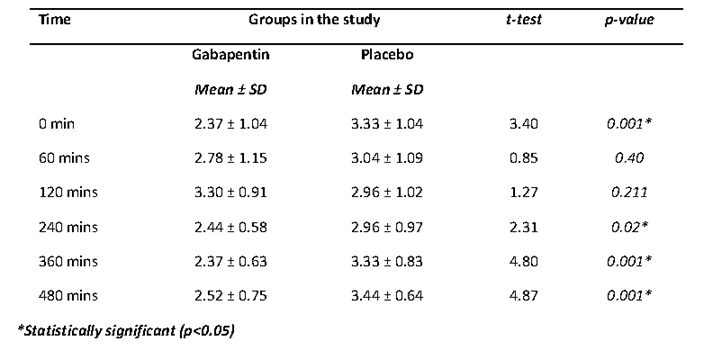
Table IV shows that the mean time of first analgesic request was prolonged in the gabapentin group (134.32±3.51minutes) compared to the placebo group (77.79±4.79minutes). The observed difference was statistically significant (p= 0.0001).
Table IV. Comparison of mean time to first request of rescue analgesia across groups in the study.
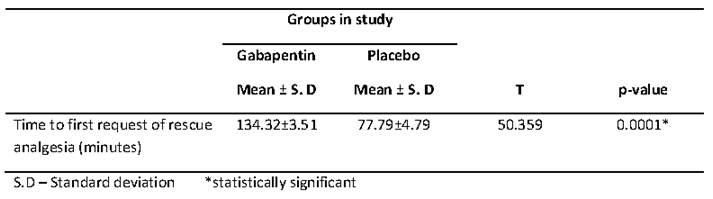
Figure 4 shows an error bar of the mean amount of opioids consumed by gabapentin and placebo groups. The mean total opioids (tramadol) consumed during the study was lower in the gabapentin group (130.8±6.4mg) in comparison to the placebo group (136.2±5.3mg). This difference in means was statistically significant (p= 0.004).
Figure 4. Error bar showing the mean amount of opioids consumed in gabapentin and placebo
groups in the study.
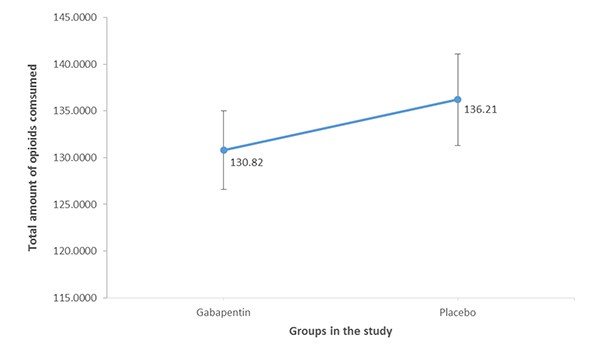
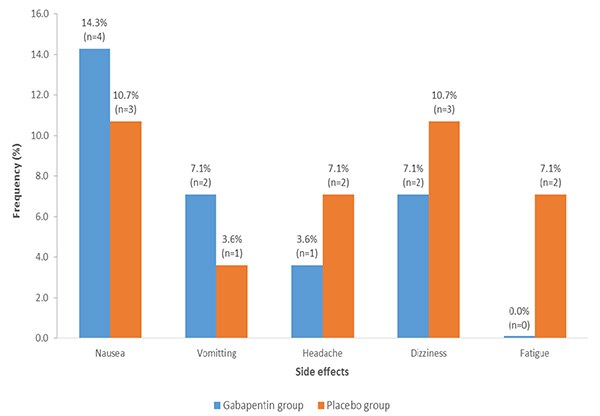
Figure 5 shows the frequency of side effects across the groups in the study. The frequency of nausea was higher in the gabapentin group (14.2%) when compared to the placebo group (10.7%). Higher proportion of the patients in the gabapentin had vomiting in comparison to the placebo group (7.1% vs 3.8%). All the patients with vomiting were treated with intravenous metoclopramide 10 mg and the vomiting resolved. Few patients complained of headache which resolved even before intervention within twenty minutes (1 patient in gabapentin group and 2 patients in the placebo group). There was also complaint of dizziness, though transient while patient was on the ward prior to discharge. The frequencies of dizziness in the gabapentin and placebo groups were 7.1% and 10.7% respectively. Fatigue was reported among 2 patients in the placebo group (7.1%), and none in the gabapentin group (0.0%).
Fig 5: Multiple bar charts showing the absolute and relative frequency of the side effects observed
in gabapentin and placebo groups.
All patients in both groups were discharged between 8 and 10 hours after surgery.
Table V shows the level of satisfaction between the two groups. In the gabapentin group, 32.1% (nine of the patients) reported excellent level of satisfaction as compared to 21.4% (six of the patients) in the placebo group The proportions of patients that reported their level of satisfaction as very good were 46.4% (13 patients) in the gabapentin group while it was 39.3% (11 patients) in the placebo group. The proportions of patients that reported their level of satisfaction as being good were 17.9% (five patients) and 32.1% (nine patients) in the gabapentin and placebo groups respectively. In the gabapentin group, 3.6% of the patients reported their level of satisfaction as being fair while in the placebo group, it was 7.1 % of the patients. There was no significant difference in the proportions of level of satisfaction across groups in the study (p = 0.5321).
Discussion
This study confirms that the oral administration of 300mg gabapentin prior to day case gynaecological procedures provided improved post-operative analgesic effect and prolonged the time to first request for analgesia with minimal side effects. It also demonstrated a reduction in the post-operative pain scores at different time points, and reduction in the total amount of analgesics required 24hours post-operatively in the gabapentin group when compared with the placebo group. These findings showed that pre-emptive oral gabapentin enhanced post-operative analgesia.
Both groups were comparable in terms of age, weight, height, intra-operative haemodynamic variables and duration of surgery. The ages and surgery durations were comparable in the studies done by Mardani-Kivi et al18 and Bafna et al14. In this study, the trends of heart rate mean systolic and diastolic blood pressures were similar between the two groups. The initial high values of pulse rates and systolic blood pressures noted in this study were probably due to anxiety, the values normalized as the surgery progressed. The finding of no significant haemodynamic variation between both groups in the study is similar to that of Bafna et al14, which revealed that gabapentin had no significant impact on the haemodynamic variables between the study group and the placebo group.
Various studies have shown that under treatment of pain following surgery is common; more than 30% of discharged post-operative patients suffer from moderate to severe pain within the first 48hours6 Luscombe et al19 conducted a study to compare the effect of parecoxib and placebo for pain management following day case gynaecological surgeries. The result showed that the study group had mild to moderate pain though the pain scores were lower in the study group compared to the placebo group.
The study by Liza et al17 titled; pain management in day case surgery, also noted that only 60% of patients undergoing minor gynaecological procedures including laparoscopic surgeries reported a satisfactory pain relief post operatively, more than 30% of the study population had mild to moderate pain post operatively which is similar to the findings in this study. To this end, the need for an effective pain control following minor gynaecological surgeries similar to the procedures in this study has been well demonstrated by the studies of Luscombe et al19 and Liza et al.17
This study showed that the pain scores using VAS were lower in the gabapentin group compared to the placebo group, this is similar to the findings in various studies done by Aryal et al20, Butt et al21, Dirks et al15 and Montazeri et al13 where the VAS scores were lower in the study groups than the placebo groups showing more evidence of the post-operative analgesic effect of gabapentin. In this study, the difference in the VAS scores between the two groups at the 10th hour post-operative period was not statistically significant, this may be attributed to the half-life of gabapentin which is 5-7hours.12 However, the exact median VAS score at the 10th hour post-operatively was lower in the gabapentin group compared to the placebo group. There was prolonged time to first analgesic request in the gabapentin group in comparison to the placebo group, which is in keeping with the study by Aryal et al20, which sought to evaluate the effect of gabapentin on post-operative analgesia with epidural morphine after abdominal hysterectomy. The finding of the index study also compares with studies by Hema et al22, Montazeri et al13 and Rajendran et al23 where there were findings of significant prolonged time to the request of first analgesia among gabapentin groups in comparison to groups without gabapentin. These studies along with present study further demonstrate that pre-emptive administration of oral gabapentin enhances post-operative analgesia.
This study revealed that the total analgesics consumed within 8hours post-operatively was significantly lower in the gabapentin group compared to the placebo group, which is consistent with findings by Dirks et al,15 who reported that there was 50% reduction in the morphine consumption 24 hour post-operatively in the gabapentin group. The findings by Aryal et al20, Mardani-Kivi et al18, Rajendran et al23 and Bafna et al14 were similar to that of this study where the reduction in the post-operative opioid consumption was significantly lower in the gabapentin group compared to the placebo groups.
The use of opioid analgesics for post-operative pain management has continued to attract concerns in view of the associated side effects.7 Therefore, the analgesic potentials of gabapentin for acute pain as demonstrated by the outlined studies23,18,14,20 and index study accounts for the reduction in the quantity of opioids to be consumed post-operatively with inherent reduction of the adverse effects of opioids.
Despite these studies23,18,14,20 that demonstrated a reduction in the consumption of opioids following pre-operative oral administration of gabapentin, a study by Panah et al24 refuted the finding as the authors noted that there was no significant decline in post-operative morphine consumption among the gabapentin group, compared to the placebo group. The study by Panah et al24 was done under spinal anaesthesia technique with bupivacaine as the local anesthetic agent.
The duration of action of bupivacaine is 2-8 hours25, this might have accounted for the contradictory findings by Panah et al24 amongst other factors. There were no side effects of gabapentin observed in the study by Panah et al24 when compared to this study where nausea, vomiting and dizziness were noted.
There were no significant differences in side effects observed between gabapentin and placebo groups in this present study. This is in contrast to the study by Jabalameli et al26 which recorded higher incidence of nausea and vomiting in the placebo group. This could have resulted from the anaesthetic technique used as hypotension following spinal anaesthesia can increase the incidence of nausea and vomiting. This present study was done under general anaesthesia thereby avoiding such a conflicting situation.
To the contrary also is the study by Mardani-kivi et al18 where the incidence of vomiting was similar in the three groups despite similar mode of anaesthesia as in this study. Cruz et al27 in a pilot study confirmed the role of gabapentin in the prevention and treatment of nausea and vomiting. The increase in the incidence of vomiting in this study may be due to the combined effect of gabapentin and tramadol drug-drug interaction (pharmacodynamics). It has also been found that vomiting is an uncommon side effect of gabapentin especially in children.28
Other side effects which the patients complained of were headache (1 in gabapentin group and 2 in placebo group) and dizziness, which is one of the commonest side effects of gabapentin28 (2 in gabapentin group and 3 in placebo group). Similar side effects were reported in a study by Bafna et al14 in which there were also no significant difference between the two groups in terms of side effects. The findings of this present study are similar to that of Dirks et al15 and Mardani-Kivi et al18 in respect to the observed side effects as there were no significant differences between the study groups and the placebo groups. Similarly, the studies by Panah et al24 and Rajendran et al23 revealed no significant side effects in both groups. This could have been as a result of the anaesthetic techniques used in the studies23,24. The studies23,24 were done under spinal anaesthesia which involved the use of only local anaesthetic agent unlike general anaesthesia that involves multiple drug usage.
This study revealed that no patient reported a low level of satisfaction with the use of gabapentin for post-operative analgesia. This is in keeping with the study by Turan et al.29 which noted that patient satisfaction with post-operative pain management at 24hours was better in the gabapentin group compared to the placebo group. In this study, rescue analgesia was given from pain score above 3 as against pain score of 7 in the study of Rajendran et al23, this may have accounted for the better patient satisfaction found in this study compared to that of Rajendran et al23. At a pain score of 7 which is equivalent to moderate pain, the patient is already in painful distress, anxious and agitated hence poor patient satisfaction is achieved.
The study by Parikh et al30 combined tramadol and diclofenac for rescue analgesia, diclofenac being a Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) could cause gastritis, peptic ulcer disease and renal impairment. Hence, tramadol was carefully chosen in this study for rescue analgesia to avoid possible complications of NSAIDS which could occur especially in fasted patients.
The ASA physical status of every patient was clearly stated in this study, whereas the study by Dirks et al15 did not specify the ASA physical status of the study population. Pain perception and interpretation may be affected by patient ASA classification as an ASA V (moribund patient) may have altered sensorium and, may not be able to interpret pain perception accurately. This further authenticates the findings of this study when compared to that of Dirks et al15.
The recruitment of only female patients in this study may limit applicability of its findings to the female gender as. it has been found that there is a variation in pain perception in males and females, with females reporting higher pain intensity31. Pain assessment was carried out more than four times in this study unlike the study by Mardani-Kivi et al18 where pain was assessed only at the 6th and 24th hours after surgery, two values may not effectively represent the pain distribution of the study population.
Amanor-Boadu et al32 also carried out a study on patients undergoing gynaecological procedures to determine if ketamine has a pre-emptive analgesic effect. That study also had a homogenous sample population similar to this one. However, their patients had major gynaecological surgeries which could cause more intense post-operative pain due to more tissue damage in contrast to this study which recruited patients for day case procedures (minor surgeries). Their conclusion that pre-emptive analgesic effect could not be demonstrated could also be due to the drug they studied.
The results from this present study demonstrated the ability of preemptive analgesic intervention using 300mg of gabapentin to attenuate post-operative pain scores, decrease supplemental postoperative analgesic requirements, and prolong time to first rescue analgesic request. The pre-emptive analgesia involves preventing the pain before it starts by desensitizing the central nervous system.
Gabapentin is readily available as an over the counter prescription drug, and affordable by the average Nigerian patient. Gabapentin is less likely to cause addiction when taken in normal doses. Within the confines of this study, the side effects are mild and insignificant when compared to that of the placebo group. The benefits in the use of pre-emptive gabapentin are many. These include economic benefits as total amount of analgesics given to control post-operative pain is reduced, improved patient satisfaction due to better quality of post-operative pain control, reduced side effects of opioids as less amount is used for pain control. Others include early ambulation as well as reduced hospital stay thereby reducing the incidence of deep vein thrombosis (DVT) and thromboembolism as a result of prolonged immobilization. This is very relevant in the day case surgeries where opioids especially the long acting ones are not ideal, due to associated side effects like nausea and vomiting which delay the discharge of the patients from the hospital.
Limitations
The recruited patients were not evaluated for visual impairment which affects the accuracy of Visual Analogue Scale used for pain intensity assessment
There was a language barrier while administering the tools for pain intensity assessment. However, the use of an interpreter was of importance in ensuring accurate data collection.
The surgical procedures in this study were not homogenous as different tissues handling may have different degree of pain receptors hence, varying pain perception. However, the surgeries were restricted to gynaecological procedures only.
Conclusion
This study has demonstrated that oral administration of 300 mg of gabapentin 2 hours prior to surgery achieved good post-operative analgesia, decreased supplemental postoperative analgesic requirements and prolonged time to first rescue analgesic request with minimal side effects.
Recommendations
Recommendations are as follows;
- Use of gabapentin to improve the quality of post-operative pain control in our health institutions across the country as a component of multimodal analgesia regimen.
- Use of gabapentin as pre-operative regimen in most developing African countries where the availability and supply of opioids is erratic.
- Further studies on its usage for day case post-operative analgesia and for possible adoption as a premedication drug during surgery.
Conflict of interest
The Authors of this article declare that there is no conflict of interest and that no funding from any external source was received during performance of this study.
References
- Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms, 1994 2nded IASP Press, Seattle
- American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the peri-operative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management Anesthesiology 20121162248–273
- Royal College of Anaesthetists. Information for Patients (online). Available at: www.rcoa.ac.uk/clinicalstandards-and-quality/patient-information-leaflets (Accessed 21st September, 2017).
- Verma R, Alladi R, Jackson I, Johnston I, Kumar C, Page R, Smith I, Stocker M, Tickner C, Williams S, Young R. Day case and short stay surgery: 2. Anaesthesia. 2011; 66(5):417-34.
- Kulkarni S, Harsoor SS, Chandrasekar M, Bhaskar SB, Bapat J, Ramdas EK, Valecha UK, Pradhan AS, Swami AC. Consensus statement on anesthesia for day care surgeries. Indian journal of anaesthesia. 2017; 61(2):110.
- Beauregard L, Pomp A, Choiniere M. Severity and impact of pain after day-surgery. Can J Anaesth. 1998; 45: 304-311.
- Tong D, Chung F. Postoperative pain control in ambulatory surgery. Surg Clin N Am 1999; 79(2): 401-31.
- Benyamin R, Trescot AM, Datta S, Buenaventura R, Adiaka R, Sehgal N, Glaser SE, Vallejo R. Opioid Complications and Side effects. Pain Physician. 2008; 11:S105-S120
- Bonnefont J, Courade JP, Alloui A, Eschalier A. Antinociceptive mechanism of action of paracetamol. Drugs. 2003; 63:1 – 4.
- Woolf CJ, Chong MS. Preemptive analgesia: treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg 1993; 77: 362 – 379.
- Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: A meta-analysis. Br J Anaesth 2011; 106:454-462.
- Cheng JK Chiou L.C Mechanisms of the antinociceptive action of gabapentin. J Pharmacol Sci. 2006; 100(5): 471-486
- Montazeri K, Kashefi P, Honarmand A. Pre-emptive gabapentin significantly reduces post-operative pain and morphine demand following lower limb extremity orthopaedic surgery. Singapore Med J. 2007; 48 (8): 748-751. (16)
- Bafna U, Verma AP, Rajarajeswaram K, Khandelwa M. A comparison of effect of preemptive use of oral gabapentin and pregabalin for acute post-operative pain after surgery under spinal anaesthesia. Journal Anaesthesiol Clin Pharmacol 2014; 30 (3): 373-377.
- Dirks J, Frendsborg BB, Christensen D, Fomsgaard JS, Flyger H, Dhal JB. A randomized study of the effects of single dose gabapentin versus placebo on post-operative pain and morphine consumption after mastectomy. Anesthesiology 2002; 97: 560-564
- Jaykaran C, Tamoghna B. How to calculate sample sizes for different study designs in medical research. Indian J Psychol Med.2013; 35 (2): 121-126.
- 17.Liza T, Peter F. Pain management in day case surgery: Continuing education in anesthesia, critical care and pain..2015; 15: 180-183.
- Mardani-Kivi M, Mobarakeh MK, Keyhani S, Motlagh KH, Ekhatiari KS. Is Gabapentin Effective on Pain Management after Arthroscopic Anterior Cruciate Ligament Reconstruction? A triple blinded randomized controlledtrial. Arch Bone Joint Surg. 2013; 1(1): 18-22.
- Luscombe KS, McDonnell NJ,Muchatuta NA, Peach MJ, Nathan EA. A randomized comparison of parecoxib versus placebo for pain management following minor day stay gynaecological surgery. Anaesthesia Intensive Care. 2010; 38 (1): 141-148.
- Aryal D, Gurung R, Marhatta MN. Evaluation of the effect of gabapentin on postoperative analgesia with epidural morphine after abdominal hysterectomy. JCMS Nepal 2017; 13 (2): 251-257.
- Butt A. Mohammad K. Ommid M, Jehan N, Qazi S. A randomized double blind placebo controlled study of prophylactic gabapentin for prevention of post-operative pain and morphine consumption in patients undergoing mastectomy. The Internet Journal Of Anaesthesiology.2010; 30:1
- Hema VR, Ramadas KT,Bigi KP, Indu S, Arun A. A prospective observational study to evaluate the role of gabapentin as preventive analgesic in thyroidectomy under general anesthesia. Anesthesia essays and researches. 2017; 11 (3): 718
- Rajendran I, Basavareddy A, Meher BR, Srinivasan S. Prospective, randomized, double blinded controlled trial of gabapentin and pregabalin as pre-emptive analgesia in patients undergoing lower abdominal and limb surgery under spinal anesthesia. Indian J Pain 2014; 28:155-159.
- Panah Khahi M, Yaghooti AA, Marashi SH, Nadjafi A. Effect of preemptive gabapentin on post-operative pain following lower extremity orthopedic surgery under spinal anesthesia. Singapore Med J. 2011: 52 (12): 879-882.
- Ebong EJ, Mato CN, Fyneface-Ogan S. Pre-Incisional Intravenous Low-Dose Ketamine Does Not Cause Pre-Emptive Analgesic Effect following Caesarean Section under Spinal Anaesthesia. J Anesthe Clinic Res. 2011; 2 (138): 2155-6148? 2158
- Jabalameli M, Hornamand A, Safavi M, Chitsav M. Treatment of post-operative nausea and vomiting after spinal anesthesia for Caesarean delivery: A randomized double blinded comparison of midazolam, ondansetron and a combination. Adv Biomed Res. 2012; 1: 2.
- Cruz FM, Taranto P et. al. Gabapentin for the prevention of chemotherapy-induced nausea and vomiting: A pilot study. Support Care Centre 2012; 20(3): 601-606
- John P, Cunha DO. Drug Centre-Rxlist-common side effects of neurotin (Gabapentin) http://www.rxlist.com/neurotin.siseeffect-drug-centre htm 10/17/2018.
- Turan A, Kaya G, Karamanlioglu B, Pamukccu Z, Apfel CC. Effect of oral gabapentin on post-operative epidural analgesia. Br J Anaesth 2006; 96: 242-246
- Parikh HG, Dash SK, Upasani CB. Study of the effect of oral gabapentin used as pre-emptive analgesia to attenuate post-operative pain in patients undergoing abdominal surgery under general anaesthesia. Saudi J Anaesth.2010; 4 (3): 137-141
- Hussain AM, Khan FA, Ahmed A, Chawla T, Azam SA. Effect of gender on pain perception and analgesic consumption in laparoscopic cholecystectomy: An observational study. J Anaesthesiol Clin Pharmacol. 2013; 29 (3): 337-341
- Amanor-Boadu SD, Sanusi AA, Abdullahi AA. Ketamine for preemptive analgesia in major gynaecological surgery. Nig J surg Res. 2003; 5 (1-2):7-11.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29258/ebirim.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse3
Mr Karthikeyan P Iyengar (corresponding author)
Trauma & Orthopaedic Surgeon, Southport & Ormskirk Hospital NHS Trust, Southport, UK PR8 6PN .
Email: kiyengar@nhs.net
Dr Ayoub Behbahani
Core Surgical trainee Orthopaedics, Southport & Ormskirk Hospital NHS Trust, Southport, UK PR8 6PN
Email: a.behbahani@nhs.net
Mr William Y Loh (senior author)
Consultant Orthopaedic Hand Surgeon, Southport & Ormskirk University Hospital NHS Trust, Southport, UK PR8 6PN
Email: william.loh@nhs.net
Conflict of Interests and Disclosures
Karthikeyan Iyengar has nothing to declare. Ayoub Behbahani has nothing to declare. W Y Loh has nothing to declare.
Funding
None
Ethical Approval
The study protocol was approved by the local research and clinical effectiveness department.
Statement of Location
The study carried out in the department of Trauma & Orthopaedics at Southport & Ormskirk Hospital NHS Trust, Southport, PR8 6PN, United Kingdom.
Abstract
Purpose: Resistant tennis elbow refers to chronic lateral elbow pain not responding to conventional treatment. Roles and Maudsley (1972) had suggested resistant tennis elbow as probably an undiagnosed entrapment neuropathy of posterior interosseous nerve. We aim to evaluate the clinical application of Rule-of-nine test and effectiveness of unified tennis elbow and radial tunnel release surgical approach in management of resistant tennis elbow.
Methods: The study group consisted of 15 females and 5 men, with a mean age of 48 years. Demographic data, analysis of presenting symptoms, previous treatment, time to diagnosis and provocative tests was undertaken. Intra-operative findings were recorded. At follow-up of 12 months an overall outcome of treatment including pain, function and satisfaction was evaluated.
Results: 17 patients (85%) had an excellent or good outcome, 2 patients had a fair result and one patient had a poor result with continual shoulder and neck pain, paraesthesia in the same limb. At final follow-up most had complete relief of pain, 2 had mild pain, one on lifting heavy objects and one on continual typing. All in work resumed their jobs. There were no wound infections.
Conclusion: Rule-of-nine test increased the diagnostic accuracy of resistant tennis elbow. In this dual pathology, Unified tennis elbow and radial tunnel release surgical approach produced excellent relief of symptoms with minimal morbidity in a select group of resistant tennis elbow patients using a Modified Thompson’s single incision technique.
Keywords: tennis elbow; radial tunnel syndrome; posterior interosseous nerve; Rule-of-nine; surgical decompression.
Introduction
Chronic lateral elbow pain refractory to conventional treatment has been referred as resistant tennis elbow (RTE). Traditionally two commonest conditions attributed to patients with lateral elbow and proximal forearm pain has been tennis elbow (lateral epicondylitis) (TE) and radial tunnel syndrome (RTS).
First described by Runge in 1973[1], tennis elbow (TE) is suggested as an overuse injury involving eccentric overload at the origin of common extensor tendon particularly of the Extensor carpi radialis brevis (ECRB) [2,3]. TE is characterized by triad of lateral epicondylar pain, pain on resisted wrist extension and absence of other pathologies (2, 4). It commonly occurs mainly in those aged from 35 to 55 years, with an equal gender distribution [4, 5]. Pathophysiologically it is considered to be a focal hyaline degeneration within the fibres of common extensor origin [5, 6] especially of ECRB. There are features of angiofibroblastic hyperplasia micro tears of the origin of ECRB [7]. TE is considered to be a self- limiting condition with most responding to conservative means [4]. Conservative treatment includes physiotherapy and eccentric exercises, shock-wave treatment, laser therapy, acupuncture, elbow straps, injections of local corticosteroid, botulinum toxin and autologous blood or platelet-rich plasma [5]. Various differing operative techniques including both open and arthroscopic methods have been described [4, 5, 6, 8]. Roles and Maudsley (1972) put forward a hypothesis that chronic tennis elbow pain could be because of the entrapment neuropathy of the posterior interosseous nerve (PIN) and coined the term resistant tennis elbow (RTE) [9]. However, van Rossum et al [10] concluded RTE could not be explained by entrapment neuropathy and the role of surgical exploration was unfounded. Henry and Stutz [6] highlighted the possibility that the 2 clinical entities of TE and RTS may in fact represent an integrated pathology. They suggested that treating both pathologies together may improve pain and function in patients suffering from RTE.
We evaluate the effectiveness of unified tennis elbow and radial tunnel release surgical approach in the management of RTE in this study.
Material and methods
Study design
We carried out a retrospective study of all patients over the age of 18 years who underwent the unified tennis elbow and radial tunnel release procedure for treatment of resistant tennis elbow at our unit with a minimum of one year follow up. The study protocol was approved by the local research and clinical effectiveness department.
Patients
All patients over the age of 18 years referred to our upper limb unit with chronic persistent lateral elbow pain from triage services between January 2008 and December 2013 were included in the study. None of these patients underwent nerve conduction studies. The Resistant Tennis Elbow (RTE) was a clinical diagnosis. The Rule-of-nine test helped increase diagnostic accuracy of this condition when the posterior interosseous nerve (PIN) in the radial tunnel was involved [11]. Data was collected from Electronic Patient Records (EPR-Evolve), Patient Archived Computer system (PACS), operative theatre log book, physiotherapy assessments and discharge summaries. All patients underwent routine pre-operative anaesthetic assessment. The surgery was carried out by a senior surgeon as a day case surgery on a short surgical stay unit under general anaesthetic with use of an arm tourniquet.
Outcome measures
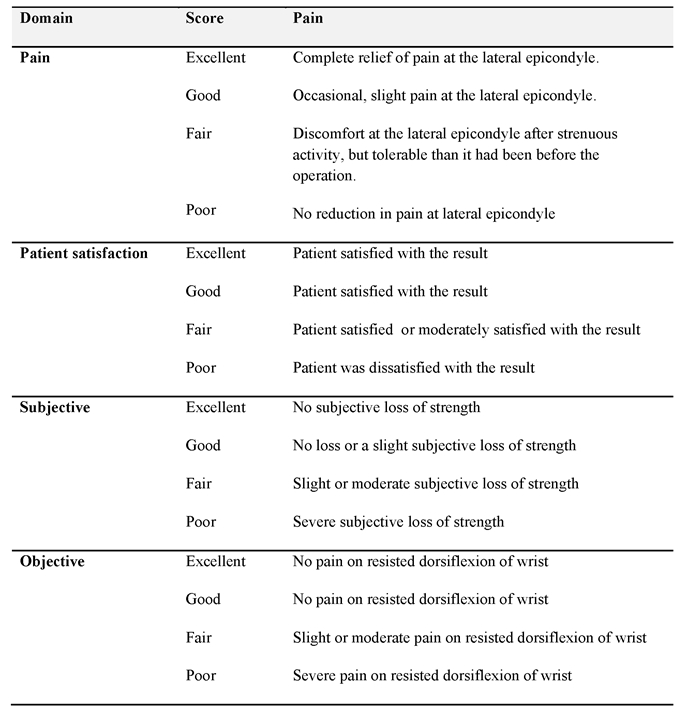
We collected demographic data including age, sex, hand dominance and occupation. Symptoms and examination findings at clinic presentation, time until diagnosis of resistant tennis elbow in the unit, any treatment prior to referral was noted. Specific tests for tennis elbow and radial tunnel syndrome including Rule of nine test were performed. Pain was assessed using Visual Analogue Scale (VAS). Intra-operative findings were recorded for clinical correlation. The patients were followed up in the clinic at 6 weeks, 3 months and 12 months following surgery for assessment. We also administered patient satisfaction questionnaire at follow-up and the overall outcome of treatment was rated using the grading system developed by Verhaar et al [8] (Table 1).
Table 1: Verhaar grading system for outcome assessment of lateral release for tennis elbow.
Operative technique
The affected arm was supported on an arm table. Using the modified Thompson’s approach a 4 centimetre longitudinal incision was placed over the proximal radial shaft of the affected elbow. Under 3.0 x loupe magnification the interval of Extensor carpi radialis brevis (ECRB) and Extensor digitorum communis (EDC) musculature was developed. We specifically noted and documented intra-operative thickness of ECRB & EDC fascia's, thickness and tightness of the proximal border of supinator, the bulk of the supinator muscle and features of posterior interosseous nerve (PIN) entrapment. Thickened fascia’s of ECRB and EDC was released to reduce traction on ECRB and EDC. A one centimetre gap was noted to be adequate to release the traction on these two muscles and the common extensor origin. The PIN was located at superior border of supinator and traced proximally and distally. The whole length of the radial tunnel was released, making sure the complete division of superior border of supinator, its Arcade of Frohse and inferior border of supinator. Fascial covering of superficial part of supinator was divided along the PIN path. Bipolar diathermy was used to achieve haemostasis. The wound was closed in layers using absorbable sutures.
The elbow was dressed with wool and crepe bandage and supported in a poly sling. The patient was safely discharged home the same day with regular analgesia and post-operative instructions.
Rehabilitation
A standardised rehabilitation protocol under the supervision of physiotherapists at regular intervals was used. This was divided in 3 phases. The first phase in the first two weeks suggested use of regular analgesia, use of cryotherapy of the elbow, avoidance of lifting heavy objects with the arm, silicone patch over the scar whilst the scar matures. The intermediate phase consisted of scar mobilization with composite stretching of the ECRB and EDC muscles. Combined position of elbow extension, forearm pronation and wrist flexion exercises (hourly exercise and 10 repetitions per session) was undertaken. Strengthening of forearm is only begun after the full composite stretch can be comfortably performed (usually 4-6 weeks post-operatively). The third phase consists of progressive strengthening from week 6 to week 8. This standard progression of first achieving elbow full range of movement and composite stretch, progressive strengthening exercises with final aim of return to full activity is planned over a period of 4 months.
Statistical analysis
The values of assessed parameters were collected. Anonymised data was recorded onto a data collection sheet on Microsoft Excel on a password-protected computer. A descriptive analysis and outcome assessment was undertaken.
Results
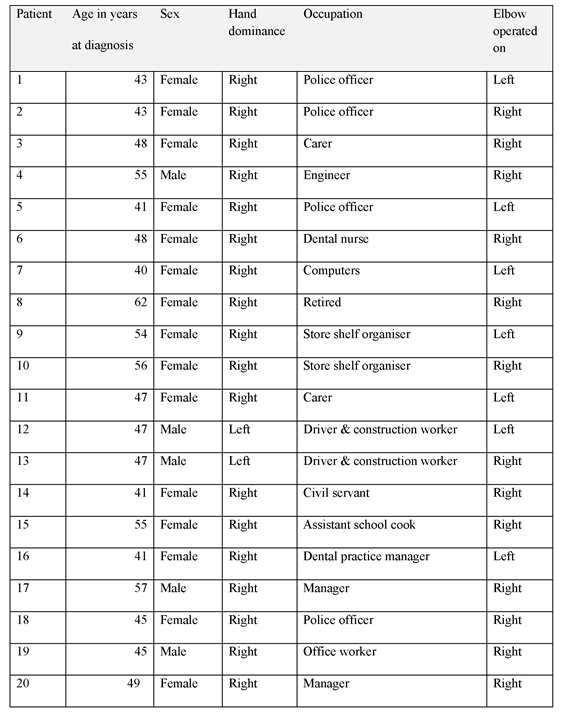
A total of 15 women and 5 men, aged from 40 to 62 years (mean 48 years) underwent unified tennis elbow and radial tunnel release procedure for treatment of resistant tennis elbow. Seven patients underwent surgery on the non-dominant side. No patient was able to provide hints to suggest a specific cause, though four patients correlated the condition to an injury sustained. Three patients had desk jobs, one patient was retired and the rest had fairly manual jobs. (Table 2).
Table 2: Demographic data of patients undergoing unified elbow release for resistant elbow.
All patients suffered long standing pain located at the lateral epicondyle with symptoms of weakness and pins and needles along the forearm in variable instances. The duration of symptoms before referral to our unit varied from 6 months to 48 months (mean, 18 months).
Despite various non operative treatments including analgesics (all 20), physiotherapy (13/20), elbow supports (15/20), local steroid injections (13/20) ultrasound therapy (2/20) and acupuncture (7/20) had been undertaken, all patients still had symptoms which continued to interfere with activities of daily living.
There were consistent features of lateral epicondylar and proximal forearm tenderness with positive provocative tests. The rule of nine test, resisted wrist dorsiflexion test and middle finger test was positive in 18/20 (90%), 18/20 (90%), and 17/20(85%) respectively.
The ECRB and EDC fascia was invariably found to be thickened in most cases. Along with this the superior proximal border of the supinator, Arcade of Frohse and sometimes the lower border were tight in all patients.
Outcome
The overall outcome as graded by Verhaar system revealed a good to excellent result in 17 patients (85%), fair in 2 patients and poor in one patient. The poor result was in a lady with shoulder and neck pain with paraesthesia in the affected limb. The 2 patients in the fair group had discomfort at the lateral epicondyle after strenuous activity (continual typing, lifting heavy objects), but more tolerable than before the operation.
Pain
At the final follow-up review, 17 elbows were painless, one patient had mild pain after lifting heavy objects at his manual work, one had pain on continual typing only and one had shoulder and neck pain with paraesthesia in the affected limb. Subjectively 19 patients (95%) were satisfied with the final outcome. All elbows had full range of moment and were stable.
Complications
All wounds healed at the time of six week review. There were no wound infections. However one patient had mild scar tenderness which settled with local massage, desensitization therapy at final review. Another patient had numbness distal to the scar but this did not affect her activities of daily living.
Discussion
Both tennis elbow and radial tunnel syndrome are distinct entities and treated as such. However, a subset of patients treated for lateral elbow pain amongst these exists who are not improving with conventional treatment and present a diagnostic dilemma.
ECRB and to a lesser degree a portion of the EDC are known to be responsible for excessive traction inducing lateral epicondylar tendinosis and micro tears [5,6,7]. The supinator, primarily the proximal thickened tendinous edge also known as Arcade of Frohse is responsible for posterior interosseous nerve compression (PIN) in the tunnel [12, 13]. However to lesser extent the superficial bulk of supinator muscle which blends with the thickened ECRB also appears to cause some element of PIN compression as evident with two of our consistent intra-operative findings of thickened ECRB fascia and tight superior border of supinator muscle which was released during the surgery.
The diagnostic dilemma is due to overlapping features amongst both the conditions. TE is identified primarily by local lateral epicondylar tenderness and positive provocative tests such as pain on resisted pronated wrist dorsiflexion and middle finger extension [4, 13]. RTS on the other hand refers to pain in the proximal forearm distal to lateral epicondyle and similar positive provocative tests. Henry and Stutz [6] have pointed out that clear and convincing data has not been brought forward to uniquely identify or differentiate TE form RTS in isolation by some of these tests.
As noted by P K Tan et al [14], all of the patients had a conservative treatment prescribed and undertaken prior to referral to our unit. Most of these patients were seen and treated in primary care or musculoskeletal triage clinics usually with physiotherapy or local steroid injections. The mean duration of symptoms before referral to our unit until diagnosis of RTE was about 18 months. Such a delay probably reflects the diagnostic dilemma faced by treating clinicians.
In considering surgical option for treatment of RTE, we need to address both pathologies contributing to RTE. Our consistent intra-operative findings of thickened ECRB fascia and tight thickened proximal supinator border and also a thickened supinator musculature in some cases confirms our belief that RTE is probably a unique combined pathology.
Our finding of 85% good or excellent post-operative result based on Verhaar et al grading and 95%subjective satisfaction supports our philosophy of treating RTE as a dual pathology in the same elbow.
The Unified tennis elbow and radial tunnel release approach presents a unified approach to treat both of these co-existing pathologies simultaneously. This retrospective study supports the rationale of releasing of traction on extensor carpi radialis brevis and release of posterior interosseous nerve entrapment to treat resistant tennis elbow using a single incision technique.
Conclusion
A positive Rule-of-nine test demonstrated the need of posterior interosseous nerve decompression in Resistant Tennis Elbow patients. Unified tennis elbow and radial tunnel release approach produced excellent relief of symptoms with minimal morbidity in a select group of resistant tennis elbow patients using a single incision technique.
References
- Runge F. Zur genese und behandlung des schreibekramfes [in German]. Berl Klin Wochenschr 1873; 10: 245.
- Garden RS. Tennis elbow. J Bone Joint Surg Br 1961; 43:100–6.
- Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am 1979;61:832–9
- Kumar VS, Shetty AA, Ravikumar KJ, Fordyce MJ. Tennis elbow--outcome following the Garden procedure: a retrospective study. J Orthop Surg (Hong Kong). 2004; 12:226–9.
- Ahmad Z, Siddiqui N, Malik SS, et al. Lateral epicondylitis: a review of pathology and management. Bone Joint J. 2013; 95(B):1158–64.
- Henry M, Stutz C. A unified approach to radial tunnel syndrome and lateral tendinosis. Tech Hand Up Extrem Surg. 2006 Dec; 10(4):200-5.
- Cyriax JH. The pathology and treatment of tennis elbow. J Bone Joint Surg 1936; 18:921–940.
- Verhaar J, Walenkamp G, Kester A, et al. Lateral extensor release for tennis elbow. A prospective long-term follow-up study. J Bone Joint Surg Am. 1993; 75:1034–43.
- Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br 1972; 54:499–508.
- van Rossum J, Buruma OJ, Kamphuisen HA, Onvlee GJ. Tennis elbow--a radial tunnel syndrome? J Bone Joint Surg Br. 1978 May; 60-B (2):197-8.
- Loh YC, Lam WL, Stanley JK, Soames RW. A new clinical test for radial tunnel syndrome - the Rule-of-Nine test: a cadaveric study. J Orthop Surg (Hong Kong) 2004; 12:83–86.
- Lister GD, Belsole RB, Kleinert HE. The radial tunnel syndrome. J Hand Surg Am. 1979; 4(1):52-59.
- Malhotra M, Bhat AK, Acharya A. Radial tunnel syndrome: Diagnostic and treatment algorithm. J Kar Orth Assoc. July-Dec 2017; 5(2): 14-17.
- Tan PK, Lam KS, Tan SK. Results of modified Bosworth's operation for persistent or recurrent tennis elbow. Singapore Med J. 1989 Aug; 30(4):359-62.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/34960/293-iyengar.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse4
British Association of Day Surgery
Annual Conference
27 -28 June 2019
Royal Society of Medicine, London
This year’s conference was a milestone for the British Association of Day Surgery (BADS), as it was the 30th year since the organisation was founded. The venue itself was very impressive and being in Central London enabled delegates to attend from far and wide. This year, once again, saw a record number of delegates attending from all around the world, namely Australia, South Africa, China, Switzerland, Belgium, Iceland, and Croatia. It is encouraging for BADS that the importance of day case and short stay surgery is recognised not only in the UK but internationally.

Once the Presidents welcome and housekeeping had been delivered it was straight into the first plenary session with presentations on “Implementing a day case gastric bypass service” delivered by the team at St George’s University Hospital NHS Foundation Trust in London including expert speakers Mr Marcus Reddy, Consultant General Surgeon, Mr Omar Khan, Consultant Bariatric Surgeon, Dr Ajit Kayal, Consultant Bariatric Anaesthetist and Dr Nick Fletcher, Consultant Anaesthetist. The session was well-received and informative. It was a pleasure to hear from Mr Derek Carpenter, a patient who had undergone day case gastric bypass, to share his experiences. All too often we listen to the professionals on the management/implementation of pathways and tend to oversee the most important person, the patient, whose active participation is essential in successfully introducing any new pathway.
After coffee we moved onto the second plenary session, which promised to be thought provoking and interesting, entitled the “Presidents’ Plenary”. As it was our 30th Conference we wanted to celebrate by inviting two past presidents of BADS and our current President to speak on topics that they feel passionate about.

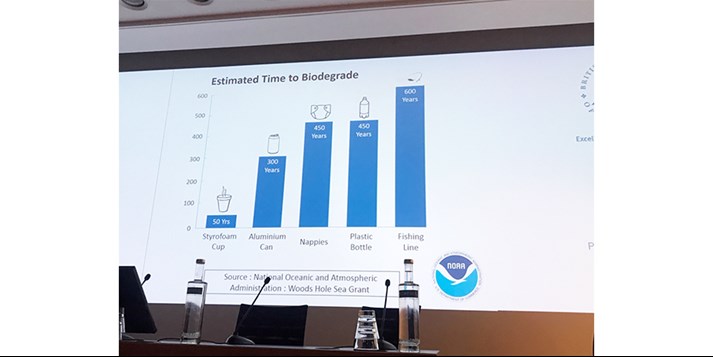
Professor Doug McWhinnie Consultant Surgeon from Milton Keynes started the session by talking about environmental issues and how in day surgery can we help to tackle these problems. He discussed recycling, unnecessary waste and potential ways in which we can help in reducing the waste we produce, not just in the work environment but in our everyday lives as well. This lecture was inspirational giving the delegates food for thought in how their units could do their bit to help to tackle environmental issues and providing motivation to achieve this in their everyday lives as well.
The second lecture of the President’s plenary session was given by Dr Ian Jackson, retired Consultant Anaesthetist providing an interesting talk on how technology can improve a patient’s day surgery journey by increasing the effectiveness and efficiency of the pathway. Examples of this included online preoperative assessment and web-based patient information portals. Dr Jackson provided further insight into tackling environmental issues, explaining how technology could be used to reduce paper used in the work environment.
The final talk in the President’s plenary session was delivered by our President, Dr Mary Stocker. She highlighted the ever-increasing range of procedures now routinely undertaken in day surgery, detailed in the new edition of the BADS Directory of Procedures and how we can optimise our day case rates by developing pathways to adapt into the day surgery setting. She also discussed the new Model Hospital website, which benchmarks day surgery rates against all the procedures that are in the BADS directory. This enables the user to identify top performers in the country so they can learn from their experiences and share their knowledge.
All speakers gave inspirational presentations and produced good debate amongst the delegates, I am sure what was presented will be fed back to Day Surgery teams throughout the UK and beyond to enable the improvement of the management of services and patient experience with an emphasis tackling environmental issues.
The afternoon programme started with the first of our parallel free paper session. The standard of presentations was high reflecting a large number of high-quality abstract submitted to the conference. It is always encouraging to see so many submissions as it demonstrates all the hard work that is occurring amongst the day surgery teams throughout the country and abroad. Subjects included, ‘Improvement in breast surgery’, ‘Improving informed consent for laparoscopic cholecystectomy’, Improving quality in operation notes in day case surgery’, ‘Re-audit of fasting policy’ and many more. All these presentations will be made available to BADS members for viewing on the BADS website.
The free paper session was followed by three parallel workshops:
- ‘Day case spinal anaesthesia’, chaired by Dr Ben Fox, Consultant Anaesthetist and Dr Anna Lipp, Consultant Anaesthetist
- ‘Does everyone need a carer for 24 hours?’ Chaired by Ms Francine Horide, Staff Nurse in preoperative assessment and Dr Jane Montgomery, Consultant Anaesthetist
- ‘Optimising your day case pathway’, chaired by Mrs Fiona Belfield, Senior Sister Day Surgery and Dr Theresa Hinde Consultant Anaesthetist
Feedback from all sessions was positive and generated interesting debate, allowing the delegates to ask questions and gain advice from the chairs as to their experiences in the subjects discussed. BADS have been running individual workshops for several conferences now. They are a good forum for networking with colleagues who encounter the similar issues and offer an important opportunity to seek specialist support and advice.
The final session of the first day commenced with the second parallel free paper session. A wide variety of subjects was presented and both sessions were well attended. Titles included ‘Retrospective Audit Examining On The Day Theatre Cancellations’, ‘Service evaluation of parent bleep for children having day surgery’, ‘Day case Laparoscopic Cholecystectomy in East Africa’ and ‘Management of postoperative urinary retention in day surgery utilising the international prostate scoring system’.
The BADS Annual General Meeting (AGM) was held in the main auditorium. Mary Stocker, BADS President detailed all the work Council members had undertaken throughout the year. This includes the introduction of our conference app and the Slido system, both measures aimed at improving the delegates’ conference experience; publication of the 6th edition of the BADS Directory and its launch that the conference and the commencement of talks regarding accreditation and its future within day surgery. She welcomed new BADS Council members, namely, Adam Kimble, Edward Dunstan, Karen Harries and Shaun Clee, our new lay member. She thanked outgoing Council members Dr Anna Lipp, Paul Rawlings and Anna Girolami for their hard work and commitment during their time on Council.
Reports were presented by the Treasurer, Hon Secretary, Conference Secretary, Journal of One Day Surgery (JODS) Editor, Publications Officer and Website Officer. All reports are available to view on the BADS website.
The AGM was followed by a drinks reception on-site at the Royal Society of Medicine. This was well attended and welcomed after a full programme on the first day. It gave the delegates a chance to network with exhibitors and other attendees in a relaxed environment, prior to an evening that would leave the delegates free to explore the sights of London!
Friday started with a Urology-themed plenary session. This was a multidisciplinary session with a presentation from Mr Mark Rochester a Consultant Surgeon from Norwich, talking about the different day case techniques and treatments available for Benign Prostatic Hyperplasia. Dr Mary Stocker, Consultant Anaesthetist from Torbay discussed anaesthetic techniques, which enable urology patients to undergo procedures such as TURP, laser prostatectomy, and Urolift as a day case procedures. The session was concluded by Alex Alen, Senior Sister at Torbay Hospital. She gave an insight into the importance on preparing the patient for day case surgery at pre assessment and that planning for more complex procedures pre-operatively is the key for a successful same-day discharge. This session highlighted the importance of good communication and team work amongst the multi-disciplinary team.
The urology plenary session was followed by the prize presentation session. The six highest-scoring abstracts were presented. They were scored by three expert judges and an audience vote via the Slido app. Topics varied from ambulatory free-standing bed-less facility to developing a pathway for upper limb arthroplasty.
Moving straight on from the prize presentations was one of the highlights of the Conference, Professor Doug McWhinnie Consultant Vascular Surgeon and General Surgeon, Milton Keynes and Dr Ian Smith Retired Senior Lecturer in Anaesthesia both past presidents of BADS debated “All slow surgeons and slow anaesthetists should be banned from Day Surgery”.

Both debaters gave convincing arguments to support their viewpoints. The debate unfolded with great humour and much banter, providing hugely entertaining and thought-provoking material for discussion.

The afternoon session began with a presentation for the winner of the prize presentations, this year going to Graham Harris for his talk on ‘Improving fluid fasting times and postoperative nausea rates after introducing a liberal preoperative fluid policy for patients undergoing elective surgery’.
Well done Graham! Unfortunately Graham was unable to collect his prize, as he had to travel back for an on-call that night, the prize being received by a colleague on his behalf.
Again, I would like to take the opportunity to thank all those individuals who submitted their work for presentation at this year’s Conference, and we encourage all presenters to publish their work in the BADS Journal of One Day Surgery (JODS). Submission information and author guidelines can be found on the BADS website. Each year the quality of submitted abstracts seems to get better and it is reassuring that there are so many aspects of Day Surgery being studied, which leads to improvements and developments in the field of day case and short-stay surgery throughout the UK and further afield.
Following the presentation of prizes, Mary Stocker formally handed over the Presidential reign to Kim Russon. Kim thanked Mary for all her hard work and is looking forward to her time as President.

And so, it came to the last plenary session of the conference, entitled ‘Hysterectomy and Enhanced Recovery’. The team from Royal Surrey County Hospital, Guilford shared their experiences. Again, this was a multi-disciplinary session, so the audience could benefit from the experience of different members of the team. Ms Wendy-Rae Mitchell, an Endometriosis Specialist Nurse spoke first, discussing the history behind the enhanced recovery programme, its purpose and how it has improved vital communication with patients undergoing such a potentially life-changing operation. She emphasised the need to take into consideration cultural beliefs amongst many factors and the impact such an operation may have on these patients. It also ensures that the patients are prepared both physically and emotionally for such an operation given that the patient will only be in hospital for a short time.
Next to present was Dr Piers Johnston, Consultant Anaesthetist, who gave us an overview of the peri-operative management and Enhanced Recovery in relation to day case hysterectomy, which included a review of pre-operative preparation, per-operative pain relief options and patient positioning to ensure positive patient experience and safety.
The final talk at the Conference was delivered by Mr Andrew Kent, Consultant Surgeon, giving an overview of ‘Laparoscopic Hysterectomy Intrafascial (LHi) Technical Aspects, Benefits and Desired Outcomes’ and how this enabled the Enhanced Recovery Programme to become successful.
Again this demonstrated how working as a team and bringing each of the elements together, enabled this to become the success that it is today.
And so this closed another successful conference with delegate numbers exceeding 200 and a real buzz was felt over the two days which is encouraging. I am sure the delegates who attended the conference felt inspired and motivated in bringing back to their individual units what they have learnt and what could be improved with their work environment.
It is always reassuring to know that there are so many Day Surgery units endeavouring to provide the best service and achieve the best outcomes possible. BADS would like to take this opportunity to acknowledge all the hard work and dedication amongst the teams to help to make this happen. Please keep up the good work, as without you this would not be possible.
I would also like to take the opportunity to thank everyone who participated in making this year’s our 30th conference so special, and for the delegates who attended for enabling us to continue to strive to always push the boundaries of Day Surgery.
Look forward to seeing you in Cardiff in 2020.
Fiona Belfield
Conference Secretary
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse5
Paper Session 1a: Surgery/Management
1a1 Ambulatory emergency care in general surgery: a scoping review
Lisa Massey1,2, Jo Day2, Rob Bethune1, Iain Lang2
1 Royal Devon and Exeter Hospital, Exeter, United Kingdom. 2 University of Exeter, Exeter, United Kingdom
Abstract
Introduction: Ambulatory emergency care (AEC) can include diagnosis, treatment and follow-up delivered outside standard inpatient admission. It has become well-established in medicine within the UK but not yet within surgery. The aim of this review is to map the available evidence for the use of AEC in general surgery and describe what outcomes have been used to assess methods of delivering this care.
Methods: A systematic search of Pubmed and CINAHL databases was conducted using terms including “ambulatory surgery” and “abdominal emergency”. All studies published in the English language describing a method of AEC (including ambulatory assessment and day case emergency surgery) were included.
Results: Of 620 records identified, 34 studies were eligible for inclusion into the review. These comprised 3 review articles and 31 studies describing original research. A range of methods of AEC were found including ambulatory assessment and day case emergency surgery (mainly appendicectomy) which could be delivered within existing inpatient areas or dedicated day case units with definitions used including <12hr stay, no overnight stay and <24hr stay. Clinical outcome measures commonly used include length of stay, success of ambulatory care and morbidity. There were little qualitative or economic outcome data available.
Conclusions: Research in this area is still aiming to establish feasibility. Only a small number of studies have used measures other than basic clinical outcomes. There is a need for further studies to elucidate the benefits from AEC and the best way to implement or expand these services.
1a2 Improvement of the delivery of day case breast surgery - a closed loop audit
Irena Stefanova1, Kathryn Duke1, Nadia Gilani1, James Livingstone1, Henry Conchie2, Elizabeth Clayton1
1 Royal Surrey County Hospital, Guildford, United Kingdom.
2 Royal Surrey County Hospital, Guildofrd, United Kingdom
Abstract
Introduction: Breast cancer surgery is increasingly undertaken as day case procedure. The British Association of Day Surgery recommends that 95% of Wide Local Excisions(WLE) and 50% of mastectomies are performed as zero-night-stay cases. Many hospitals struggle to achieve the Gold Standard. This audit aimed to assess our unit’s performance before and after the introduction of improved education.
Methods: Retrospective data for 982 patients undergoing breast surgery over a 3-year period before, and 128 patients over 3 months after the introduction of internal education, was captured. The Education Programme targeted medical staff, nursing staff and most importantly patients. We organised meeting-discussions, designed patient information leaflets with safety-netting and drain management advice; contact details for the breast team. GraphPad-v7.04 was used for data analysis.
Results: Between March 2014 and April 2017, the identified zero-night-stay rates for WLE and Mastectomies were 67% and 9%, respectively. Following the implementation of internal education our unit’s performance has significantly improved. We have achieved same-day-discharge rates of 88%(51/58)(p<0.05) for WLE, and 19%(4/21)(p=0.06) for Mastectomy, between April and June 2018. There was no increase in re-admissions/complication rates. The improvement resulted in larger profit for the Trust equivalent to £40, 000 per year. We now compare favourably to other trusts being in the top25% of hospitals in the country, but not yet achieved top5% status.
Conclusions: The introduction of improved education has led to improved utilisation of day case breast surgery at our Centre, with maintained high levels of patient satisfaction.
1a3 Audiovisual technology to improve informed consent for laparoscopic cholecystectomy
Mehdi Raza
Dartford and Gravesham NHS trust, Dartford, United Kingdom
Abstract
Introduction: Despite laparoscopic cholecystectomy being a major operative procedure to remove the gallbladder, the general impression is that it is a common procedure with early recovery. We all know complications, though not common, can be quite severe like bile duct injury. Improving the understanding of the anatomy and the risks should help in reducing the ‘on the day’ anxiety of consenting. We aim to provide all common procedures with comprehensive audiovisual advice in clinic .
Methods: We audited the individual perceptions of the standard consenting in clinic and on the day of the procedure. This included paper consent and then literature for reading at home. We asked them if they wanted audiovisual information to help with understanding the anatomy and the risks. We got excellent feedback from 50 patients. A video was made with the help of a film company (funded by the author).
General advice was received by showing all doctors in our audit meeting . We closed the loop of our audit by using the video in our clinics to consent people. A consent form was signed and literature was provided to take home.
Results: Excellent feedback from patients was received. Very good understanding of the risks was obvious by the questionnaires signed by the individuals.
Conclusion: Consenting can be improved by using audiovisual aids. This can be uplodaed on to a website for perusal at home as well.
1a4 A Cost-effective and Safe Way to Alleviate the Soaring Medical Demands in China: A Case Study
Lisha Jiang, Hongsheng Ma, Yan Dai
West China Hospital,Sichuan University/West China Hospital of Medicine, Chengdu, China
Abstract
The objective of this case study is to analyze the leading success, existing barriers and future planningof day surgery, which also can prove it is a cost-effective and safe way to alleviate soaring medical demands in China. Firstly, this case briefly introduces current healthcare statues and medical problems in China, then lies on the case study hospital, West China Hospital, Sichuan University. We found that the success of West China Hospital on day surgery is the lack of payment obstacles and winning highly patient acceptance, utilize different processes to manage. Especially under the background of promoting day surgery by the government which makes it take great leap forward. As one of the earliest central health organizations that started day surgery service in mainland China, West China Hospital, Sichuan University has conducted approximate 140 thousands day surgery cases in the past decade, the case number keep increasing each year, but, the patient satisfaction rate remains a high level, no day surgery or anesthesia related death and severe complication.This is also message for the world that is in southwest China, Chengdu, there are a bunch of young enthusiasts and health professionals who are trying to devote their careers to promote day surgery which could provide high quality and cost-effective medical care for patients.
1a5 Improving quality of operation notes in day case surgery
Matthew Flynn1, Sam Lakey2
1Mater, Belfast, United Kingdom. 2Queens University Belfast, Belfast, United Kingdom
Abstract
AIM: Good operation notes are a key component of “Good Surgical Practice” where specificity can help future treating clinicians and in medico-legal cases. This audit aimed to improve the quality of operation notes in an urban acute hospital against standards set by the Royal College of Surgeons (RCS).
METHOD: Retrospective review of 20 case notes in a day case procedure unit dealing with local anaesthetic excisions, primarily of the head and neck. Change of practice was achieved by dissemination of preliminary audit results, introduction of a checklist at the point of operation note completion and simplification of the operation note proforma itself. The audit was repeated following intervention.
RESULTS: Recording of procedure time rose from 0% to 100%, logging of operative findings and operative diagnosis improved from 80% to 100% and a detailed note on postoperative instructions arose from 60% to 75%.
CONCLUSION: Proforma redesign along with necessary education and efficient recording prompts lead to improvement over time in operation notes, in accordance with best pracice. Simplification of historically cluttered forms led to a good response from clinicians.
1a6 Factors Contributing to Readmission After Elective Day-Case Surgery in a dedicated Day Surgery Unit
Alan Askari, Ratna Makker, Amjid Riaz
West Hertfordshire Hospitals NHS Trust, Watford, United Kingdom
Abstract
Introduction: Readmission following elective day-case surgery remains an ongoing issue in the NHS. The aim of this study is to determine what factors are associated with an increased likelihood of readmission following elective day-case surgery
Methods: All patients undergoing elective day-case surgery under General Anaesthetic across all surgical specialties at our institution over a 2-year period were included in this study. Data on gender, age, ASA grade, smoking status and BMI were analysed.
Results: A total of 4,254 patients with the relevant data were identified, of whom 37% (n=1,589) were Male. The vast majority of patients (68.9%, n= 2,930/5,254) had a BMI over 25. Nearly a third (32.3%, n= 1,375) were classified as obese with a BMI over 30. The overall readmission rate was 8.9% (n=379). There was a significant difference between smokers and non-smokers in terms of readmission rates (Smokers: 9.4%, Non-Smokers: 7.0%, p=0.022) as well as increasing age (>75 years: 13.0%, 15-25 years old: 6.0%, p<0.001). ASA was also associated with a higher readmission rate (ASA 1: 7.0%, ASA>1: 10.1%, p<0.001) however obesity was not (BMI >30: 9.7%, BMI 20-25: 7.9%, p=0.231). There was also no difference in readmission rates based on gender (Male: 9.8% vs Female: 8.4%, p=0.109).
Conclusions: Increasing age, ASA grade and current smoking are factors associated with a higher readmission rate, obesity itself however is not. Concerns over obese patients undergoing day-case surgery appear to be unjustified as they did not experience a higher rate of admission than the non-obese population.
Paper Session 1b: Anaesthetics
1b1 Re-audit of local fasting policy “Sip until we send”
Daniel Greenwood, Sally Dunlop
Airedale General Hospital, Steeton, United Kingdom
Abstract
Introduction: Following previous audit showing prolonged fasting times for fluids and a patient satisfaction survey revealing thirst as the most complained about symptom post surgery we introduced “sip until we send” in January 2018. Patients are allowed to drink water freely on the ward pre-operatively until they leave to come to theatre. This re-audit was to assess the impact of the new policy.
Method: Prospective audit of elective surgery patients over 2 weeks. Audit forms comprised tick box for ward staff to describe the volume of water consumed and further questionnaire to be completed in the anaesthetic room.
Results: 138 forms completed. Mean fasting time for fluid (excluding water as part of “sip until we send”) was 6 hours 22 minutes. However, 89% had been drinking water on the ward, with an average consumption of just over 1 cup of water. 51% of patients reported no thirst at the time of induction. Of those who did report thirst, 76% had consumed less than 1 cup of water.
Conclusions: Since the introduction of “sip until we send” we have had no incident forms completed related to aspiration. This re-audit shows that the majority of patients are taking water on the ward and that this has contributed to reduction in complaints of thirst. The use of the word “sip” may have caused some confusion as to the volume of water which patients are allowed, and further education is planned.
1b2 Influence of catastrophism on the quality of recovery after orthopedic and gynecologic one day surgery
Sibel Boz, Luc Van Obbergh, Turgay Tuna
C.U.B. Hospital Erasme, Brussels, Belgium
Abstract
Introduction: The assessment of postopoerative recovery should consider pain, nausea, vomiting but also quality of recovery (QoR). The Pain Catastrophizing scale (PCS) is an efficient tool to predict postoperative pain. Our aim was to determine the influence of catastrophism and its three subscores (rumination, helplessness and amplification) on QoR after orthopedic and gynecologic one day surgery.
Methods: Adults programmed for orthopedic and gynecologic one day surgery were prospectively recruited during five months . The PCS was completed during the preoperative anesthesia consultation. Patients were asked to complete the Quality of Recovery-9 questionnaire on postoperative day (POD) 1, 3 and 7 and about the intensity of pain, nausea and vomiting during that period.
Results: The median (IQR) PCS, rumination, magnification and helplessness scores were respectively 25 (0-46), 8 (0-16), 6 (0-11), 10 (0-24). PCS and its subscores did not influence postoperative pain, nausea and vomiting. For the gynecologic population, on POD 1 and 3, patients with high rumination score (≥8) had a poorer QoR-9 score than patients with low rumination (<8), p=0,02, and on POD 7, the 3 subscores of the PCS influenced the QoR significantly.
Conclusion: For the gynecologic population, the QoR was influenced by the rumination subscore on POD 1 and on POD 3 and by the three subscores on POD 7. The PCS and its three subscores did not influence QoR in the orthopedic population. 61,9 % of those patients had locoregional anesthesia.
1b3 The highs and lows of day case surgery
Rohan Goel, Rashmi Khirwadkar, Jenny Hardaker, Caroline Yeoman
St Helens and Knowsley Teaching Hospitals NHS Trust, Prescot, United Kingdom
Abstract
Introduction: Diabetic patients attending hospital for elective day case surgery can have difficulties with fasting and altered medication regimes leading to hypo/hyper glycaemia. As a result it was found that patients were having procedures cancelled on the day due to staff in a district general hospital day case unit struggling with knowing how to manage patients’ blood sugars prior and post procedure.
Methods: Meetings with staff working in the day case unit and the endocrinology team were held to see what issues were being faced and how these could be best addressed.
Using the Association of Anaesthetists guidelines, the local hospital guidelines and recommendations from National Confidential Enquiry into Patient Outcome and Death a tool was created that would gather the information and provide support for managing these patients safely.
Results: A new document, to be incorporated into the hospital surgical day case pathway, that helps to manage diabetic patients had been implemented. The document gathers information regarding last meal, blood sugar monitoring whilst in hospital and provides a step-by-step flow chart to support nursing staff in what to do should they encounter a patient who is hyper/hypo glycaemic prior or post procedure.
Conclusion: This simple document provides all medical staff with a simple flow chart allowing them to safely manage a diabetic patient with abnormal sugars whilst collating all blood sugar recordings so trends can be monitored and acted upon. This along with a teaching program for staff aims to help reduce the numbered of cancelled procedures.
1b4 Post-operative Day Surgery Carers’ Service Evaluation
Aaqid Akram, Simon Hennigan, Kim Russon
The Rotherham NHS Foundation Trust, Rotherham, United Kingdom
Abstract
Introduction: The Association of Anaesthetists (AAGBI) recommend that “Following most procedures under general anaesthesia, a responsible adult provide support for the first 24 hours” (1). The aim of this service evaluation was to ascertain how long carers were present post-operatively, explore if patients felt this was enough time and identify any procedures where patients felt that a carer for 24 hours may be unnecessary.
Method: All adult patients attending the Rotherham NHS Foundation Trust (RFT) Day Surgery Unit, during November/December 2018, were invited to participate. A telephone questionnaire ona standardised data collection sheet was conducted 2 to 28 days post-procedure.
Results: 99 patients provided responses with 100% confirming overnight carer presence. 73 patients had a carer present for 48 hours or less. No procedures were identified with universally low requirements for post-operative care. Some patients felt they needed better access to post-operative healthcare for pain relief or longer carer support. Patients with non-relative carers felt they had less carer support than desired.
Conclusions: RFT patients were conforming to AAGBI recommendations regarding minimum duration of carer presence. Patients undergoing Laparoscopic cholecystectomy & shoulder arthroscopy reported the longest times to regaining independence.
RFT patient information leaflets require revision to enable realistic expectations of the duration of carer presence.
Further data collection on targeted procedures is needed to assess if less than 24 hours carer support is feasible.
Reference
1. AAGBI & BADS. Day case and short stay surgery: 2. Anaesthesia. 2011 May;66(5):417-34.
1b5 Marginal Adjustments for Maximal Gains in Vascular Day Case Anaesthesia
Richard Bentley, Linda Waddilove, Jenny Sainsbury, Rita Singh
Freeman Hospital, Newcastle upon Tyne, United Kingdom
Abstract
Background: Arterio-venous fistula (AVF) formation is a common surgical procedure, which is associated with low rates of post-operative complications and is performed as a day case (DC) procedure in many institutions. We identified that patients undergoing AVF surgery were frequently admitted to hospital the night before surgery and being kept as in-patients post-operatively.
Methods: We performed retrospective analysis of the AVF formation procedures performed at our centre over a 2 year period, with data collected for 12 months either side of a change in our practice. We made changes to the management of AVF patients, aiming to reduce in-patient length of stay (LOS) and increase the number of day case procedures. Changes implemented included the introduction of a regional anaesthesia service for the list, altering the method of listing patients for surgery, streamlining the discharge process with checklists, introducing patient information leaflets and education of the multi-disciplinary team.
Results: Records of 183 patients were examined in total; 74 before change of practice and 109 afterwards. We demonstrated a reduction in patients’ mean LOS from 3.95 days to 1.54 days. DC rate improved from 14% to 43%. Patients discharged within 24 hours of surgery increased from 62% to 84%.
Conclusion: Reduction in LOS and increasing DC rates has many potential benefits including reduced strain on hospital beds (and less procedure cancellation), cost reduction by reducing bed days, improved patient satisfaction, reduced risk of nosocomial infection, better throughput of patients, reduced anaesthetic time/overall theatre time and reduced waiting times for surgery.
1b6 Plastic recycling and beyond
Adrian Nunn, James Rooke
West Suffolk Hospital, Day surgery unit.IP332QZ, Bury St Edmunds, United Kingdom
Abstract
Objective: In one of our audit meetings it was brought to light that:
- A large amount of plastic waste was being produced by our day surgery unit.
- Hand scrub bottles in theatre had a high residual scrub volume.
- Large amount of Balanced Salt Solution (BSS), containing a very minute quantity of adrenaline, had to be disposed as pharmaceutical waste because of added adrenaline.
Method: We ran three parallel projects at our unit.
- We identified the waste that should and shouldn’t go into each bin and educated the staff via posters, corridor conversations and staff news.
- Hand scrub bottles were fitted with new pumps so that we could use all the liquid and then recycle the empty bottles.
- We contacted our local water authority and got approval to dispose of the BSS with adrenaline through our sluice.
Results: We have substantially reduced the amount of plastic waste entering our general and medical waste streams.
Fitting new hand pumps resulted in a saving of £1600pa.
Eye theatre pharmaceutical waste bins now no longer reach capacity or weight limit. 25 litre bins now take in excess of three months to fill as opposed to 2-3 weeks before we started our project.
Conclusion: We could implement this project successfully as we educated and engaged the staff right from the start. We have managed to streamline our waste so that significant amount of it can be recycled. Lots of new ideas are pouring in and we continue to introduce these in our daily practice.
Paper Session 2a: Surgery/Management
2a1 Retrospective Audit Examining On-The-Day Theatre Cancellations
Sanjeev Kotecha, Achal Khanna
Milton Keynes University Hospital, Milton Keynes, United Kingdom
Abstract
INTRODUCTION: The aim of this audit is to evaluate on-the-day (OTD) theatre cancellations at Milton Keynes University Hospital (MKUH) and to identify the reasons behind these cancellations.
METHOD: All elective patients undergoing surgery in the General, Colorectal and Breast specialties over a 6-month period were included. 195 patients were identified. The reasons behind these cancellations were then ascertained using the electronic patient record system. Cancellations were defined as either avoidable: insufficient time, medication issues, not fasted; or unavoidable: bed availability, did not attend (DNA), unwell, surgical cancellation, self-cancellation.
RESULTS: 40% of cancellations were OTD cancellations (78/195). Of these, 89.7% (70/78) were considered to be unavoidable: the most common reasons being bed availability (27/70) and DNAs (14/70). 10.3% (8/78) of OTD cancellations were deemed to be avoidable.
CONCLUSION: OTD theatre cancellations account for significant financial burden across healthcare systems worldwide. Their unpredictable nature exacerbates wasted time of theatre staff and resources. The implementation of measures to reduce OTD cancellations, especially avoidable ones, would lead to increased efficiency and cost-effectiveness. Certain unavoidable OTD cancellations, such as bed availability and DNAs, are also areas worth targeting.
2a2 Reasons for same-day cancellation in a dedicated Day Surgery Hospital: A two year prospective study
Alan Askari, Nuha Ahmed, Ratna Makker, Amjid Riaz
West Hertfordshire Hospitals NHS Trust, Watford, United Kingdom
Abstract
Introduction: Thousands of elective day-case procedures are cancelled in the NHS annually on the day of surgery resulting in significant financial and strategic loss. The aim of this study is to determine the rate of cancellations and identify contributing factors in order to minimise these rates.
Methods: Hospital data was collated on patients undergoing elective-day case surgery across all surgical specialties at our institution over a 2-year period from 1/9/2015 to 31/08/2017. Reasons for cancellation were categorised as due to patient factors, hospital, administration/organisational factors. The data was collected prospectively.
Results: A total 1,692 cases were cancelled on the day of surgery (8%). The majority were Orthopaedic (32.1%, n=543/1,692), Ophthalmology (26.4%, n=446/1,692) and General Surgery cases (14.9%, n=252/1,692). The median number of cancellations were 75 per month. Cancellations were lower in the summer months of July and August (112 and 134 respectively, P=0.03). The majority of patients were cancelled due to patient reasons (65.2%, n= 1,104/1,692); either patient did not attend/changed their mind on day, acute infection/poor diabetic control, blood pressure control (26.3%, n=445/1,692). Approximately 34.8% (n=588/1,692) were cancelled due to hospital/administrative factors such as non-functioning equipment, lack of bed/staff and medical issues which were previously known about and should have been resolved at pre-assessment.
Conclusions: Approximately a third of cancellations of elective day-case procedure on the day of planned surgery are due to hospital factors, which are avoidable. Better communication between pre-operative assessment clinics, patients and theatre staff, is vital in reducing this.
2a3 Service evaluation of parent bleep for children having day surgery at Rotherham Foundation Trust Hospital
Gaynor Rollin, Thomas Pinnell, Kim Russon
Rotherham Foundation Trust, Rotherham, United Kingdom
Abstract
Introduction: The purpose of this evaluation was to obtain feedback from parents using this service. The accompanying parent is given the bleep upon leaving their anaesthetised child. Recovery staff bleep it when their child can return to the ward.
Bleeps were initially introduced to day surgery theatres to improve efficiency of recovery and improve patient, parent and staff experiences. Having the bleep means: Parents don’t need to remain on the ward awaiting a call from theatres, Recovery staff do not have to wait for the ward to answer the telephone, Ward staff had fewer phone calls and don’t have to find parents when their child is ready.
Methods: Parents given a theatre bleep were given a questionnaire to be returned on discharge.
Results: The bleeps were used 201 times 1/11/18-28/2/19 for the following theatres: Emergency(23%); Trauma/Orthopaedics(25%), Maxillo-facial/ENT(23%), Day surgery(21%), other(8%).
26% of questionnaires were returned. 100% parents reported they felt that they could have left the ward if they had wanted to whilst their child was in theatre (57% did leave the ward). All parents reported feeling reassured that they could be contacted using the bleep (91% very reassured). 91% of parents felt the time they waited outside theatre after the bleep had sounded was reasonable; 9% thought it was too long. 98% of parents reported that the instructions given with the bleep were easily understandable.
Conclusions: This evaluation shows good use of the bleeps with positive experience reported by parents.
2a4 . Unplanned admissions following day case laparoscopic cholecystectomy
Kelly-Anne Ide, David Bunting, David Sanders
North Devon District Hospital, Barnstaple, United Kingdom
Abstract
Introduction: Day case laparoscopic cholecystectomy accounts for a significant proportion of the general surgical workload. It was noted that an unexpectedly large number of patients were being admitted following cholecystectomy in North Devon District Hospital so an audit was conducted to discover the reasons for the unplanned admissions and to identify any preventable factors. The British Association of Day Surgery and Royal College of Anaesthetists suggest a target rate of 2% for unexpected overnight stays after laparoscopic cholecystectomy.
Methods: A data collection tool was designed and placed in the Day Surgery Unit. Any unplanned admission following laparoscopic cholecystectomy and the reason for admission was recorded. from 01/02/2018 to 31/10/2018.
Results: 180 day case laparoscopic cholecystectomies were performed, with 26 (14.4%) unplanned admissions. 24 (92.3%) of these were acute cholecystectomies. Reasons for admission were:
- Co-morbidities – 1 (3.8%)
- Pain – 3 (11.5%)
- Active infection found intra-operatively – 3 (11.5%)
- Converted to open procedure – 5 (19.2%)
- Complexity of surgery – 6 (23.1%)
- Drain in situ – 8 (30.8%)
Conclusions: On review of the reasons for admission the majority of cases were deemed clinically appropriate and non-preventable. Post-operative pain and co-morbidities were identified as potentially preventable reasons for admission. These factors were responsible for unplanned admissions in 4 (2.2%) of the 180 cholecystectomies performed which is in line with current targets. It is, however, acknowledged that we perform a large number of acute cholecystectomies and as such a higher admission rate may be expected.
2a5 Day Case Laparoscopic Cholecystectomy in East Africa
Imogen Cullen1, Liam Horgan2, Fadlo Shaban3, Oroog Ali3, Daudi Wapalila4, Mercy Elinisa5, Jamil Suleiman6
1 Newcastle University, Newcastle Upon Tyne , United Kingdom.
2,3 Northumbria Healthcare Trust , Newcastle Upon Tyne , United Kingdom.
4,5,6 Kilimanjaro Christian Medical Centre, Moshi, Tanzania, United Republic of.
Abstract
Introduction: Northumbria Healthcare has fostered a 20 year relationship with Kilimanjaro Christian Medical Centre (KCMC) in Tanzania allowing KCMC to provide expert laparoscopic surgery since 2005. In 2017, a day case laparoscopic cholecystectomy (LC) service for KCMC patients was established. The aim of this research is to evaluate the service and investigate the barriers to its implementation.
Methods: Firstly, all patients who underwent LC’s in KCMC since 2017 were identified. The demographics, day case rate, complications and conversions to open were recorded. The second part involved a patient telephone questionnaire to gain insight into patient perspective of day case service. Finally, KCMC staff interviews were conducted to determine their opinions on barriers to providing a day case service at KCMC.
Results: Of the notes analysed thus far, 82 patients were planned for day case and 55 (67%) were discharged as day case. For 16 (59%), no reason was identified for cancellation of planned day case, 6 (22%) were due to intra-operative complications or conversions and 5 (19%) were due to post-operative symptoms. Of the successful day cases, 3(5%) developed complications with one readmission. Of the 26 patients interviewed so far, 24 (92%) were ‘Extremely Satisfied’ with the service and 26 (100%) would recommend it to their relatives. All data collection will be complete by 28th May.
Conclusions: Day surgery is safe, achievable and beneficial in low resource hospitals such as KCMC. Working with developing countries to understand the barriers preventing day surgery is key in overcoming such obstacles.
2a6 Management of postoperative urinary retention in day surgery utilising the international prostate scoring system
Judith Spalding, Caroline Wilson , Julie Gallagher, Pattabiraman Maheshkummar, Benjamin Fox
Queen Elizabeth Hospital Kings Lynn, Kings Lynn, United Kingdom
Abstract
Introduction: We initiated a quality improvement project where we improved upon our existing bladder management pathway with the addition of the International Prostate Symptom Score (IPSS) for selected male high-risk patients, a novel approach that has not been done before.
Methods: Plan: In 2013 we identified our existing bladder management pathway left a group of high-risk patients in need of either a prolonged stay until discharge and/or 48 hour catheterisation.
Do: In 2014 we implemented the IPSS bladder pathway and conducted an IPSS on high-risk patients who had a residual bladder volume of <400ml. An IPSS >17 led to 48 hours catheterisation. IPSS less than <17 led to discharge without catheterisation.
Study: We prospectively collected data on all patients who were managed using this system.
Act: We found that the service improvement was a positive success and have continued with the service, continually adding and improving upon it.
Results: After initiation of the service in 2014 we analysed the case records of 148 male patients. We prevented 46 patients from having a 48-hour catheter and expedited the discharge of 102 patients.
Conclusions: We have presented a summary of a 5-year quality improvement project that follows a continuous Plan Do Study Act loop. This pathway is the first that we are aware of that incorporates the IPSS.
Limitations of this project include the obvious gender gap that exists and we are looking at adopting a female modification to IPSS.
Paper Session 2b: Anaesthetics
2b1 Is day case total hip replacement feasible, safe and acceptable? Experience of a pilot project.
Anne-Marie Bougeard, Michael Kent, Claire Blandford, Alexandra Alen, Mary Stocker
Torbay and South Devon NHS Foundation Trust, Torquay, United Kingdom
Abstract
Introduction: Over 105000 elective total hip replacements (THR) were performed in England and Wales in 20181, a year when NHS England suspended much of non-urgent elective orthopaedic surgery due to capacity pressures2. Our unit has had a day surgery pathway for unicondylar knee replacement3 since 2011, and we wished to apply the same principles of safety, feasibility and acceptability to selected THR patients.
Methods: We process mapped our inpatient pathway, including audit of ward interventions within the first 24 hours. We adapted our current anaesthesia and analgesia protocols. Inclusion criteria included: ASA 1-3, BMI <30kg/m2, age <75. They were consented for and underwent a planned day case procedure. Our orthopaedic outreach team followed patients up on days 1, 2, and 7 or 10. We collected satisfaction scores and qualitative data on experience.
Results: We have performed 12 planned day case THRs, with no failed discharges, readmissions or complications. Patients were all ambulant by the early afternoon and discharged home before 1900hrs. Satisfaction scores were high and pain was mild or moderate only.
Conclusion: This pilot study shows day case THR to be a feasible, safe and effective option for selected patients. We have demonstrated high levels of patient satisfaction, 100% successful discharge rate and no readmissions or complications. We plan to use this pathway to increase our day case THR rates as well as improve our inpatient processes to benefit our patients and the organisation.
2b2 Same day discharge for “hot” laparoscopic cholecystectomies
William Hare, Theresa Hinde, Kirk Bowling, Mary Stocker
Torbay Hospital, Torquay, United Kingdom
Abstract
Introduction: Urgent laparoscopic cholecystectomies constitute a significant proportion of emergency work at our trust. Evidence in recent literature demonstrates improved patient outcomes and organisational financial benefits in operating on the initial admission. Our unit has incorporated suitable ‘hot’ cases into an existing emergency ambulatory surgery pathway.
Methods: Patients identified as surgically and socially suitable were operated on in the day surgery unit via our recently established emergency ambulatory pathway, aiming for same day discharge.
A database search, and, where necessary, a review of clinical notes of a 22 month period was performed to evaluate caseload and factors enabling successful management as a day case.
Results: We undertook 67 emergency ambulatory laparoscopic cholecystectomies over 22 months. 29 (43%) of these were successfully discharged on the same day. This generated potential cost savings of at least £23,200 in overnight admission costs (£400 per night) and £120,540 in saved emergency theatre time (£15 per minute)
Factors that impacted positively on discharge rates were origin of admission (direct to DSU from home), operation timing (morning cases) and duration of surgery.
The most common reasons for admission were surgical complication and late finish. 84% of respondents reported general feeling of ‘good’ or ‘very good’ when managed through the DSU.
Conclusions: We have demonstrated that management of emergency laparoscopic cholecystectomies via our ambulatory pathway, although challenging, is possible and can result in excellent patient experience with financial benefits to the organisation. We intend to use our experience to improve discharge rates.
2b3 ‘Here today, gone today’- evaluating an emergency ambulatory pathway
Ciska Uys, Hare William , Hinde Theresa , Mary Stocker
Torbay and South Devon NHS Trust, Torquay, United Kingdom
Abstract
Introduction: Minor or intermediate surgical procedures account for a significant proportion of booked emergency cases. Implementing a novel day surgery pathway for appropriately selected cases has improved patient flow and experience, saved theatre time and decreased bed occupancy.
Methods: Vacant but staffed day surgery lists were highlighted to emergency teams in advance. At daily handovers teams identified patients fulfilling emergency ambulatory surgery criteria. Stable patients were sent home and instructed to return to the day surgery unit (DSU) for their surgery. The aim was surgery and discharge via the DSU pathway. Some patients underwent surgery in main theatres, but same day discharge via DSU.
Results: Over 22 months 442 patients (18 children, 424 adults) underwent emergency surgery via the ambulatory pathway. This freed 386 hours of emergency theatre time, saving around £347,280.
370 patients (83.7%) were successfully discharged same day. 301 patients (68.1%) avoided a pre-operative night stay. This saved 671 bed days with estimated cost of £268,400.
Next day, 90% of 257 patients (58.1%) followed up by telephone reported feeling ‘good’ or ‘very good’.
Conclusions: Streamlining our ambulatory pathway for emergency patients has reduced cost, saved emergency theatre time and maintained patient satisfaction. The pathway’s success is enjoyed by surgical, anaesthetic, theatre and recovery teams. Theatre culture has changed to expect ambulatory list availability and the pathway is used when elective list capacity allows for ad hoc emergencies. With growing confidence in the process, more complex procedures (gynaecological laparoscopies, laparoscopic appendicectomies/ ‘hot’ cholecystectomies) are undertaken as ambulatory cases.
2b4 Developing a teaching module for day surgery Preoperative Assessment staff
Rachel Tibble1, Wendy Holmes Taylor2, Cheryl Webster1, Leah Frame3, Angela Gent
1Royal Derby Hospital, Derby, United Kingdom. 2Royal Derby Hospital, derby, United Kingdom. 3Royal Derby Hospital, Derby, United Kingdom
Abstract
Introduction: BADS ratifies specifically trained preoperative (POA)staff working within daycase areas for best day surgery outcomes. New staff or those covering absence are commonplace. We postulated a specific daycase training module for these staff would retain day surgery success rates especially for complex patients.
Methods: A working party updated POA guidelines at Derby. Guidelines specific to day surgery were identified and linked to the aims set for daycase POA. All POA nurses listed topics they wanted addressing. Dedicated teaching time was identified for maximum attendance with end of course feedback.
All POA staff had access to the course.
Results: Topics identified were ; complex patients and daycase suitability (using anaesthetic led clinics). obstructive sleep apnoea, high body mass index, difficult airways, diabetes, cardiac failure management, chronic obstructive pulmonary disease.ischaemic heart disease, pacemakers, paraumbilical hernias, renal access, urology patients, chronic pain, cirrhosis, antihypertensives and anticoagulants, neuromuscular/multisystem disorders
30 minute interactive teaching sessions from a consultant anaesthetist were developed and implemented
Conclusion: Topics were devised by POA nurses to cover areas of need. Input from experienced day surgery POA staff delineated differences between day surgery and inpatient POA with emphasis on sending patients home safely post operatively
Teaching was implemented by a consultant anaesthetist interested in day surgery POA.
Teaching is currently ongoing and review of the process should allow revision and improvement to maintain expertise in day surgery POA.
2b5 A comparison of day case pathways demonstrates the benefits of a dedicated day surgery unit
Alexandra Humphreys, Gregory Warren, Jonathan Carter, Mary Stocker
Torbay and South Devon NHS Foundation Trust, Torbay, United Kingdom
Abstract
Introduction: Patients undergoing day case operations in our trust are managed via one of two pathways:
- Admission, surgical procedure, recovery and discharge all in dedicated Day Surgery Unit (DSU)
- Admission, surgical procedure and first stage recovery via main inpatient theatres (IT), then transfer to DSU for second stage recovery and discharge.
We aimed to establish the difference in time taken for patients to undergo the same operation via each of the two pathways.
Methods: Three routine elective operations were monitored: laparoscopic cholecystectomy (LC), laparoscopic hysterectomy (LH), and open repair of inguinal hernia (IH).
The entire patient journey was observed. The time that each patient spent at each stage, and any delaying factors, were noted. Surgical procedural time was excluded.
18 patient journeys were monitored.
Results: The mean time taken for every step of the pathway was shorter in the patients on the DSU pathway.
From sending to arrival in second stage recovery, the mean duration for patients on the DSU pathway was less by:
- LC – 50 minutes
- LH – 32 minutes
- IH – 24 minutes
Combined, 9 patients undergoing their procedure via DSU saved a total of 5 hours and 19 minutes of direct clinical care.
Conclusions: Managing patients in a dedicated DSU results in less time taken for direct clinical care, which has associated financial savings for the trust. The increased turnover should enable more patients to be managed on an individual list.
2b6 Chest Wall Blocks - Still a Luxury in Day-Case Breast Surgery?
Araz Pourkashanian, Rahul Bandopadhyay, Madan Narayanan, Isabella Karat
Frimley Park Hospital, Camberley, United Kingdom
Abstract
Introduction: The benefit of regional anaesthesia in day case and breast surgery is well documented. For mastectomies, current recommendation from The British Association of Day Surgery (BADS) Directory of Procedures sets a standard of 15% day-case rate and 70% single-night stay. The audit aim was to identify the proportion of patients receiving regional anaesthesia for mastectomy at our institute and establish whether this had an impact on perioperative opioid requirements and total length of hospital stay.
Methods: Retrospective data was collected for consecutive patients having mastectomies over a 12-month period at Frimley Park Hospital, UK. Electronic anaesthetic notes and drug charts were reviewed for data collection.
Results: 52 mastectomies were performed during the audit period. 27% of these patients had a regional anaesthetic technique as part of their intraoperative care with paravertebral and erector spinae blocks being the most commonly performed (36%). Time to first post-operative opioid administration was longer in the regional group, with total 24-hour opioid consumption being equivalent in both groups. At our institute the proportion of patients being discharged within 23 hours was 6%, and 62% of patients had a single-night stay. The regional group had a shorter average hospital stay.
Conclusion: With the introduction of a new enhanced recovery mastectomy protocol incorporating regional anaesthesia as a standard of care, we aim to improve patients’ perioperative experience and increase the percentage of 23 hour ambulatory non-reconstructive breast cancer surgery. This pilot audit will act as a baseline for further comparative audits and improvement in perioperative care.
Posters
P1 The Scope for Emergency Day Surgery in the Surgical Management of Abscesses
Erin Dawson1, Matthew Blaylock1, Lisa Massey2,1, Rob Bethune2
1University of Exeter, Exeter, United Kingdom. 2Royal Devon and Exeter Hospital, Exeter, United Kingdom
Abstract
Aim: We aim to implement a long-term, sustainable, ambulatory surgical abscess pathway that utilises pre-existing day surgery ward infrastructure. In doing so, we hope to provide a shorter stay for patients thus reducing inpatient bed usage. Previous studies indicate there is no significant difference in clinical outcomes between inpatient and ambulatory care.
Methods: Patients were identified by surveying admissions lists from a single surgical admissions unit. Data were collected prior to the introduction of ambulatory care (October 2017-April 2018) and seven months after the change (April 2018-November 2018).
Results: Prior to the introduction of the pathway, all patients requiring incision and drainage received standard inpatient care. Since the introduction of the new pathway, 43 of 163 patients (26%) have been treated within a true ambulatory setting. The mean length-of-stay for true ambulatory patients was 10.0hrs (SD±5.1) whereas for inpatients it was 23.4hrs (SD±17.5). Unpaired t-test analysis demonstrated a significant reduction in length-of-stay for an ambulatory patient compared to an inpatient (n=149 p<0.000001).
Conclusion: Our results indicate that it is feasible to use the new ambulatory pathway for a significant proportion of emergency abscess patients, using the strong platform we have to assess the success of further interventions.
P2 Day-Case Mastectomy Target- Achievable and Sustainable for the Future of the NHS
Claudia Wilson, Gwen Bromley, Annie Chan, Mujahid Pervaz
Queen Elizabeth Hospital , Gateshead, United Kingdom
Abstract
INTRODUCTION: Mastectomy remains a commonly used surgery in the management of breast cancer. National guidelines now recommend that we aim to carry out 50% of mastectomy procedures as day-cases. This project assesses how achievable the recommended day-case mastectomy (DCM) rates are within our trust, how DCM rates can be improved and whether this can be applied to other trusts.
METHODS: All mastectomy cases were evaluated from February to August 2018 at a district general hospital following an initial audit in 2017 identifying DCM rates much lower than the national 50% target. We undertook retrospective analysis of electronic records of all patients who underwent mastectomies.
RESULTS: 82 patients were included for analysis and the average age was 58. Overall 54.9% had their mastectomies as day cases, including patients with immediate reconstruction and all nodal procedures. 62% of patients who underwent simple mastectomies had their procedures done as day-cases compared to 35% of patients in 2017. Mean length of stay decreased for all types of mastectomies over this period compared to the previously audited period.
CONCLUSION: The rate of day-case mastectomies has improved significantly from 2017 to 2018. This has been attributed mainly to a drive to adjust patient expectations. This has had huge financial implications in the trust. Further work should be done nationally with patients and clinicians to make day-case mastectomies a part of routine surgical practice.
P3 “Dying of thirst?” Perioperative fasting in adult patients undergoing day case surgery
Roisin Baker, Somasundaram Jeyanthan
Queen Elizabeth Hospital , Birmingham , United Kingdom
Abstract
Introduction: To reduce the risk of aspiration of gastric contents, patients have traditionally been denied food and clear fluids for 6 and 2 hours respectively prior to general anaesthesia. Much attention has been paid to reducing fasting times in children, who are more susceptible to dehydration and hypoglycaemia. Children are now encouraged to drink clear fluids until 1 hour prior to elective anaesthesia. As well as reducing patient discomfort, relaxing fluid fasting in adults may reduce pre-operative anxiety and post-operative nausea and vomiting. The aim of this study was to identify current fasting practice for adult patients undergoing day case surgery.
Methods: Data was collected prospectively over a 4-week period. Patient reported fasting times for solids and liquids and time of anaesthetic induction were recorded.
Results: A broad case-mix of 45 surgical patients was studied. Fasting times for clear fluids ranged from 3 hours and 5 minutes to 17 hours and 40 minutes (median time 11 hours and 20 minutes). Fasting times for solids ranged from 7 hours and 5 minutes to 22 hours and 40 minutes (median time 15 hours and 5 minutes).
Conclusions: Our study demonstrates that adult patients are being subjected to unnecessarily prolonged fasting times. This is likely to result in patient discomfort, increase the risk of nausea and vomiting and even perioperative renal dysfunction. There is scope to improve current practice through patient and staff education, updating current local policy and highlighting patients who can safely drink at the daily morning team brief.
P4 Managing patients with challenging behaviour for day surgery; use of a Vanguard mobile theatre.
Anna Lipp
Norfolk and Norwich University Hospital, Norwich, United Kingdom
Abstract
Patients with challenging behaviour which may present a risk to staff and other patients pose a variety of issues when they need surgical procedures. We have recently managed 3 admissions for such patients and wish to share the learning from our experiences.
Planning for the admissions focussed on reducing triggers for the patient’s behaviour and ensuring safety for the patient, staff and hospital users. Prior to admission the patient’s carers visited the hospital to walk through the pathway. The identified triggers for challenging behaviour in each case were
- Waiting
- Unfamiliar environments
- Unfamiliar people
- Close contact and interventions
To minimise risks of waiting and contact with unfamiliar people we used the Vanguard mobile theatre which has direct vehicle access with a short walk up the ramp to the anaesthetic room. The area can be easily overseen by security staff and is separate from other patient areas.
A plan for management was agreed with the patient’s carers for each admission and staff rehearsed the key steps. Photographs of the area and staff were used to familiarise the patients in advance. For 2 admissions it was recommended that anaesthetic induction and recovery should take place on the floor where the patient felt secure. A scoop stretcher was used for lifting the first time and “Hoverjack air patient lift” on second occasion and this was rehearsed with manual handling team.
Each admission proceeded uneventfully, and carers were grateful for the planning and use of a suitable environment for the procedures.
P5 Gynaecology Day Case Surgery Pathway in Northumbria Healthcare Trust
Ehab Hafiz, Nalini Munjuluri, Michael Blundell
Northumbria Healthcare NHS Trust, Newcastle, United Kingdom
Abstract
INTRODUCTION: The day-case enhanced recovery pathway has been developed to streamline the patients journey from their initial referral to their recovery from elective day case surgery. This aims to facilitate a more rapid recovery, shortened length of stay and return to normal activity. It will also reduce the trust’s unplanned admission rate for day-case surgery, to alleviate inpatient bed pressures and improve patient satisfaction.
METHODS: The trust have developed a pathway for all day case surgeries which includes criteria for patient selection, patient counselling & consenting , optimisation and Pre-assessment. Following the Royal College of Obstetricians and Gynaecologists Enhanced Recovery Pathway and Patient Reported Outcome Measures.
RESULTS: Out of 2422 day case surgeries performed in 2018,113 required stay overnight (4.7%). Example of patient feedback “All positive following the operation, my lifestyle has improved dramatically. I would like to thank the NHS for making a huge difference to my life.”.
CONCLUSION: Increased successful planned day case surgeries . High-quality patient care with excellent patient satisfaction. Day surgery is the standard pathway of care for many complex patients and procedures traditionally treated through inpatient pathways.
P6 The use of botulinum toxin in keloid management: A literature review
Catrin Sohrabi1, Ioannis Goutos2
1Barts and The London School of Medicine and Dentistry, London, United Kingdom.
2Centre for Cutaneous Research, Blizard Institute, Queen Mary University of London, London, United Kingdom
Abstract
INTRODUCTION: Keloids represent a challenging clinical entity resulting from pathophysiological processes such as fibroblastic hyperactivity. Despite the presence of various management strategies including intralesional/extralesional excision and corticosteroid injection, however, the ideal therapeutic approach has yet to be reached. To address this, botulinum toxin (BXT) has emerged as a promising approach to managing keloids owing to its ability to reduce the intensity of tensile forces caused by muscle pull during the wound healing process, and of its ability to modulate the cell-cycle distribution of fibroblasts derived from human hypertrophic scars.
METHODS: 87 total articles were identified following a literature search of PubMed Medline, Embase, and Web of Science with appropriate search terms. 11 studies were included for analysis and classified according to the Joanna Briggs Institute Levels of evidence.
RESULTS: Various level 2 studies confirm the additive and statistically significant value of BXT in alleviating pain and itch when compared to intralesional steroids alone. Two level 2 studies appraise the value of BXT as a post-operative keloid management adjunct. A notable advantage of BXT as a primary agent is of the lack of significant side-effects when compared against local intralesional steroid.
CONCLUSIONS: The adoption of BXT in keloid scar management has a number of potential advantages by virtue of its ability to confer chemoimmobilisation to the underlying tissue musculature. Having displayed good therapeutic outcomes and superior symptomatic benefit when compared to steroids, however, further high-quality studies are awaited to delineate the long-term role of BXT in keloid management protocols.
P7 Retrospective Audit Assessing the Completion Rate of the World Health Organisation Surgical Safety Checklist
Sanjeev Kotecha, Achal Khanna
Milton Keynes University Hospital, Milton Keynes, United Kingdom
Abstract
INTRODUCTION: The World Health Organisation (WHO) Surgical Safety Checklist was developed in order to enhance surgical outcomes. Milton Keynes University Hospital (MKUH) has developed its own modified version. The purpose of this audit is to determine the extent to which this checklist is being completed.
METHOD: Patients undergoing procedures by the General Surgery Department over a 2-month period were included. The electronic patient record system was used to analyse each individual’s checklist. MKUH’s version comprises 30 distinct components that are categorised into one of the 3 primary categories: Sign In; Time Out; Sign Out. The number of incomplete components for each patient was then calculated.
RESULTS: 84 patients’ checklists were assessed. Only 33.3% (28/84) of checklists were fully completed i.e. two-thirds of checklists were incomplete. In the remaining 56 checklists, there were a total of 156 missing components: an average of 2.79 per checklist. 2 particular checklists were missing as many as 10 components.
CONCLUSION: Given that the WHO Surgical Safety Checklist was designed in an attempt to improve patient safety by maximising consistency across all surgical procedures, it would be sensible to attempt to improve MKUH’s checklist completion rate by implementing relevant changes and re-auditing.
P8 Should we be performing Day Case Laparoscopic Cholecystectomy after 3pm?
Nadhirah Kahar1, Joanna Aldoori2, Amro Alamassi1, Laura Whittaker2, Sally Dunlop2
1Airedale General Hospital , Keighley , United Kingdom.
2Airedale General Hospital , Keighley, United Kingdom
Abstract
Introduction: Laparoscopic cholecystectomy (LC) is a common daycase procedure. The British Association of Day Surgery (BADS) Procedure Directory[i]sets out national performance targets for the number of LCs treated as day cases. We aimed to assess if operation time predicted unplanned inpatient admission.
Methods: An anonymised retrospective review of all patients undergoing LC was undertaken over a 6-month period. Data was obtained from multiple sources: discharge letters and the theatre data manager.
Results: 113 LCs were performed over a 6-month period, 5 (4%) were planned admissions. The zero night stay for Day Case Laparoscopic Cholecystectomy (DCLC) was 56%, which lies within the top 50% of current national performance but is below the BADS target of 75%. Of the planned DCLC there were 47 (42%) unexpected admissions. The unexpected admission and zero stay groups were matched in age and gender. Average age 54 (22 to 87) with 76% female in the zero stay group compared to 51 (18 to 81), with 77% female in the unplanned admission group. In the day zero stay group. 3 (10.4%) patients underwent operations between the hours of 15:00 to 18:00 compared to 14 (32.5%) in the unplanned admission group (P=0.0069).
Conclusion: The timing of operation of DCLC predicts inpatient admission; our data suggests that DCLC should not take place after 3pm. A small proportion of patients were planned admissions suggesting that there is a default for clinicians to book patients undergoing LC as DCLC, which may be inappropriate.
Reference
[i] BADS Directory of Procedures 5th Edition
P9 Re-audit of Unplanned Admissions following Day Surgery at the Norfolk and Norwich University Hospital
Elizabeth Herbert, Rachel Morris, Samuel Fletcher
Norfolk and Norwich University Hospital, Norwich, United Kingdom
Abstract
Introduction: Unplanned admissions (UA) following day surgery (DS) represent a costly dilemma. They reduce the availability of acute hospital beds and negatively impact the lives of patients. UA rates are used as performance indicators for DS and the Royal College of Anaesthetists (RCOA) advises they should be <2% overall.
Method: We performed a retrospective study and re-audited UA following DS and recovery at the Norfolk and Norwich University Hospital’s Day Procedure Unit (DPU) in August 2018. Data was collected from paper bed request forms and electronic discharge summaries.
Results: In August 2018, 1372 DS patients were recovered in DPU. There were 57 UA, which equates to 4.15% (vs 1.1% 2017).
Urology had the highest percentage of UA (35% vs 30% 2017), followed by general surgery (15.8% vs 32% 2017) and gynaecology (12.3% vs 6% 2017).
The reasons for UA were manifold. The most common were that the surgery was more extensive than planned (15.8%) (no definitive 2017 data), bleeding (10.5% vs 5% 2017) and urinary retention (10.5% vs 11% 2017).
Conclusions: Our August 2018 DPU UA rate was double the RCOA’s recommended <2% and four times the 2017 rate of 1.1%. However, not all DS cases are processed by DPU. The fact that the highest percentage of UA were due to surgical reasons may reflect the evolving nature and increasing complexity of DS. We plan to extend our study over a six-month period, to more reliably establish UA rates and patterns, with the aim to design targeted perioperative protocols.
P10 Unplanned Day Case Surgery Admissions from 2008 – 2018 in Rotherham Foundation Trust Hospital
Lorna McEwan1, Kim Russon2
1Rotherham Foundation Trust Hospital, Rotherham, United Kingdom.
2Rotherham Foundation Trust, Rotherham, United Kingdom
Abstract
Introduction: In-line with NHS Improvements national drive, the proportion of elective surgical procedures performed as day-cases is continually increasing. However, as the complexity procedures performed as day-cases and patients’ comorbidities increases so too does the risk of unplanned admissions. Unplanned admissions are inconvenient for patients and their carers, additionally it places increased pressure on hospitals (higher costs, loss of acute beds and best-practice tariffs). Therefore, at Rotherham Foundation Trust (RFT) we regularly audit the number and causes of unplanned admissions in order to reduce the rate of unplanned admissions and improve the quality of care delivered to day-case patients.
Methods: The time, procedure and cause of every patient unexpectedly admitted after a day-case procedure was prospectively recorded from 2008-2018, based on the Royal College of Anaesthetists audit compendium.
Results: Since 2008, RFT has performed 4460-6413 day-case surgical procedures annually. The rate of unplanned admission across the years ranges from 2.9%-1.5%. Some common reasons for unplanned admissions include pain, late leaving theatre, bleeding and post-operative nausea and vomiting. Regular auditing identified factors causing admission which targeted departmental education leading to improved practices. For example, the introduction of departmental guidelines and spinal-anaesthetic recipes reduced the rate of urinary retention and prolonged block admissions.
Conclusions: The increasing complexity of day-case patients and procedures increases the risk of unplanned admissions. Indeed, the continual pushing of boundaries may necessitate accepting a higher transfer from day-case pathway to inpatient. This highlights the importance of regularly auditing the rate and reason for admissions to actively manage root-causes.
P11 Why don’t we ask patients to supply their own post-op analgesia - A matter of perspective?
Elizabeth Reynolds1, Carol Makin2
1University of Bristol Medical School, Bristol, United Kingdom.
2The Medical Specialist Group, Guernsey, Guernsey, Guernsey
Abstract
Introduction: We investigated the process of patients acquiring analgesia following day surgery.
Methods: Interviews were conducted with staff and patients involved in prescribing, dispensing and receiving analgesia following day surgery.
Results: Surgeons: Frequently employ local anaesthetic intra-operatively. They do not routinely prescribe discharge analgesia leaving the task to anaesthetists.
Anaesthetists: Prescribe analgesia routinely - paracetamol, ibuprofen and codeine. They are concerned patients cannot be relied on to purchase their own supplies.
Day Ward Nurses: Label and dispense all drugs ordered by anaesthetists.
Pharmacists: Supply pre packed analgesia to the day unit.
Patients: Paracetamol and ibuprofen are commonly taken, codeine rarely. Most are familiar with these analgesics and have supplies at home. They would purchase drugs if instructed.
Conclusions: The aim of post-operative pain management is to ensure patient comfort, enable early restoration to normal activity, minimize side effects associated with analgesia, allow effective self-management of pain at home, and ensure safe, cost-effective use of analgesia1.
If patients acquired their own post-operative analgesia further supplies from the hospital would be unnecessary. Nurses and pharmacists would be relieved of unnecessary work.
Dispensing excess quantities of analgesics, particularly codeine, would be avoided with less waste.
Reference
1 Day Case Surgery. Ed. I Smith, D McWhinnie, I Jackson. Oxford University Press. 2012.
P12 Short stay and day case Hysterectomy patient outcomes when receiving anaesthetic service from a Physician’ Assistant in (Anaesthesia)
Howard Cox
University Hospital Birmingham, Birmingham, United Kingdom
Abstract
Physician’ Assistant in (Anaesthesia) [PA-(A)] have worked in a qualified capacity for the National Health Service (NHS) since 2007.
It is widely recognised that with robust local governance frameworks PA-(A)’s perform extended anaesthetic roles such as Regional Anaesthesia and providing anaesthetic services to patient undergoing major abdominal cavity surgery.
Despite these advance in the PA-(A) practice, there has been no evaluation of patient outcomes with extended role. There equally has been no evaluation of working in a 2 to 1 capacity in major abdominal surgery when the PA-(A) has been the primary anaesthetic provider. This study focuses over a two your period on the work carried out by PA-(A) specifically focussing on patient having elective hysterectomy.
The study elevated Length of Patient Stay (LOS) and post operative complication, be those of an anaesthetic or surgical nature.
The Study recruited 103 cases or which 82 could be successfully use within the study .
It demonstrated there was no adverse outcome in LOS with Laparoscopic Hysterectomy patients mean LOS been 28 hours and open Hysterectomy cases having a mean of 48 hours. This is within keeping in current NHS LOS for Hysterectomy patients.
The spinal anaesthetics undertaken by the PA-(A) in these two group which amounted to 56 patients had a100% success rate and there was only one complication relating to the anaesthesia which was post operative nausea and vomiting.
This study give a useful insight into PA-(A) extended roles and evolving scope of Practice.
P13 Improvement of analgesia prescribing in day surgery patients
Owen Thomas, Katharine Stenlake
Musgrove Park Hospital, Taunton, United Kingdom
Abstract
Introduction: The number and complexity of cases performed in our unit has increased, but so have the numbers of patients requiring rescue analgesia from GPs postoperatively. Our prescription guidance was reviewed.
Methods: Day surgery cases (adults) were classified into 4 categories based on expected post-op pain. These were: none, mild, moderate and severe. An analgesic regime was recommended for each, and this categorization was circulated to senior anaesthetists and surgeons for comment before being widely distributed.
An audit of routine analgesia prescribing was conducted before and after implementation, and GPs contacted for any noticeable change in ‘rescue’ prescriptions required.
Results: The majority of patients purchase the recommended simple analgesia prior to surgery, but additional post-operative analgesic prescribing by clinicians is variable. 87% of patients had none and 40% did not have the recommended analgesia prescribed.
Reasons included clinicians unclear about their responsibility for prescribing, and the complex process of obtaining additional TTOs. Prescription rates were higher for procedures with clear guidance already in place e.g. tonsillectomy.
Post implementation anecdotal evidence suggests an improvement in rates of analgesia prescribing. (Data is still being collected)
Conclusions: A significant percentage of patients having surgery with potential post-op opioid analgesia requirements did not have adequate prescriptions. The introduction of a clear analgesic protocol improved prescription rates for specified operations.
Categorizing operations based on expected analgesia requirements should have a beneficial effect on individual patient’s experience of their day surgery and reduce the burden on local GPs.
P14 Reducing Overnight Admissions Following Planned Day Case Surgery
Sally Dunlop
Airedale General Hospital, Keighley, United Kingdom
Abstract
Introduction: Avoidable admissions following day surgery can cause distress to patients, increase risk of hospital acquired infection and venous thromboembolism. They have a negative financial impact on the hospital due to cost of overnight stay and loss of best practice tariff, along with reduction in bed availability for acute admissions
Method: In summer 2017 our admission rate was unacceptably high at 12%. A thorough review of all admissions over a 3 month period was carried out by a team of medical and senior nursing staff to look for common themes.
Common reasons for admission included
- insufficient time for recovery due to late out of theatre
- not having passed urine
- patient too drowsy / nauseous / in pain
Results: Based on these results, we have implemented numerous work streams, including
- education surrounding criteria not time based discharge
- post operative urinary retention policy allowing discharge home without having passed urine
- “sip until we send” fasting policy to encourage hydration and reduce post operative nausea
- list planning review to achieve day case work earlier in the day
- introduction of fentanyl in place of morphine for rescue analgesia in theatre recovery (recent change effect yet to be analysed)
Our admission rate has reduced to 7% following some of these changes.
Conclusion: A through and ongoing review of reasons for admission is necessary to understand the issue. We continue to attempt to implement flexible opening hours for our day ward and for nurse led discharge into the evening from our inpatient wards.
P15 An observational study to analyse the potential effect of infusion dead space in the surgical and critical care setting
Manraj Sura, Tamsin Rope
London North West University Healthcare Trust, London, United Kingdom
Abstract
Introduction: This study observed current clinical practice to analyse the potential effect of infusion dead space. The importance of this study revolves around the potential for patients to receive suboptimal dosage of prescribed drugs or blood products.
Methods: We conducted a 6 – question survey of nursing staff across two intensive care units (ICUs), four surgical wards, postoperative recovery area and a Postoperative Care Unit (PACU).
Results: Experimental work using administration sets (B Braun Intrafix® SafeSet) found the infusion dead space on average to be 18ml (filling chamber 50% full). 102 surveys were given to nursing staff over a 4 day period with an 81% response rate. Following administration of IV Metronidazole (500mg/100ml) 67% of respondents would not flush the administration set, resulting in the patient not receiving 18% (90mgs) of the infusion. Following administration of IV Paracetamol (1g/100ml) 71% of respondents would not flush the administration set, resulting in the patient not receiving 18% (180mg) of the infusion. Following administration of one unit of Packed Red Cells (average 250ml) 48% would not flush the administration set, resulting in the patient not receiving 7% of the infusion. Following administration of IV Omeprazole (40mg/100ml) 75% would not flush the administration set, resulting in the patient not receiving 18% (7.2mg) of the infusion.
Conclusions: Based on the study results, potentially subtherapeutic treatment could lead to longer, more complicated patient recovery postoperatively and adverse patient outcomes. There is a need for robust national guidelines and increased awareness of intravenous infusion sets’ dead space.
P16 Reducing Perioperative Fasting at The Rotherham Foundation Trust – A completed Quality Improvement Cycle
Ahmed Atewah1,2, Chloe Billingham1,2, Kim Russon1
1Rotherham NHS Foundation Trust, Rotherham, United Kingdom.
2Sheffield Teaching Hospitals, Sheffield, United Kingdom
Abstract
Introduction: A service evaluation in our department in 2017 demonstrated excessive fasting times. Despite local guidance in keeping with the Association of Anaesthetists’ of 2hours for clear fluids 26% of patients had clear fluid fasting time exceeding 6hours.
Prolonged fasting can be detrimental to patients’ experience and health including causing headaches, nausea, increased insulin resistance and an altered acute phase response to surgery.
Studies demonstrate that stomach emptying follows an exponential course, with a half-time(T½) for water approximating 15minutes.
In November 2018, guidelines were introduced to try and reduce excessive pre-operative fasting. Our written patient information was amended to encourage drinking clear fluid until 2hours before. The pre-operative assessment nurses were asked to tell patients that they should actively try and drink water up until 2hours preoperatively. Patients are offered a small glass of water on admission to Theatres admission unit.
We aimed to determine whether there had been a reduction in clear fluid fasting times following this change.
Methods: Clear fluid fasting times for all adult elective surgery cases (including day surgery) was collected over five consecutive days in February 2019.
Results: Data from 117 patients was collected. 15% of patients had clear fluid fasting time >6hours, a 42% reduction from our previous service evaluation. 33% of patients received water on admission. 66% had received clear fluids <4hours before arrival to Theatre. There were no cases of postoperative pulmonary complications.
Conclusions: Our intervention has resulted in a reduction in prolonged fasting. There is still room for further improvement.
P17 Pre-operative waiting, a timely solution
Katharine Hannon, Christopher Roberts
Royal Free Hospital, London, United Kingdom
Abstract
Introduction: The Royal Free Day Surgery unit has been operating since the early 1990s. Typically the unit sees 50-70 patients per day. Day surgery historically involves long waiting times and, although there is no specific guidance on how long patients should wait pre-operatively, we are aware that prolonged waiting times increase patient dissatisfaction and anxiety. With patient satisfaction a key performance indicator of the trust we chose to audit pre-operative waiting times.
Methods: Over the course of two weeks the nurses recorded the time patients arrived in the department, when they saw a nurse, anaesthetist and surgeon and the time they went to theatre using a table the patients kept with them. We cross referenced the patients to the surgical speciality to see areas needing improvement or areas of excellence.
Results: We surveyed 86 patients in a 2 week period, focusing on the elective lists only. The results showed an average waiting time of 3 hours 58 minutes; with patients seen by a nurse within 35 minutes and by a surgeon within 1 hour 11 minutes. The longest waiting time was 9 hours the shortest 1 hour.
Conclusion: Day surgery procedures can involve long waiting times leading to a decrease in patient satisfaction. The plastic speciality had the shortest waiting times, mainly due to the effective staggering of lists, and breast surgery had the longest waiting time. We can use the results to make a case for change and replicate the plastics model across other specialities.
P18 “Routine Preoperative Tests for Elective Surgery” – Audit and Education of Guidelines can Cut the Costs Associated with Unnecessary Tests
Deeksha Arora, Thomas Seddon, Haroon Iqbal, Dinesh Thekkinkkattil
Pilgrim Hospital, Boston, United Kingdom
Abstract
Introduction: Patients undergoing elective operations frequently attend a pre-operative assessment, where a series of tests are performed, each with an associated cost. Guidelines exist to guide the tests required for each grade of surgical severity in patients of all ASA Grades. We performed an audit to evaluate knowledge of and adherence to these guidelines. An educational poster was made and a re-audit performed to see if education helped improve adherence to these guidelines, and assess any cost implications.
Method: Inclusion criteria included patients over 16 attending pre-assessment for elective surgery in Pilgrim Hospital, Boston. A random selection of case notes covering a range of Surgical Specialties were reviewed to see what tests were ordered, whether they were advised under NICE guidelines and what the associated costs were. A poster of the guidelines was subsequently made available in the pre-assessment clinic and the amount of tests ordered and their cost was compared between cycles.
Results: The first audit cycle of 50 patients over 1 month highlighted 44 tests not required under guidelines, with a cost of £632.24, correlating to £75,868.80/year when extrapolated to the number of patients operated on per year in Pilgrim Hospital and £189,672 across the Trust. The second cycle of 100 patients over 8 weeks highlighted 121 unnecessary tests, equating to £372.28 - £22,336.80/year in Pilgrim and £55,469.72 across the Trust. The saving was £53,532/year in Pilgrim, and £134,202/year across the Trust.
Conclusion: Knowledge and adherence to existing guidelines regarding pre-assessment tests has significant cost implications for the NHS.
P19 What are the barriers to daycase TURBT?
Luisa MacDonald, Heidi Salminen, Mustafa Hilmy
York District Hospital, York, United Kingdom
Abstract
Introduction: Transurethral resection of bladder tumour (TURBT) is integral for the diagnosis, grading and treatment of bladder cancer. There has been an increasing drive for day surgery to optimise inpatient capacity, and current policy is to plan patients for daycase TURBT where feasible. This is a re-audit of TURBTs in a district general hospital where previous audit demonstrated 43% discharge rate within 24 hours.
Methods: Retrospective data was collected on all TURBTs from January-December 2018 utilising the hospital’s database. Demographic data included age at operation, American Society of Anaesthesiologists (ASA) grade, tumour size, resection mass and histology, as well as length of stay (LOS).
Results: There were 104 resections including 13 re-resections in 94 patients, with a mean age of 76. 12 underwent an additional procedure at time of surgery. Male to female ratio was 3:1. 50% of patients were ASA 1-2 and 50% ASA 3-4. 79% had a new tumour diagnosis and 16% were undertaken for recurrence. 3.8% were booked as daycases. At re-audit, 9.6% were discharged within 24 hours, increasing to 62.5% at 48 hours with mean LOS 44.4 hours. 57 tumours were solitary and 32 multifocal. Spread of histological grading was 8.2% G1, 38% G2 and 54% G3 respectively.
Conclusions: The previous daycase discharge rate has not been replicated at re-audit. This may be due to booking as inpatient rather than daycase procedures, increased rate of G2/3 tumours, and higher ASA grades. Better implementation of the pre-existing pathway, and further audit, is required.
P20 Operation note documentation in laparoscopic cholecystectomies in a District General Hospital.
Polly Estridge1, William Ward2, David Bunting1
1North Devon District Hospital, Barnstaple, United Kingdom. 2Royal Devon and Exeter Hospital, Exeter, United Kingdom
Abstract
Introduction: The Royal College of Surgeons of England (RCSE) published “Good Surgical Practice” in 2014. This publication includes a recommended minimum data set to be recorded in operation notes. We set out to quantify and improve adherence to these guidelines.
Methods: Operation notes (op. notes) were obtained for all patients undergoing Laparoscopic Cholecystectomies (lap. Chole.) between 1/11/2017 and 31/11/2017 and compliance to the guideline was assessed.
Findings were presented at a local meeting attended by surgical staff. Recommendations included: typing operation notes where possible, familiarization with the guidelines and display of the guideline in areas where operation notes are produced.
Finally the same data was collected from the op notes of all patients undergoing lap chole between 1/11/18 and 31/11/18. Compliance with the same set of guidance was assessed and comparisons made.
Results: Initially, 28 surgeries were carried out and the majority (24) of operation notes were hand written. Many criteria such as date, incision and operative findings were recorded in 100% of cases. Others, including time of surgery, DVT prophylaxis and name of anesthetist, were less consistently recorded.
At re-audit, 32 surgeries were performed. More operation notes were typed and legibility was improved. Compliance was improved in typed operation notes. In particular, time of surgery, elective/emergency status, and theatre anesthetist. In contrast, hand written operation notes demonstrated similar recording of the recommended data.
Conclusions: Adherence to this guidance was improved following intervention. Amount of typed op notes also increased. This may reflect use of typed, prepopulated operation notes.
P21 How to Improve the Experience of Day Surgery Patients
Tajinere Fregene1, Katherine Stagg1, Yun-Mei Lau1, Sarah Wintle2, Vishal Raman1, Holly Edmond1, Shaoib Rizvi1
1Royal Free Hospitals NHS Trust, London, United Kingdom. 2Royal Marsden Hospital, London, United Kingdom
Abstract
Introduction: This quality improvement project had two aims:
- Identify factors that influence the experience of elective surgery patients
- Improve that experience.
Methods: We conducted repeated snapshot surveys on our on-the-day surgical admissions unit over a four year period. On a given day, all patients admitted to the Royal Free Hospital for elective surgery to completed a questionnaire about their experience and the factors that influenced it.
We conducted semi-structured interviews with our patients about their experience and the themes were identified. The iterative nature of this project allowed us to identify which interventions were effective and which were less so.
Results: The proportion of patients reporting their overall experience as “Excellent” or “Good” was 65% in 2015, it peaked at 96% in 2017 and was 82% in 2019.
Patients who had operations before 12:00 were significantly more likely to report a “Good” or “Excellent” experience compared to those whose operations were after 15:00 (p<0.05).
The most common positive theme was the staff, who were described as friendly, helpful and caring. The most common negative factor theme was waiting before surgery.
Impactful interventions were staggering lists (reducing waiting times) and updating patients about their operation time. Ineffective interventions were; having a single telephone number for calls from theatre and the ward and altering the letters sent to patients.
Discussion: Our study demonstrates the importance of patient engagement in quality improvement projects. By speaking to our patients directly, we were able to make focused and effective changes to our processes.
Prize Papers
Prize 1 Major ambulatory surgery in a freestanding, bedless facility?
Brian Oosterhoff
DaisY, ehnv., Yverdon-les-Bains, Switzerland
Abstract
Introduction: In 2007, our local public hospital faced saturation and needed expansion while ambulatory surgery suffered from poor quality and bad cost-coverage. With this in mind, we reconsidered our organization and set up a dedicated, freestanding ambulatory surgery center (ASC).
We now perform more than 3800 increasingly invasive surgical procedures in a wide range of surgical specialties, without beds.
Methods: 9 years later we assessed the relevance of the freestanding option by using the SWOT tool and put some of our practical results in perspective with other studies, OECD data and recommendations.
Results: The freestanding, single level design facilitates setting up specific clinical pathways maximizing the quality and thereby improving cost-effectiveness.
The compact and open architectural design of the recovery room and the operating theater provides a safe and reassuring overview while preserving patient privacy.
The “bedless” concept helps optimizing patient circulation, increases the safety and turns out to be a real space saver.
The appropriate level of cooperation with the main hospital, an important key factor to success, has yet to be found and challenges us to find a different corporate structure.
Conclusions: Ambulatory surgery is about innovation of care, it’s not about improving hospitals. Architecture is an important key factor as it enables the blossoming of an adjusted culture to make it as simple and safe as possible.
The challenge of a successful integration of freestanding ASC’s in local healthcare systems might not to be underestimated.
Prize 2 Patient-centred hernia surgery in a Primary Care Setting: optimising quality
Michael Lewis, Rita Chotai, Anita Pandya
Norfolk and Norwich University Hospital, Norwich, United Kingdom
Abstract
Introduction: Stresses on the NHS and specifically secondary care has meant that some surgical services are increasingly difficult to provide in hospital environments. Long waits and difficult access requires strategies to change methods of provision that bring the patients needs into focus.
Method: We describe the provision of a day case local anaesthetic hernia service in a primary care setting instigated in 2015.
Results: The service was started in 2015. To August 2018 a total of 324 patients have undergone Consultant lead hernia surgery after 692 were seen in a dedicated hernia clinic. Surgery and clinics were done in an easily accessible primary care setting with a dedicated operating theatre and staff. The service required a standardised approach with Consultant Surgeon and Anaesthetist, a day 5 wound assessment, a standard post-operative analgesia protocol and pre and post patient information literature. There were two post operative admissions to secondary care (one at day 2 with pain, one at day 5 with a haematoma). One patient developed recurrence and two patients developed chronic groin pain.
National PROMs results showed an improvement of 54.4% by EQ5D and 57% by VAS (national results 51.3 and 39.2 respectively).
Patient satisfaction survey demonstrated a 92% excellent service response, 8% good service response and 92% would recommend the service to others.
Conclusion: Moving hernia surgery to primary care setting provides good results and excellent patient feedback. This model of Primary Care-based Consultant Lead Service may be the future way forward for hernia repair in the UK
Prize 3 Breaking the conventional -hip replacement as day surgery
Gyorgy Lovasz Lovasz, Marco La Malfa, Attila Aros
Barlborough NHS Treatment Centre, Barlborough, United Kingdom
Abstract
Background and aims: Longer life expectancy, obesity, changes in lifestyle have increased the prevalence of osteoarthritis therefore the demand for total hip arthroplasty in the forthcoming years is predicted to rise(over 90000 in 2017). It is well known that higher morbidity and mortality is associated with prolonged hospital stay after total joint arthroplasty. The current situation generates multiple problems for our healthcare system, principally an unsustainable high cost.
In order to reduce costs, ‘fast-track’ or ‘enhanced recovery’ protocols were introduced and found to be successful to reduce the length of stay compared with conventional pathways. While this led to a reduction in the LOS in our hospita from 4 to 1- 2.2 days, day-case arthroplasty is still relatively uncommon worldwide.
Our experience aims to define the safety and effectiveness of day-case arthroplasty
Methods: 25 patients scheduled for hip arthroplasty were included into the pilot study. Patients included were ASA 1 to ASA 2, BMI < 40, age was not an exclusion criteria. The anaesthetic protocol and fluid management were standardised.
Results: Of the 25 patients scheduled, 21 went home on the same day. Average length of surgery was 55minutes, average blood loss 277ml stay. Patients were discharged between 4 and 6 Pm. There were no readmissions. None of the patients used rescue analgesia at home
Conclusion: Outpatient hip arthroplasty is a good option for selected patients. Costs are reduced, safety (complications rate) and effectiveness (patient satisfaction and functionality)seem to not be compromised compared with conventional pathways for hip arthroplasty
Prize 4 Improving fluid fasting times and postoperative nausea rates after introducing a liberal preoperative fluid policy for patients undergoing elective surgery
Graham Harris1, Izzy Ross2, Michael Blundell1, Stephen Worthy1, Lindsay Dawson1
1Northumbria NHS Trust, Newcastle, United Kingdom. 2Newcastle University, Newcastle, United Kingdom
Abstract
Introduction: In 2018, Northumbria NHS Trust implemented a Liberal Preoperative Fluid Policy (LPFP) for patients undergoing elective surgery. Patients can now drink water freely until being transferred to theatres. Previously, drinking was prohibited in the two hours before general anaesthesia. However, previous audits had demonstrated that the Average Fluid Fast Time (AFFT) greatly exceeded the two-hour cut-off (5.7 Hours).
Fluid fasting is an unpleasant patient experience, linked to several adverse pre/postoperative consequences.
This re-audit aimed to review the current AFFT, since the introduction of the LPFP.
Methods: Questionnaires were distributed to the recovery units of four hospitals within the trust. Recovery nurses questioned all patients who had undergone elective surgery. The time of their last drink and arrival time to theatres was noted and used to deduce the AFFT. Nurses also recorded patients’ sensation of preoperative thirst and postoperative nausea & vomiting (PONV).
The re-audit ran between the 28th Jan – 8th Feb 2019.
Results: 219 questionnaires were completed, 188 included enough information to calculate the AFFT.
Our results demonstrated an AFFT of 2.1 Hours, an improvement of 63% compared to previous audit cycles.
75% reported drinking water in the three hours proceeding general anaesthesia.
Seven patients experienced PONV giving an incidence of 3.2%, previously recorded at 5.7%, a 43% decrease.
Pre-operative thirst reduced by 20%
Conclusion: A LPFP has resulted in a 63% decrease in the AFFT before elective surgery. Preoperative thirst rates have improved, with our results also suggesting that PONV has reduced since the implementation of the LPFP.
Prize 5 Upper limb day case arthroplasty – Developing a pathway
Mark McMullan, David Cloke
Northumbria NHS Foundation Trust , Newcastle upon Tyne, United Kingdom
Abstract
Introduction: There is a drive towards shortening length of stay for elective surgery. Whilst reducing hospital costs and bed pressures, it improves patient satisfaction and has proven possible in lower limb arthroplasty. A retrospective audit of upper limb arthroplasty (approx. 150 cases) showed a mean length of stay of 2.9 days.
Our aim was to develop and introduce a pathway for upper limb arthroplasty day-cases in our trust.
Methods: A clearly defined pathway was devised in collaboration with a multidisciplinary team. This involved identifying suitable patients and educating them in the process. Anaesthetic, physiotherapy and occupational therapy evaluation were carried out to identify obstacles to discharge. Patients were placed first on morning lists and planned for regional analgesia, with a general anaesthetic or sedation. Ward contact details were given on discharge along with pain diaries and rescue analgesia.
Results: Of 21 suitable cases since introduction of the pathway, 16 successful day-cases have been managed across two sites within the trust. Failed discharges were on one of the two sites. Patient feedback is positive and we have had no readmissions or complications relating to early discharge. The success of our pathway on mainly one site suggests logistical issues and lack of engagement in the pathway may be a factor.
Conclusion: Day-case arthroplasty may be beneficial and is possible, but patient selection and education of all team members is key. We hope the formation of a clear pathway and multidisciplinary collaboration has potential to establish this as standard practice in the trust.
Prize 6 Total Ankle Replacement – Walking the Path to Day Case Surgery
Benjamin Drake, Michael Blundell, Bruce Gibson, Rajesh Kakwani, David Townshend
Northumbria Healthcare NHS Foundation Trust, North Tyneside, United Kingdom
Abstract
Introduction: Day Case Surgery is a priority within the National Health Service and has been shown to provide beneficial outcomes for patients and hospitals. We report our experience developing a Day Case Programme for Total Ankle Replacement (TAR).
Methods: Prior to the introduction of a Day Case Programme, average length of stay following TAR in our unit was 3.5 days. Stakeholders were consulted about ways in which same day discharge could be facilitated. Patients’ post-operative pain charts were reviewed prior to the introduction of this programme. Inclusion criteria included non-complex surgery, friend or relative support and pre-operative walking-aid assessment. An enhanced recovery protocol included long-acting popliteal block and dexamethasone. Patients were discharged with opiate analgesia and written pain instructions. Patients were asked to complete a pain and satisfaction questionnaire. Patient Reported Outcome Measures (PROMs) were recorded.
Results: From September 2017 to April 2019 21 of 70 patients underwent TAR as a Day Case. Mean age was 67 years (43–85 years). Complications included one superficial infection and one readmission on day three with urinary retention. No patients reported post-operative nausea or vomiting, half did not use Oramorph at home. Average Visual Analogue Score for pain was 21 on day one and day three post-operatively. PROMs at 12 months showed a trend improvement compared to standard inpatient care.
Conclusions: Early results suggest that Day Case Total Ankle Replacements are safe. Appropriate patient selection is necessary. Day Case Surgery relies on support and communication between multiple teams to organise and run effectively.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29257/asm-abs-2019.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse6
Shazia M Khan, Specialist Registrar in Surgery,1 Mahmoud Bakr, Medical Student, 1,2 Iman A Azmy, Consultant Oncoplastic Breast Surgeon, 1 Ciaran J Hollywood, Consultant Oncoplastic Breast Surgeon, 1 Amar Jawad, Consultant Anaesthetist, 1 Julia C Massey, Consultant Oncoplastic Breast Surgeon1
1 Chesterfield Royal Hospital NHS Foundation Trust . 2 The Medical School, University of Sheffield
Corresponding author: Shazia M Khan
Keywords: Day case, mastectomy, service improvement, audit loop
Declaration
There was no funding required for this project.
The authors have no affiliations that could be perceived as posing a potential conflict of interest in the publication of this article.
Abstract
Introduction: The 2016 BADS target for day case mastectomies was 30% (1). At Chesterfield Royal Hospital we achieved 25% (2). To improve this we conducted an audit to document our day case mastectomy rates, determine causes for inpatient stay and identify modifiable factors.
Method: All mastectomies performed in our unit over a 4 month period were included. Factors influencing admission were: carer presence post-operatively, distance from hospital, co-morbidities, type of surgery, surgical drain use, regional block, opioid use. Recommendations regarding modifiable factors were used to implement change. The audit was repeated one year later.
Results: In 2016, 10 out of 26 patients were planned day cases. 2 became unplanned admissions; making our actual day case mastectomy rate 31% (8/26). Modifiable factors influencing planned inpatient rates were identified: inaccurate allocation of patients’ hospital episode to the “planned admissions” group leading to coding errors (3/16), reason for inpatient planning not clearly documented (8/16), ANC (4/16) and bilateral mastectomy (2/16), use of drains in ANC (4/16). In 2017, 10 out of 19 patients were planned day cases. One became an unplanned admission; making our 2017 day case mastectomy rate 47%
Conclusions: The initial audit highlighted the need for: more robust documentation of reasons for inpatient admission planning, recognising that ANC and bilateral mastectomies alone shouldn’t necessitate admission, reviewing our use of drains in ANC & further promotion of our existing outpatient drain removal pathway in the minority that receive a drain. On re-auditing we saw an improved day case mastectomy rate from 31% to 47% following the implementation of the recommendations of the initial audit.
Introduction
Breast cancer is the commonest cancer in women in England & Wales with an annual incidence of 55,222 (3). 74% of breast cancer patients receive a surgical resection as part of their cancer treatment (4) and the majority of these patients undergo surgery as their first procedure.
Historically, patients undergoing breast cancer surgery required up to 6 days’ inpatient stay. Recognising the need for efficiency savings to be made in an era of diminishing available resources to serve the increasing demands placed on the National Health Service, the Department of Health in 2002 launched its “Day Surgery Strategy” with an aim of achieving 75% of all elective surgery in the UK to be performed on a day case basis by the year 2005. (5) Over the past 2 decades advancements in surgical and anaesthetic techniques have continued to improve and facilitate the national drive towards day case breast surgery. (6) An expansion of the age, ASA, and BMI eligibility criteria for day surgery procedures recommended in the in 2011 British Association of Day Surgery guidelines (7), in recognition of the national trends towards an aging population and rising levels of obesity, has enabled an even greater proportion of our patients to be considered as potential day case candidates.
Mastectomies are ideal procedures for day case surgery due to their significantly lower rates of post-operative events including pain, nausea & vomiting, venous thromboembolism and the greater feasibility of early mobilisation. (8,9) Patients report greater convenience in their own home environment with better recovery (9), while providers benefit from reduced hospital bed occupancy rates, reduced length of hospital stay (10) and hence reduced rates of hospital acquired infections; making this a financially sound option too.
In 2012 the “Quality & Productivity Case Study” published by NHS Improvement reported a 50% reduction in length of stay, release of 61,000 bed-day capacity and potential saving of £10.5 million if day case breast cancer surgery was rolled out nationally. (10) At Chesterfield Royal Hospital we estimated a potential saving of £5686 over the period April to July 2016 by moving from our recorded current practice to all day case mastectomies.
The day case procedure Best Practice Tariff (BPT) is a financial incentive for providers which aims to increase the proportion of elective activity performed as a day case, where clinically appropriate. The British Association of Day Surgery publishes a directory of procedures suitable for day-case admissions along with rates that they believe are achievable in most cases. Selection of procedures for day case BPT is based on the BADS directory. These are high volume procedures and have day case rates that vary significantly between providers and with achievement nationally that is below the BADS rates. In 2016 the BADS target for day case mastectomy was 30% (1). At Chesterfield Royal Hospital our published day case rate was only 25% (2). To identify ways in which we could improve our service, we conducted an initial audit to address this. The aims were to:
- document our day case and inpatient mastectomy rates
- determine causes for inpatient stay
- identify any modifiable factors to improve day case rate
- identify any coding errors impacting on our published day case rate
- identify achievable changes to our service that we can implement and re-audit
Methods
We conducted a retrospective initial audit of our service over a 4 month period in 2016, comparing this to nationally recommended day case rates for breast surgery. All patients having mastectomies with or without any form of axillary surgery and without immediate breast reconstructions between April and July 2016 were included. Patients were identified from the Service Improvement Lead & checked against consultants’ theatre diaries. Patients were excluded if their case notes were not available. A list of potential modifiable factors that would influence our day case activity was complied. Pre-operative factors in this list included co-morbidities, type of breast & axillary surgery (unilateral versus bilateral mastectomy and sentinel node biopsy versus axillary node clearance), distance from hospital, and availability of responsible adult at home for the first 24 hours post-operatively. Peri-operative factors included use of regional anaesthetic blocks, opioid analgesia & antiemetic use peri-operatively and use of surgical drains.
The audit was repeated for the same time period in 2017 following implementation of changes recommend by the 2016 audit.
Results
27 patients had mastectomies during the initial study period in 2016. 1 patient was excluded as her case notes were unavailable. Of the 26 cases studied, 10 were planned as day case. See figure 1.
Figure 1. Number of patients planned as inpatient and day case over four months in 2016.
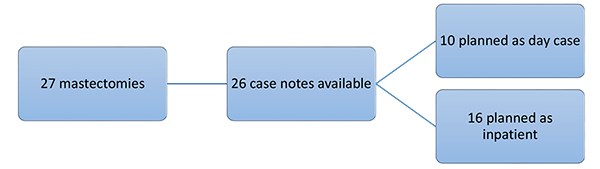
3 patients had been incorrectly coded as having planned inpatient stay post-operatively when in fact they had day surgery procedures. This increased our number planned as day case to 10. However, 2 out of these 10 patients ultimately required unplanned admission. One was due to PONV despite the patient having a regional block and anti-emetics with morphine. The other unplanned admission was due to low oxygen saturations post operatively in an asthmatic patient.
Thus we achieved a final day case rate for this period of 31% (8/26) once coding inaccuracies were removed, figure 2.
Figure 2. Mastectomies in the 4 Month Period 2016.
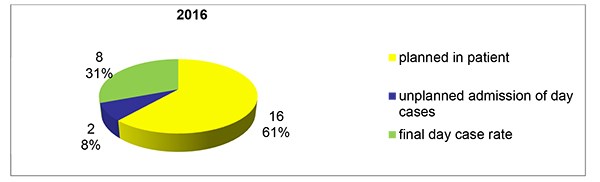
On re-auditing our practice over the April to July 4 month period in 2017 we found 21 patients had mastectomies. Two patients were excluded from further review as they had immediate breast reconstruction at the time of mastectomy. 10 of the remaining 19 patients were planned as day case (Figure 3)
Figure 3. Number of patients planned as inpatient and day case over four months in 2017.
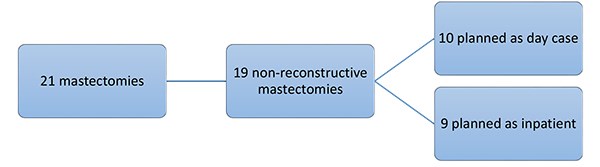
One of these 10 required an unplanned admission to hospital postoperatively due to having a persistently low respiration rate (<10 /min) post operatively. This patient was administered opiate analgesia intraoperatively. She was allowed home the following day when the opiate effect had worn off. Our final day case mastectomy rate was 47% (9/19) in the 2017 study period, Figure 4.
Figure 4. Mastectomies in the 4 Month Period 2017.
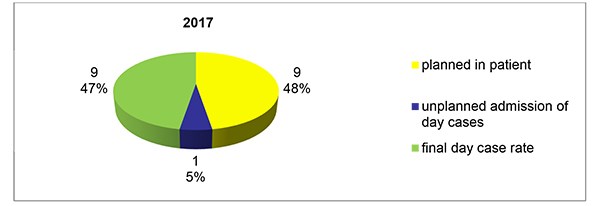
In 2016, 16 patients had a planned inpatient stay and reasons given for this are shown in Figure 5. The reason for inpatient stay was not clearly documented for 8 out of the 16 patients. On closer review, 4 of these patients had axillary node clearances with one patient having a surgical drain placed. 2 of the 8 had bilateral mastectomies. It was inferred that the types of surgery might have influenced the decision for inpatient stay; however, we routinely perform axillary node clearance as day case surgery. For the remaining 2 patients no potential reason for inpatient stay was identifiable.
Figure 5. Reasons Given for Planned Inpatient Stay 2016.
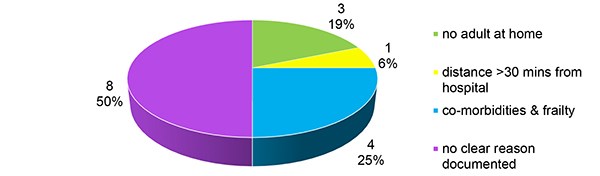
In the re-audit period we found 9 patients needed planned inpatient stay, the reasons for this are illustrated in Figure 6. An improvement in documentation of reasons for inpatient planning was noted by 2017, with 33% (3/9) of patients having no clear reason documented in 2017 compared to 50% (8/16) for 2016. Where no clear reason was identifiable in the 3 out of 9 patients in 2107; 2 had bilateral mastectomies and one had no potential reason identifiable for inpatient stay.
Figure 6. Reasons Given for Planned Inpatient Stay 2017.
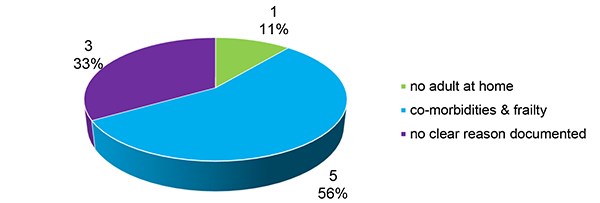
Table 1 details the reasons for planned inpatient stay for the patients who required admission due to co-morbidity & frailty.
Table 1. Co-morbidities necessitating planned admission.
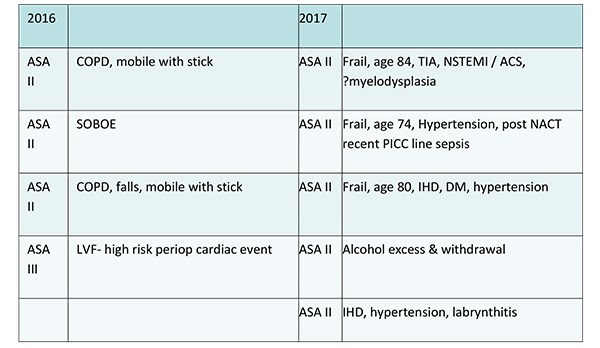
Discussion
Historically there was a reluctance for early discharge home due to perceived gravity of cancer surgery and the need for specialist care post operatively. The clinician’s decision on whether to offer day case mastectomy to a patient in the modern era may be influenced by the availability of comprehensive oncoplastic services, patient motivation and the availability of robust out of hours’ services. To this end, a cornerstone to the success of modern day case breast surgery is the role of the specialist BCN in their peri-operative interactions with patients & carers to address their concerns and expectations regarding recovery at home, especially with drains in situ. (11) Recent studies with large patient cohorts have once again added to the wealth of available evidence confirming that whilst day case breast surgery has been shown to be safe, its success relies upon maximising close collaboration by all stakeholders including a well organised multi-professional team; at the same time as ensuring patients are reassured through education that the quality of their post-operative care will not be compromised by what they may have previously perceived as too early a discharge home. (12)
We have demonstrated here that in 2016 when coding errors are removed, over the period studied, Chesterfield Royal Hospital just achieved the target set by BADS for day case mastectomy.
When searching for ways to improve our day case mastectomy rate further we recognise some factors would be more readily modifiable than others.
It is difficult to improve on the unexpected events encountered leading to unplanned admission, despite perioperative optimisation as seen in the 2 out of 10 patients admitted in the 2016 group due to PONV despite use of regional block and anti-emetics, or low saturations in an asthmatic patient. In the 2017 group, only one patient had unplanned admission and this was due to persistently low respiration rate due to opiate effect. Our unit’s routine anaesthetic practice is to avoid perioperative opiate use and to administer a pectoral nerve block, where possible to avoid problems associated with opiate use. Without major input of increasingly fewer resources it is also difficult to improve the day case mastectomy rate in the case of the 8 patients out of 16 in 2016 who had either no carer, or lived a long distance from the hospital or had multiple significant co-morbidities.
However, an obvious area for improvement is in the 8 out of 16 patients’ group in the initial audit who had no clear documentation of indication for planned inpatient admission. Of these 4 had ANC (one of whom had a surgical drain inserted), 2 had bilateral mastectomies and for 2 patients it was inferred from the notes that the reason for planned admission was patient choice, though this was not clearly documented. Clear documentation of reasons for planned inpatient stay would also facilitate and improve consistency of admission planning across our unit.
Although there is no consensus on pre-assessment criteria, a patient’s choice, medical fitness, social support and requirement for immediate breast reconstruction are among the key factors for consideration when planning inpatient stay. (11,13) Whilst patient choice and non-availability of an adult carer post operatively are valid reasons for planned inpatient stay; in the modern perioperative care setting neither ANC (14) nor bilateral mastectomy alone mandate inpatient stay (13). In the United States the Healthcare Cost and Utilization Project (HCUP) data showed that between 2005 and 2013 the rate of bilateral mastectomies tripled. By 2013 whilst unilateral mastectomies were still commoner approximately one third of bilateral and half of unilateral mastectomies were performed in the outpatient setting. (15)
Although many units, ours included, have now dispensed with the routine placement of a surgical drain in cases of mastectomy alone without reconstruction; use of drains in ANC is variable. Mastectomy and ANC surgeries have been shown to have up to 91% seroma rate when no drain is used versus 85% with a drain. (16) Other studies have shown that whilst there may be some reduction in seroma rates with the use of axillary drainage (17), infection rates (17) and the overall duration of seroma fluid accumulation remains unaltered (18). Axillary drain placement is associated with a longer hospital stay. (17,19) Outpatient drain removal services are useful in preventing inpatient stay purely for drain management in instances where one is used. Discharge with drain in situ has long been shown to be a safe and cost effective strategy with high rates of patient satisfaction reported when supported by well-co-ordinated inpatient and outpatient services. (20,21,22) We note that utilisation of our unit’s outpatient drain removal pathway needs to be improved and flow through this is likely to be increased with further staff education and engagement. (23) Clinical pathways have been shown to be good educational tools; particularly for new staff, nurses and allied health professionals. (24,25) Revisiting our own local outpatient drain removal pathway at points of staff changeover and induction may maximise its effective implementation.
Better utilisation of our outpatient drain removal pathway may also improve overall patient flow through the hospital. Unit based pathways have been shown to not only impacts on the micro system of service provision in a single unit and its day case rates, for example, but also to affect, indirectly, the macro system of the hospital as a whole; not least by streamlining bed occupancy rates to ensure bed availability for those patients where admission is necessary. (26)
Our main focus in this study was to look at ways of improving our day case mastectomy rate by identifying modifiable factors in the pre-operative planning phase. We did not set out to review readmission rates as part of this study. Although very valuable to establishing the success of a day case mastectomy service; this separate line of enquiry may be considered the subject of a subsequent study. We recognise that this study represents a very small cohort of patients and the results of the achieved day case rates comparing 2016 & 2017 lack statistical significance (χ2 analysis p value > 0.05). However, it highlights key areas for improvement in the service we provide to our patients. We need robust documentation of and consistency in admission planning for different types of surgery as ANC and bilateral mastectomies alone do not necessitate inpatient stay. Studies have shown that patient flow can be optimised by addressing organisational boundaries at various points along the patients’ care journey. (26) Therefore, whilst we looked at ways of maximising ward staff awareness of our outpatient drain removal pathway, we also reviewed our use of drains in ANC. The outpatient drain removal pathway was then used in the minority that require a drain post ANC.
We liaised with the clinical coding department to minimise future costly coding inaccuracies. We re-audited our practice and by placing patient safety and satisfaction as well as staff education at the core of team practice, following implementation of the changes recommended by the initial audit we were able to improve our performance.
The findings of our initial audit were disseminated locally and presented at the BADS annual meeting 2017. Change was implement based on the recommendations regarding the identified modifiable variables. The audit was repeated one year later to assess the effect of these implementations.
In completing the audit loop in 2017 over the same 4 month period, we demonstrated a marked improvement in the day case mastectomy rate at Chesterfield Royal Hospital from 31% to 47%. As a team indoctrinating the philosophy that day surgery is the default position for non-reconstructive mastectomy with or without axillary surgery into our practice and promoting this to our patients our documentation of the reasons for planning inpatient stay has also improved from 50% to 66%. In the patients without any clearly discernible reason for inpatient planning in both the audits a possible explanation may have been simply patient choice, though this needs documenting.
We plan to continue to seek out further areas of development in an effort to increase our day case mastectomy rate further.
References
- British Association of Day Surgery. (2016). BADS Directory of Procedures. 5th Edition. BADS, London.
- Productivity.nhs.uk. (2017). Better Care, Better Values. [online] Available at: http://productivity.nhs.uk/PCT_Dashboard/DetailedView? practiceCode=RFS&pctCode=Q55&percentileId=2 &yearQtrId=29&indicatorId=609&indicatorTypeId=1&component Name=Simple%20mastectomy%20(with%20and%20w ithout%20axillary%20surgery)&treatment=selected&componentId=3004#performance [Accessed 31/03/2017
- Cancer Research UK (2017]), Breast Cancer Statistics, Cancer Research UK. [On line] Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer [accessed 31/ March 2017
- National Cancer Intelligence Network and Cancer Research UK. Major resections by cancer site, in England; 2006 to 2010 workbook (Version 2.0 - reissued June 2015) (link is external). London: NCIN; 2015.
- Department of Health: In Day Surgery: Operational Guide. 2002, Department of Health, London.
- Kopp, S. L. and Horlocker, T. T. (2010), Regional anaesthesia in day-stay and short-stay surgery. Anaesthesia, 65: 84–96. doi:10.1111/j.1365-2044.2009.06204.x
- Verma R, Alladi R, Jackson I, Johnston I, Kumar C, Page R, Smith I, Stocker M, Tickner C, Williams S and Young R: Day Surgery and short stay Surgery: 2. Anaesthesia. 66,2011, 417-434
- Jeevan R, Cromwell D, Browne J, et al. National Mastectomy and Breast Reconstruction Audit 2010. Third Annual Report, vol. IC28050110, 2010.
- Canet J, Raeder J, Rasmussen LS, Enlund M, Kuipers HM, Hanning CD, Jolles J, Korttila K, Siersma VD, Dodds C, Abildstrom H, Sneyd JR, Vila P, Johnson T, Muñoz Corsini L, Silverstein JH, Nielsen IK, Moller JT; ISPOCD2 investigators. Cognitive dysfunction after minor surgery in the elderly. Acta Anaesthesiologica Scandinavica. 2003 Nov; 47(10):1204-10
- National Institute for Health and Clinical Excellence (2012). Ambulatory breast cancer surgical care: day case and one night stay. In: NHS Evidence: Quality and Productivity Study. Available at: http://publications.nice.org.uk/pmg6. [Accessed 31/03/2017]
- Marla S, Stallard S. Systematic review of day surgery for breast cancer..Int J Surg. 2009 Aug;7(4):318-23. doi: 10.1016/j.ijsu.2009.04.015. Epub 2009 May 8
- Ballardini B, Cavalli M, Manfredi GF, Sangalli C, Galimberti V, Intra M, Rossi EM, Seco J, Campanelli G, Veronesi P. Surgical treatment of breast lesions at a Day Centre: Experience of the European Institute of Oncology.Breast. 2016 Jun;27:169-74. doi: 10.1016/j.breast.2016.04.002. Epub 2016 Apr 25. P7.
- Yvonne Ying Ru Ng, Patrick Mun Yew Chan, Juliana Jia Chuan Chen, Melanie Dee Wern Seah, Christine Teo, and Ern Yu Tan. Adopting Ambulatory Breast Cancer Surgery as the Standard of Care in an Asian Population. International Journal of Breast Cancer, vol. 2014, Article ID 672743, 8 pages, 2014. doi:10.1155/2014/672743
- Athey N, Gilliam AD, Sinha P, Kurup VJ, Hennessey C, Leaper DJ. Day-case breast cancer axillary surgery. Ann R Coll Surg Engl. 2005 Mar;87(2):96-8.
- Steiner CA, Weiss AJ, Barrett ML, Fingar KR, Davis PH. Trends in Bilateral and Unilateral Mastectomies in Hospital Inpatient and Ambulatory Settings, 2005-2013. HCUP Statistical Brief #201. February 2016. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb201-Mastectomies-Inpatient-Outpatient.pdf.
- Troost MS, Kempees CJ, de Roos MA. Breast cancer surgery without drains: no influence on seroma formation. Int J Surg. 2015 Jan;13:170-4. doi: 10.1016/j.ijsu.2014.11.050. Epub 2014 Dec 6..
- Thomson DR, Sadideen H, Furniss D. Wound drainage after axillary dissection for carcinoma of the breast. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No.: CD006823. DOI: 10.1002/14651858.CD006823.pub2.
- Talbot ML, Magarey CJ. Reduced use of drains following axillary lymphadenectomy for breast cancer. ANZ Journal of Surgery 2002;72(7):488-90. [PUBMED: 12123509]
- He XD, Guo ZH, Tian JH, Yang KH, Xie XD. Whether drainage should be used after surgery for breast cancer? A systematic review of randomized controlled trials. Med Oncol. 2011 Dec;28 Suppl 1:S22-30. doi: 10.1007/s12032-010-9673-2. Epub 2010 Sep 9.
- Holcombe C, West N, Mansel RE, Horgan K. The satisfaction and savings of early discharge with drain in situ following axillary lymphadenectomy in the treatment of breast cancer. Eur J Surg Oncol. 1995;21:604–606.
- Burke CC, Zabka CL, McCarver KJ, Singletary SE. Patient satisfaction with 23-hour "short-stay" observation following breast cancer surgery. Oncol Nurs Forum. 1997;24:645–651.
- Chadha NK, Cumming S, O'Connor R, Burke M. . Is discharge home with drains after breast surgery producing satisfactory outcomes? Ann R Coll Surg Engl. 2004 Sep;86(5):353-7
- Allen D, Gillen E. Systematic review of the effectiveness of integrated care pathways: what works, for whom, in which circumstances? Int j evid based healthc. 2009 jun;7(2):61-74. doi: 10.1111/j.1744-1609.2009.00127. x.
- Bryson A and Browning J (1999) Clinical audit and quality using integrated pathways of care. Report No.: CA96/01, Edinburgh: CRAG, Clinical Resource and Audit
- Roberts P1, Boldy D, Robertson J. . Use and development of clinical pathways by registered nurses in an acute paediatric setting. Collegian. 2005 Oct;12(4):22-8
- The Health Foundation – Inspiring Improvement (2013). Improving Patient Flow - How two trusts focused on flow to improve the quality of care and use available capacity effectively. [online] Available at: http://www.health.org.uk/sites/health/files/ImprovingPatientFlow_fullversion.pdf. [Accessed 13/11/2017]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29260/khan.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse7
Matthew Allan Jonesa, Dan Morellb, Chrishan Mariathasc, Meg Birksd
aConsultant Hand and Wrist Surgeon, University Hospital Coventry
bConsultant Hand and Wrist Surgeon, Doncaster and Bassetlaw Teaching Hospitals
cHand Fellow
dConsultant Hand and Wrist Surgeon, Sheffield Hand Centre
Sheffield Hand Centre, Northern General Hospital, Herries Road, Sheffield S5 7AU
Corresponding author: Matthew Allan Jones, Consultant Hand and Wrist Surgeon, Orthopaedic Offices, Level 5, University Hospital Coventry, Clifford Bridge Road, Coventry CV2 2DX . Email: Matthew.jones2@uhcw.nhs.uk
Key words: Unplanned admission; unanticipated admission; day surgery; hand surgery
Acknowledgements
The authors wish to acknowledge and thank Georgina Jones, Professor of Health Psychology at the School of Social Sciences at Leeds Beckett University for her assistance with statistical analysis.
Conflicts of interest statement
No funding was received and there are no conflicts of interest.
Abstract
Introduction: The UK Department of Health recommends that 75% of elective surgery should be undertaken as a daycase with an unplanned admission rate below 3%. Most hand surgery is undertaken with the intention of discharge on the day of admission. We sought to establish our unplanned admission and readmission rates, and implement changes in practice to improve these.
Methods: A hospital database review identified the number of patients treated at the hand centre with a length of stay of more than 0 days, or readmission within 48 hours. The patient records were analysed for factors which may indicate the need for an overnight stay. Reasons for admission were recorded. Changes were made to post-operative analgesia and patient information leaflets. Regional block techniques were refined and more widely used. The process was then repeated to establish the efficacy of the changes.
Results: From April 2012 to March 2014, 4407 patients were admitted to the hand centre. Sixty-six had an unplanned overnight stay or readmission (1.50%). Common reasons were pain and post-operative nausea and vomiting. After the changes were implemented, a repeat review from April 2016 to June 2016 identified 886 admissions with only 3 having an unplanned overnight stay (0.34%).
Conclusions: Attention to timing of surgery, anaesthetic techniques, post-operative analgesia, patient information and social arrangements can minimise unplanned admission rates in daycase hand surgery at minimal cost.
Introduction
Guidance introduced by the UK Department of Health recommends that 75% of elective surgery should be undertaken as a daycase with an unplanned admission rate below 3% (1). Unplanned admissions and readmissions after daycase surgery are undesirable from both the patients’ and the healthcare provider’s perspective for financial, operational and quality reasons. Daycase surgery is preferred by the majority of patients due to convenience, reduced requirement for social arrangements, and a reduction in the likelihood of acquiring a nosocomial infection (2-4). Avoiding an overnight stay results in a significant saving for healthcare commissioning groups.
The aim of this study was to assess the rate of unplanned admissions and readmissions after daycase hand surgery at a tertiary referral adult hand centre. The centre is based in a UK teaching hospital serving a local population of 500,000 and an extended catchment of 3 million, where the majority of elective and trauma work is carried out on an ambulatory, same day discharge basis. Improvements to the service to reduce these rates were sought.
Methods
The first phase of the study was to carry out a retrospective review of performance. All patients admitted under the care of hand surgery consultants over a two year period (1st April 2012 to 31st March 2014) were identified from the hospital databases. Those with a length of stay (LOS) greater than zero days were identified and each case investigated. ‘Daycase’ was defined as admission and discharge on the same day (i.e. no overnight stay). Patients with planned overnight stay as per their operation note and incorrectly recorded cases of overnight stay were excluded.
Routine admission was anticipated for patients undergoing total wrist arthroplasty, brachial plexus surgery or those requiring inpatient neuro-rehabilitation post-operatively. Trauma patients requiring intravenous antibiotics, observation of neurovascular status and monitoring for the development of compartment syndrome were also considered planned admissions and therefore excluded. Those who had been discharged on the day of surgery but then readmitted within 48 hours were also identified and included.
Electronic and paper case notes were scrutinised for demographics and details surrounding the care episode (figure 1). Data were analysed with the assistance of a statistician and Chi-squared tests were carried out using SPSS.
Figure 1 – Information collected about unplanned admissions.
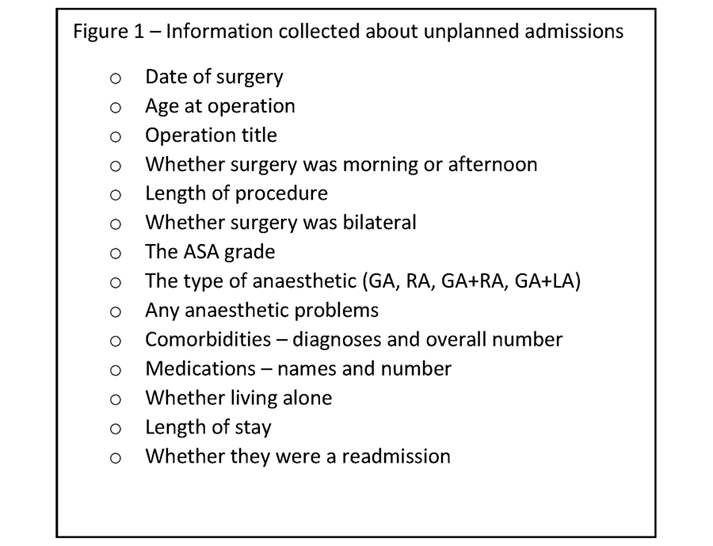
The first phase identified post-operative pain as the main reason for unplanned admission. The following strategies were formulated in collaboration with colleagues in anaesthetics to mitigate this problem:
- Addition of ibuprofen to the take-home analgesic medications for 48 hours post-operatively for all patients, including those having bony surgery, unless contraindicated.
- Introduction of a post-operative analgesia patient information leaflet to augment the verbal information provided at discharge (figure 2)
- Refinement of the regional anaesthetic techniques for hand and wrist surgery using a short-acting brachial plexus block and long-acting peripheral nerve block to enhance post-operative analgesia without an associated flail limb
- The anaesthetic team expanded the number of clinicians trained in the administration of regional anaesthesia, including a number of Physicians’ Assistants, ensuring almost all hand surgery lists are staffed by someone competent in ultrasound-guided regional anaesthesia.
The second phase of data collection was then carried out in the same way as the first, for a three month period, after the interventions to assess their effect.
Figure 2 – Post Operative Pain Relief Patient Information Leaflet.
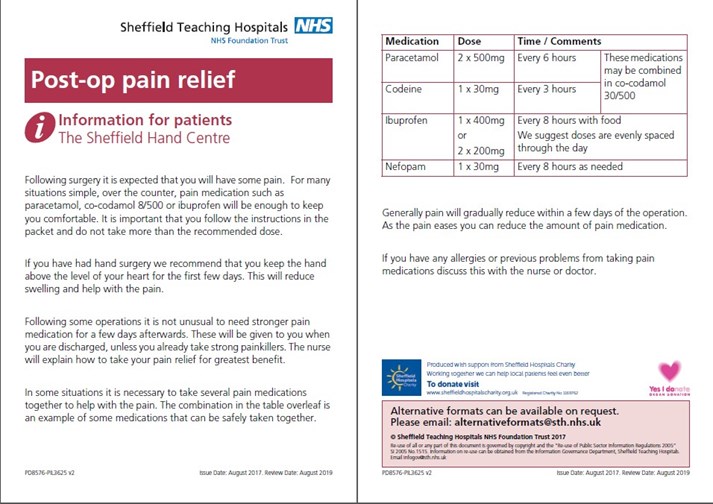
Results
First phase
During the first study phase (April 2012 to March 2014) 4,407 patients were admitted via the hand centre. A flow chart detailing the fate of those individuals can be seen in figure 3; 62 were unplanned admissions on the day of surgery. In addition there were four readmissions in the first 48 hours after surgery. The total number of unplanned admission at this time was 66 making the rate of unplanned admissions 1.5%. Thirty-two were male and 34 female.
Figure 3 – Flow chart of Patient Cohort Phase 1 (April 2012 – March 2014).

Other features of the group are shown in Table 1. Of these 66 patients, 17 lived alone, 30 lived with someone and for 19 their home circumstances were not recorded. The reasons for admission are shown in Table 2.
Table 1 – Patient Demographics and General Information.
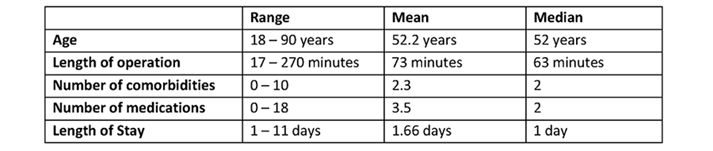
Table 2 – Reason for Overnight Admission.
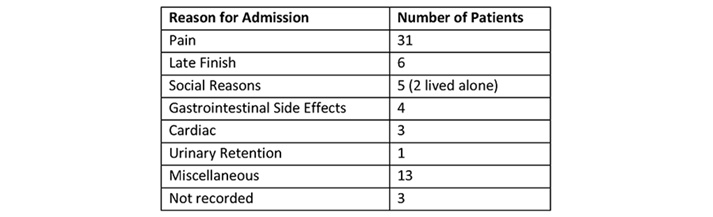
Time of surgery is shown in table 3. Operations carried out in the afternoon were markedly more likely to result in an unplanned admission. However, the day of the week was not linked to likelihood of admission (table 4).
Table 3 – Time of Day Surgery Performed.
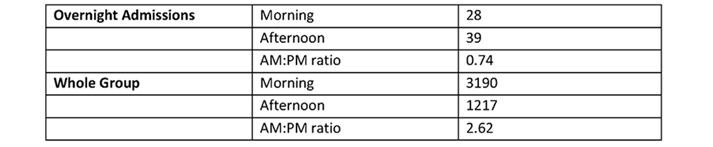
Table 4 – Day of the Week Surgery Performed.
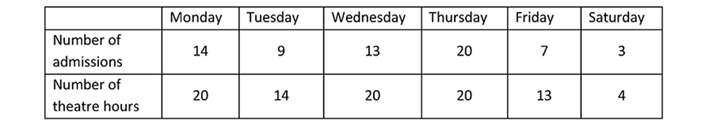
The type of surgery had a clear influence on unplanned overnight admission. The total number of unplanned admissions per operation, or type of operation, is presented in Table 5 along with the total number of those procedures carried out by the Hand Service during that period. Statistical analysis reveals that Ulna Shortening, Brunelli Ligament Reconstruction, Corrective Osteotomy (all) and Open Reduction Internal Fixation (ORIF) (all) each had a significantly higher chance of being admitted (p value <0.01). Soft Tissue Procedures have a significantly lower risk of unplanned admission, p <0.01.
Table 5 – Rate of Admission by Type of Surgical Procedure.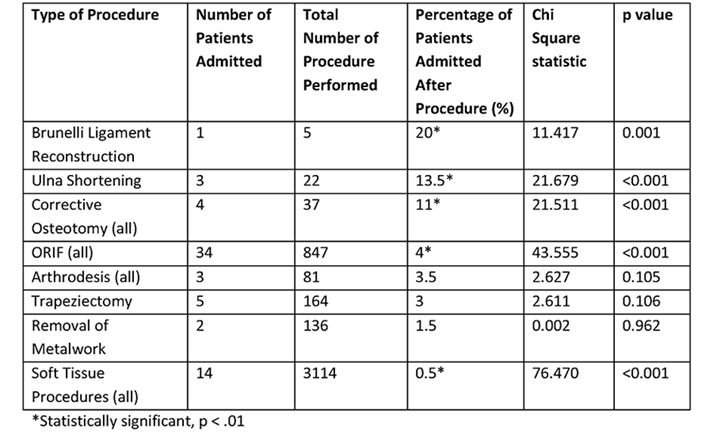
Assessment of whether anaesthetic factors contributed to unplanned admission was hampered by inability to obtain detailed anaesthetic information for the group successfully treated as day patients. The modal ASA grade in the unplanned admission group was 2 (range 1-4).
The type of anaesthetic received by these patients is shown in Table 6. In the unplanned admission group, GA represented all or part of the technique for 61% of patients. Data regarding combined anaesthesia (GA with RA or local anaesthesia) is not recorded in a format that can be easily retrieved and assessment of large numbers of successful day case hand surgery patients was not feasible. During the initial study period 20% of all hand surgery patients received a general anaesthetic (GA).
Table 6 – Type of Anaesthetic.
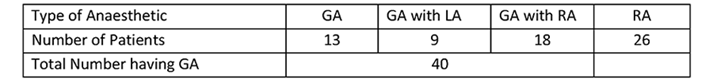
Second phase
To evaluate the changes in practice, the second phase was carried out from April to June 2016. During this period 886 patients were admitted to the hand centre for hand surgery (figure 4). This number is similar to the number admitted in April-June 2012 and April-June 2013 (during the first phase), accepting a gradual increase in the activity of the unit over time. Of these, 31 were coded as having a length of stay greater than zero days. There were only four coding errors in this sample. The rate of coding errors reduced from 3.6% in 2012-14 to 0.45% in 2016.
Figure 4 – Flow chart of Patient Cohort Phase 2 (April 2016 – June 2016).
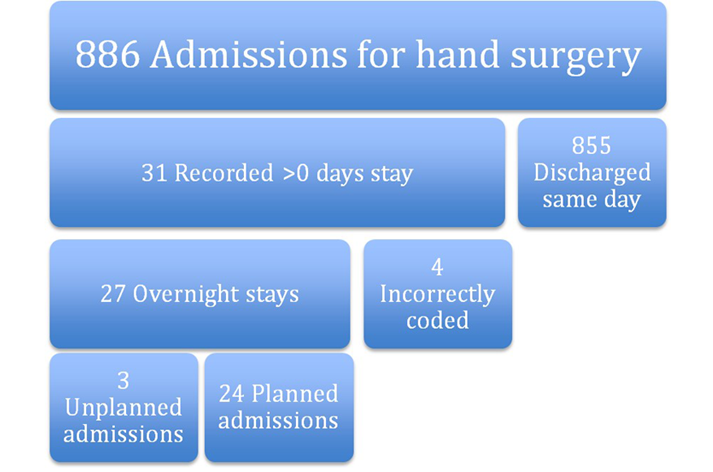
There were 24 planned admissions; the majority were for post operative intravenous (IV) antibiotics. The rate of planned admissions remained static. There were three unplanned admissions, a rate of 0.34%. Table 7 shows a comparison of the two study periods. The reduction in unplanned admissions is significant at p < 0.05. Of note there was a reduction from approximately one in two to one in three unplanned admissions resulting from pain.
Table 7 – Comparison of 2012-14 and 2016 Study Periods.
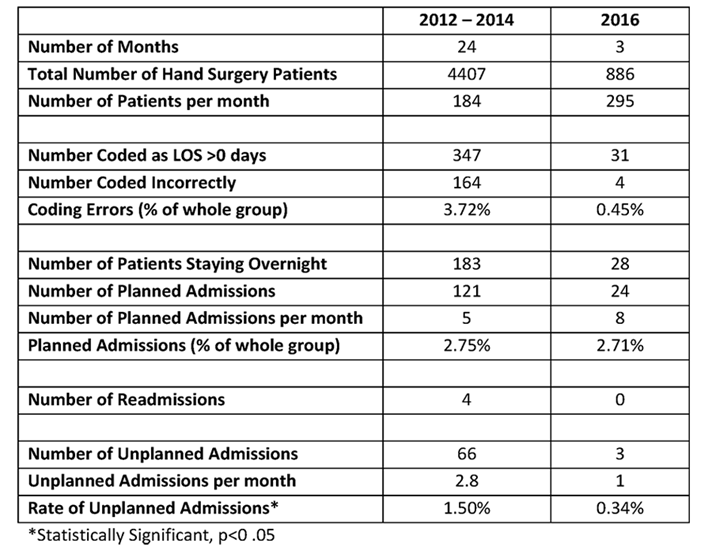
Discussion
Phase one of the study identified that almost half of unplanned admissions were attributed to inadequate pain control. This is in keeping with other studies which also cite bleeding and post-operative nausea and vomiting (PONV) as common reasons (5-13). The changes implemented regarding anaesthetic techniques and post-op analgesia contributed to the improved rate of successful daycase surgery.
Procedures on bone were more likely to result in unplanned admission. In a hand surgery cohort, Goodman et al found more invasive surgeries had higher complication rates (9). Other studies have found that the type of surgery undertaken, and the specialty delivering the care, have a profound effect. General surgery, urology and gynaecology are associated with higher rates of admission (6, 10, 14). Rates of unplanned admission can be as high as 30% (11) for procedures such as laparoscopic cholecystectomy, whereas for orthopaedic day cases, rates tend to be much lower. Cardosa et al published a 1.07% admission rate in daycase knee arthrosopy patients at an orthopaedic centre (15). Minatti et al found a post-discharge admission rate of 1% within 30 days, halving to 0.49% when only including the orthopaedic cohort (14). Our rate of 0.34% in phase two of our study is compares favourably to other published studies, partly due to the suitability of regional and local anaesthesia in hand surgery and the minimal impact on patient mobility. Goodman et al found an even lower rate of 0.15% based on a 30 day reoperation and/or admission rate in an elective hand surgery population (9). The majority of their admissions/operations happened in the second post-operative week and these were mostly due to infection. This usually takes longer than 48 hours to present, and therefore there may be a group of patients in our cohort who were admitted later than 48 hours post op and are therefore not identified by our study. Furthermore, some complications can present much later such as tendon rupture.
Lack of suitable social support can sometimes prevent safe discharge – accounting for 5 cases of unplanned admission in this study – but this can usually be pre-empted and suitable arrangements made. Others have also found social reasons to be a factor in unplanned admission (5, 10, 12, 13, 16).
Some of our patients may have had a minor complication and presented to their general practitioner rather than the hospital, and these patients would not have been captured by the study.
Duration and timing of surgery are also risk factors for unplanned admission. Both Garcea and Soler-Dorda found that unplanned admissions/readmissions had significantly longer operation times (7, 11). Surgery in the afternoon was a negative factor in our study. Thus one way of reducing unplanned admissions could be to undertake longer, more complex and bony surgeries earlier in the day. Smaller cases, that are less likely to require an overnight stay, can be done in the afternoon.
We found no particular trends in patient factors such as age, ASA grade or number of comorbidities in the admitted group. In contrast, Soler-Dorda found age >65, and Minatti age >90 to be statistically significant risk factors (11, 14). An ASA greater than 2 has been associated with higher admission rates (11, 12).
Obstructive sleep apnoea in children has also been identified as possible risk factors for admission (12), but Bryson found no such association with obstructive sleep apnoea in adults (17).
Administration of general anaesthesia was another risk factor for admission. This finding helped to inform and drive further development of the regional anaesthesia service in our unit, and was addressed by the third of our interventions after phase one. Most hand patients undergoing hand surgery do not need to have a general anaesthetic, making them ideal candidates for daycase surgery. Most patients in our study who had combined general and regional anaesthesia had experienced an inadequate regional block, but this block may well have helped their post-operative pain. For safe discharge and effective post-operative analgesia, we recommend that general anaesthesia alone is insufficient, especially for bony surgery.
Our study is limited by the lack of a control group, which would more robustly have identified risk factors for admission. We studied readmission rates at 48 hours post-discharge. This identified early post-operative problems such as pain and nausea, but will not have captured infections as these will generally represent later. We did not set out to establish infection rates, which are known to be low in hand surgery in general (9).
The cost of our interventions was minimal. The development of a patient information leaflet cost very little, and the majority of patients buy their own ibuprofen over-the-counter.
Coding errors have reduced in our unit thanks to a new patient administration and tracking system. Patients are discharged or transferred electronically, reducing the potential for errors, improving the information available to general practitioners and other healthcare providers and providing a more robust audit trail.
Low cost improvements in post-operative pain control and anaesthetic techniques resulted in a demonstrable improvement in unplanned admission/readmission rates in our centre. Similar interventions could be undertaken in other units for the mutual benefit of patients and healthcare providers.
References
- Royal College of Surgeons of England. Commission on the provision of surgical services. Guidelines for day case surgery. London: HMSO, 1992.
- Peplow J, Randall E, Campbell-Cole C, Kamdar R, Petzer E, Dhillon P, Mergatroyd F, Scott P. Day-case device implantation – A prospective single-center experience including patient satisfaction data. Pacing Clin Electrophysiol. 2018 May;41(5):546-552.
- Ridings LM, Colby JM, Burch NE. Evaluation of patient satisfaction following percutaneous endoscopic gastrostomy (PEG) insertion: day case versus in-patient model in UHCW NHS Trust. Gut 2014;63(Suppl 1):A229.
- Tysome JR, Padgham ND. A comparative study of patient satisfaction with day case and in-patient major ear surgery. J Laryngol Otol. 2006 Aug;120(8):670-5.
- Aldwinckle RJ1, Montgomery JE. Unplanned admission rates and postdischarge complications in patients over the age of 70 following day case surgery. Anaesthesia 2004 Jan;59(1):57-9.
- Barros AL, Duque MR, Nunes F, Ribeiro S, Ventura C, Assuncao JP. Five year retrospective study of unanticipated admission after ambulatory surgery. Eur J Anaesthsiol, 2014 Jun;31(SUPPL. 52):27.
- Garcea G, Majid I, Pattenden CJ, Sutton CD, Neal CP, Berry DP. Predictive factors for unanticipated admission following day case surgery. J Eval Clin Pract. 2008 Feb;14(1):175-7.
- Gold BS, Kitz DS, Lecky JH, Neuhaus JM. Unanticipated admission to the hospital following ambulatory surgery. JAMA 1989 Dec 1;262(21):3008-10.
- Goodman AD, Gil JA, Starr AM, Akelman E, Weiss AC. Thirty-Day Reoperation and/or Admission After Elective Hand Surgery in Adults: A 10-Year Review. J Hand Surg Am 2018 Apr;43(4):383.e1-383.e7.
- Hardman DTA, Patel MI, Yiing D, Warden JC. The unplanned admission: a review of the daycase experience. Ambulatory Surg 1997(5):21-4.
- Soler-Dorda G, San Emeterio Gonzalez E, Martón Bedia P. Risk factors for unplanned admission after ambulatory laparoscopic cholecystectomy. Cir Esp. 2016 Feb;94(2):93-9.
- Whippey A, Kostandoff G, Ma HK, Cheng J, Thabane L, Paul J. Predictors of unanticipated admission following ambulatory surgery in the pediatric population: a retrospective case-control study. Paediatr Anaesth 2016 Aug;26(8):831-7.
- Zulfiquer FA, Pattanayak K. Evaluation of unplanned admission following day surgery at a new surgical centre in London. Ambulatory Surg 2009 Nov;15.4:93-96.
- Minatti WR, Benavides F, Capelino P, Ramos R, Premoli G, Statti M. Postdischarge unplanned admission in ambulatory surgery – a prospective study. Ambulatory Surg 2006(12):107-12.
- Cardosa M, Rudkin GE, Osborne GA. Outcome from day surgery knee arthroscopy in a major teaching hospital. Arthroscopy 1994; 10: 624-629.
- Deshpande S, Watts J. Unanticipated admission following day surgery. Anaesthesia 1998 Oct;53(10):1033-4.
- Bryson GL, Gomez CP, Jee RM, Blackburn J, Taljaard M, Forster AJ. Unplanned admission after day surgery: a historical cohort study in patients with obstructive sleep apnea. Can J Anaesth 2012 Sep;59(9):842-51.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29261/jones.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse8
The Journal of One-Day Surgery considers all articles of relevance to day and short stay surgery. Articles may be in the form of original research, review papers, audits, service improvement reports, case reports, case series, practice development and letters to the editor. Research projects must clearly state that ethics committee approval was sought where appropriate and that patients gave their consent to be included. Patients must not be identifiable unless their written consent has been obtained. If your work was conducted in the UK and you are unsure as to whether it is considered as research requiring approval from an NHS Research Ethics Committee (REC), please consult the NHS Health Research Authority decision tool at http://www.hra-decisiontools.org.uk/ethics/.
Articles should be prepared as Microsoft Word documents with double line spacing and wide margins. Submissions must be sent by email to the address below. A scanned letter requesting publication signed on behalf of all authors must also accompany articles.
Any source of funding should be declared and authors should also disclose any possible conflict of interest that might be relevant to their article.
Title Page
The first page should list all authors (including their first names), their job titles, the hospital(s) or unit(s) from where the work originates and should give a current contact address for the corresponding author.
The author should provide three or four keywords describing their article, which should be as informative as possible.
Abstract
An abstract of 250 words maximum summarising the manuscript should be provided and structured as follows: Introduction, Methods, Results, Conclusions.
Main article structure
Manuscripts should be divided into the following sections: Introduction, Methods, Results, Discussion and References. Tables and figures should follow, with each on a separate page. Each table and figure should be accompanied by a legend that should be sufficiently informative as to allow it to be interpreted without reference to the main text.
All figures and graphs are reformatted to the standard style of the journal. If a manuscript includes such submission, particularly if exported from a spreadsheet (for example Microsoft Excel), a copy of the original data (or numbers) would assist the editorial process.
Copies of original photographs, as a JPEG or TIFF file, should be included as a separate enclosure, rather than embedding pictures within the text of the manuscript.
Tables, Figures and Graphs:
Please submit any figures, graphs and images as separately attached files rather than embedding non-word files into the word manuscript document. Tables constructed in MS Word can be left in their original MS Word file including the manuscript if this is where they were drawn.
Figures and graphs can be presented in colour but try to avoid 3-d effects, shading etc. Figures and graphs may be redrawn if the quality is not in keeping with the Journal. Please make it clear within the manuscript text where you would like tables, graphs or images to be placed in the finished article with the use of a brief explanatory legend in the manuscript file where you wish the item to be placed, e.g.
Table 1. Patient demographic details.
Figure 1. Proportion of procedures performed as a day-case each year between 2005 and 2018.
Photographs
Photographs can be provided as jpg or tiff files but should be included as a separate enclosure, rather than embedded within the text of the manuscript. This ensures higher quality images. However, we will accept images within Word documents but image quality might suffer!
References
Please follow the Vancouver referencing style:
- References in the reference list should be cited numerically in the order in which they appear in the text using Arabic numerals, e.g. 1, 2, 3, 4 etc.
- The reference list should appear at the end of the paper. Begin your reference list on a new page and title it 'References.'
- Cite articles in the manuscript text using numbers in parentheses and the end of phrases or sentences, e.g. (1,2)
- Abbreviate journal titles in the style used in the NLM Catalogue: https://www.ncbi.nlm.nih.gov/nlmcatalog?Db=journals&Cmd=DetailsSearch&Term=currentlyindexed%5BAll%5D
- The reference list should include all and only those references you have cited in the text. (However, do not include unpublished items such as correspondence).
- Check the reference details against the actual source - you are indicating that you have read a source when you cite it.
- Be consistent with your referencing style across the document.
Example of reference list:
- Ravikumar R, Williams J. The operative management of gallstone ileus. Ann R Coll Surg Engl 2010;92:279–281.
- Dybvig DD, Dybvig M. Det tenkende mennesket. Filosofi- og vitenskapshistorie med vitenskapsteori. 2nd ed. Trondheim: Tapir akademisk forlag; 2003.
- Beizer JL, Timiras ML. Pharmacology and drug management in the elderly. In: Timiras PS, editor. Physiological basis of aging and geriatrics. 2nd ed. Boca Raton: CRC Press; 1994. p. 279-84.
- Kwan I, Mapstone J. Visibility aids for pedestrians and cyclists: a systematic review of randomised controlled trials. Accid Anal Prev. 2004;36(3):305-12.
- Barton CA, McKenzie DP, Walters EH, et al. Interactions between psychosocial problems and management of asthma: who is at risk of dying? J Asthma [serial on the Internet]. 2005 [cited 2005 Jun 30];42(4):249-56. Available from: http://www.tandf.co.uk/journals/.
Submissions are subject to peer review. Proofs will not normally be sent to authors and reprints are not available.
All submissions should be emailed to The Editor: davidbunting@nhs.net
Mr David Bunting
Editor, Journal of One Day Surgery
Consultant Upper GI Surgeon
North Devon District Hospital
[These guidelines were last revised on 05.11.2018]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29928/284-author-guidelines.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1795#collapse9