Dave Bunting
This month, the NHS Chief Executive Sir Simon Stevens and NHS Improvement Chief Operating Officer Amanda Pritchard wrote a letter to NHS leaders calling for Trusts to recover at least 80% of their last year’s activity for outpatient/day case procedures (in addition to short-stay overnight elective procedures). It is vital that day surgery pathways are prioritised as they have huge potential to help in meeting this demand. Many day surgery units are ideal environments to open as ‘green’ zones where COVID negative patients can be brought in for treatment and discharged on the same day, with minimal impact on other hospital departments and bed occupancy. It is essential, therefore, that NHS Trusts prioritise the re-opening and ring-fencing of day surgery beds so productivity can be increased.
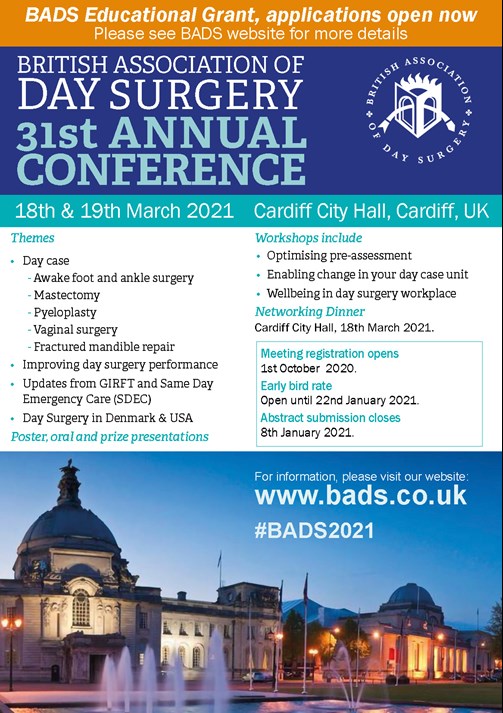
Readers will probably be aware by now that the Annual Conference has now been rescheduled to take place on 18th-19th March 2021 at the Cardiff City Hall. There is a new abstract submission deadline of Friday 8th January 2021. This is the link to abstract submission:
https://app.oxfordabstracts.com/login?redirect=/stages/1625/submissions/new
This year BADS again plans to co-host several national and regional meetings in association with external organisations such as Health Care Conferences UK (HCUK). The conference environment has gone through important and necessary changes this year due to COVID restrictions and whilst the normal group audience meetings cannot be held in the same way, these changes offer exciting opportunities to host meetings in different ways to generate novel educational experiences. The HCUK meetings this year will be held as hybrid events offering a web-based virtual conference experience in addition to on-site attendance. Reduced dependence on individual travel and on-site presence offers the possibility of bringing conferences to a much larger audience.
- BADS/HCUK Conference on Day Case Major Knee Surgery will be held on Monday 5th October 2020 at the De Vere W1 Conference Centre, London
- BADS/HCUK Conference on Day Case Total Hip Replacement will be held on Wednesday 4th November 2020 at the Studio Conference Centre, Birmingham
- BADS/HCUK Conference on Day Surgery in Gynaecology will be held on Thursday 19th November 2020 at the De Vere W1 Conference Centre, London
- BADS/HCUK Conference on Breast Surgery as Day Surgery will be held on Tuesday 1st December 2020 at the Studio Conference Centre, Manchester
- BADS/HCUK Conference on Developing your Daycase General Surgery Service will be held on Friday 4th December 2020 at the De Vere West One Conference Centre, London
Further details of all the above conferences can be found in this edition of JODS.
Original papers in this edition of JODS include two original articles on the topic of day case mastectomy. One discusses the benefits of using Fibrin Sealant Spray to reduce the routine use of drains and increase daycase rates; and the other describes a service improvement project successfully increasing the daycase mastectomy rate after introducing a programme of education. The Royal Wolverhampton NHS Trust have produced a report demonstrating the feasibility and safety of daycase/short-stay laparoscopic cholecystectomy in patients with morbid obesity supporting the BADS view that obesity should not be a barrier to daycase surgery. The Torbay and South Devon NHS Foundation Trust is one of few trusts in the UK regularly performing daycase shoulder surgery and describe how remarkably high (>90%) daycase rates can be achieved in their publication of a case series. Finally, the Royal Cornwall Hospitals NHS Trust are one of the highest performers nationally in daycase fundoplication surgery and present their data on over 200 cases performed with a daycase rate of over 85%.
Some years ago, BADS commissioned a series of ‘How I do it’ guides for publication in JODS. Each guide is presented as an - easy to digest - single page document, covering anaesthetic technique, surgical technique, peri-operative analgesia, take home medication, organisational issues, common pitfalls, and anticipated day case rates. The guides have been updated for this year and we will be publishing them over the next few JODS issues starting with the following guides in this edition:
- ‘How I do it - Laparoscopic Cholecystectomy’
- ‘How I do it - Laparoscopic hysterectomy’
- ‘How I do it - Laparoscopic Nephrectomy’
Please keep your submissions to the journal coming in and remember – JODS still offers citable peer-reviewed publication with no author processing fees. Author guidelines and submission instructions can be found in this edition of the journal.
Finally, please enjoy this edition of JODS, looks after yourselves and stay safe.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/41286/303-editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse0

Kim Russon
It is now the summer holiday season so I hope many of you have managed to get a well-earned break and enjoy some of the hot and sunny weather the UK has recently been experiencing. Nationally the prevalence of covid19 has been falling and some hospitals, have thankfully not had a positive inpatient for a little while. I am, however, mindful that things have not returned to normal.
Now comes a new challenge to the NHS – the recovery of planned surgery. A few months may not sound like long but now we realise just how much “routine” surgical activity previously occurred every day prior to the covid19 pandemic. In a letter to all NHS Trusts Simon Stevens, NHS Chief Executive and Amanda Pritchard, NHS Chief Operating Officer set out the priority to “Recover the maximum elective activity possible between now and winter making full use of the NHS capacity currently available as well as re-contracted independent hospitals”. There was recognition of the covid related capacity restraints. The goal that has been suggested is that “in September at least 80% of last years activity for both overnight and day case procedures rising to 90% in October” should be achieved.
This poses a huge opportunity for progressing day surgery. As BADS members, the benefits and processes of a day surgery pathway is not news to you. However, this is not necessarily the case everywhere and I urge you to engage with your local Trust or STP/ICS to further develop your day surgery pathways to increase day case rates and help reduce hospital waiting lists. The importance of treating as many patients on a day surgery pathway has been recognised by NHSE through their Adopt and Adapt programme and by Get It Right First Time (GIRFT) implementation programmes and I have had the privilege of being involved in both workstreams. This month BADS has completed a draft “National Day Surgery Delivery Pack” written in collaboration with Centre of Perioperative care (CPOC) and GIRFT. We hope that it will not be too long before this can be released.
Please encourage your colleagues to visit the BADS website https://daysurgeryuk.net/en/home/. It is an informative resource and we are continually adding links to useful websites relating to restarting planned surgery. The BADS Dataset 2020 has just been published and Edition 2 of Day Case Hip and Knee Replacement booklet is to be published at the end of this month. Recently popular BADS booklets have been Spinal Anaesthesia for Day Surgery Patients: A Practical Guide and Nurse Led Discharge, as well as the Directory of Procedures 6th Edition which lists over 200 procedures that are suitable to be performed as day case. BADS booklets can all be purchased via the website.
BADS / HCUK conferences are also an excellent learning opportunity and they are now available to attend virtually should you prefer to do this. I do hope you can join us for some of them.
Another useful resource about to be published on the 1st September 2020 is The Royal College of Anaesthetists Quality Improvement Book https://www.rcoa.ac.uk/safety-standards-quality/support-anaesthetic-departments/quality-improvement-book. I'm grateful for all of the hard work from the authors and members of BADS council to produce the 10 day surgery RCoA QIPs / audit recipes.
As always JODS is an incredible source of information and I’m delighted to see the return of the “How do I do it “series with revised versions in this edition and new ones commissioned. Thank you to everyone involved in the production of JODS and thank you to everyone who reads it, I hope you enjoy it as much as I do. Please stay safe and well and get some rest when you can.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42061/303-president.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse1
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40090/2021-prog-3.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse3
Download the 2021 Conference pdf by clicking
the link at the bottom of the page.

Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40104/2021-prog-1.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse4
Claire Blandford1 & Veronica Conboy2
1Consultant Anaesthetist, 2 Consultant Orthopaedic Surgeon
Torbay & South Devon NHS Foundation Trust
Corresponding author: Dr Claire Blandford, Consultant Anaesthetist, Torbay & South Devon NHS Foundation Trust, Lawes Bridge, Torquay, TQ2 7AA. Email: claireblandford@nhs.net
Keywords: Developing new services; shoulder replacement; translational learning
Abstract
Torbay hospital is a medium sized district general hospital in South West England with three upper limb specialist orthopaedic surgeons. Having successfully instituted a pathway for day surgery hip replacement in September 2018, we were able to translate learning from this to our care pathway for shoulder replacement. This account details our day surgery shoulder arthroplasty pathway and exemplifies an approach to transforming inpatient to day surgery pathways which could be extrapolated to other procedures or disciplines.
Introduction
Over 11,500 daycase procedures are done annually at Torbay hospital and the day surgery unit is nationally respected for its ethos and outcomes. We regularly perform uni-compartmental knee replacement (national top performer), laparoscopic hysterectomy, paediatric tonsillectomy, and transurethral resection of prostate surgery as day case procedures.
We are a medium sized district general hospital in the South West of England. Our day surgery unit comprises four operating theatres and ancillary space, self-contained but physically connected to the main hospital. We perform more daycase procedures per year than we can presently accommodate within our dedicated day surgery theatre capacity and as such we have a long established pathway whereby patients may have their surgery in inpatient theatres and be transferred to the day surgery unit for completion of their recovery and subsequent discharge home. The existence of this practice has allowed us to widen it to those patients requiring surgery or procedures in specialist theatres (in this case, laminar flow).
Annually as a trust we perform approximately 50 elective upper limb joint replacements; typically, 42 shoulder replacements and 8 elbow replacements. National Joint Registry data shows our patient demographic has a higher than national average representation of ASA3+ patients (American Society of Anaesthesiologists Physical Status classification system) undergoing upper limb joint replacement procedures; 45% ASA3+ vs national average of 29% for shoulders and 47% ASA3+ vs 33% for elbow replacement [1].
Translational learning
In September 2018 we successfully introduced day case hip replacement in our trust. This was a multi-professional team endeavour involving anaesthetists (myself, Dr A Bougeard & Dr M Stocker), surgeon (Mr M Kent), nursing (Mrs J Allen & Mrs A Alen) and physiotherapy (Mrs B Sullivan).
The pathway has the following features:
- meticulous pre-assessment and preparation
- utilising our pre-existing joint school to include appropriate counselling about day case discharge
- use of a short acting prilocaine spinal
- regular antiemetics
- intra-operative goals of normothermia, normovolaemia, blood conservation.
- post operatively a supported discharge with physio input ensuring patient confidence in mobilisation
- early post op follow-up in the community delivered by a dedicated team of orthopaedic outreach nurses
- bespoke analgesia regimen clearly communicated to promote confident self-management by the patient
To date we have performed 30 cases with 93% same day discharge and no complications. The two patients in our Total Hip Replacement (THR) cohort to date that failed day-case discharge were the two patients where there was deviation from the care protocol.
The idea
In the upper limb team, we began to consider if we could start offering total shoulder replacements as day case procedures in our trust. Learning and experience from the hip and other complex day surgery procedure pathways is that medical co-morbidities can be optimised, and techniques adjusted for, and are often not the barrier. In a well-planned case with a suitable operation and surgical technique, appropriate anaesthetic technique, high quality analgesia, and adequate time for recovery with appropriate support and rehabilitation, then day case discharge is likely to be achievable. A key requisite is patient engagement and belief in the pathway – the moment a patient doubts it, or staff in contact with the patient are not universally supportive the chance of day case discharge decreases sharply.
Assessing current practice for pathway redesign
Introducing a new clinical pathway often represents an adaptation of an existing pathway rather than de novo creation. A pathway that facilitates same day discharge will contain the same elements as an inpatient pathway, but they may need to be provided for differently.
By looking at what is currently happening during an inpatient stay, the requirements for a day case pathway can be established.
- Why are your patients staying overnight in hospital? - is something active being done? – if so, might that activity be able to be done in the community by a district nurse, an outreach nurse from the hospital or by a next day outpatient appointment?
- Are they staying in hospital simply because that is what has always happened before?
- Are they in pain? – then review your current management and see if a pain protocol can be developed that allows patients to continue effective analgesia in their own homes?
- Is nausea a problem?
- Is urinary retention a problem?
Social and psychological support for patients is important – it requires good communication at every stage; appropriate and consistent written and verbal information; contact details and confidence in response in case of concerns. Historically all our day case patients have received a day 1 follow-up phone call from our day surgery nurses: wellbeing status, satisfaction and feedback are recorded, and any questions answered. This additional information, over the years, has given us an extensive database of direct patient feedback which informs our refinement of pathways and processes. We also planned to supplement this with additional patient feedback to support the learning around new pathway introduction.
The reality
Our first daycase shoulder replacement patient had their surgery in June 2019. Having discussed the idea of doing a pilot daycase shoulder replacement case for a couple of months it transpired that our first suitable case was a revision procedure.
The patient was a woman in her early 50s who had undergone hemiarthroplasty replacement for inflammatory arthropathy 2.5 years previously (as she had rotator cuff deficiency and was thought at that stage too young to consider primary reverse arthroplasty). Unfortunately, after early promising pain relief she developed significant pain due to glenoid erosion. Inflammatory markers, aspiration and Synovasure for possible infection were all negative and she was listed for a one-stage revision to a reverse polarity shoulder replacement. In all other aspects she was ideal, highly motivated and engaged with idea of day surgery. Relevant past medical history included both rheumatoid and psoriatic arthropathy but no cardiac, respiratory, or renal disease. Her regular medications included methotrexate, TNF inhibitor (Adalimumab, which was stopped two weeks pre op), co-codamol and gabapentin.
Pre-op
Our index case was identified at point of listing and was receptive to the idea of day surgery when the idea was raised: she valued being able to rapidly return to her own environment to complete her recovery from surgery. As a team we had the advantage of both having met her before as we had been the operating surgeon/anaesthetist for her primary hemiarthroplasty procedure. At consent clinic it was reinforced that the plan for her surgery was day case but with reassurance that would only go ahead if all were well and that both we and the patient were happy with that.
On the day; anaesthesia
The patient underwent standard pre-operative preparation on our admissions ward and had taken her carbohydrate pre-op drinks as advised. She was given oral pre-medications of Paracetamol 1g and Oxycodone MR 10mg.
The anaesthetist performed their standard anaesthetic technique for shoulder replacement; an awake in-plane ultrasound guided upper trunk interscalane block in combination with a superficial cervical plexus block (0.25% levobupivacaine; total volume used 30mls) followed by induction of general anaesthesia with TCI Propofol + Remifentanil. The patient was intubated with a RAE 7.0 endotracheal tube. Other drugs administered included rocuronium single dose at intubation (30mg), dexamethasone (6.6mg), ondansetron (4mg), teicoplanin (400mg), gentamicin (240mg) and tranexamic acid (1g).
The surgery was performed in beach chair position with pressure controlled-volume guaranteed ventilation (PCV-VG) at 6mls/kg. The rest of her anaesthetic management included active patient warming throughout (forced air blanket + fluid warmer) cell salvage collection (insufficient volume collected to warrant processing) and use of foot pumps to reduce venous thromboembolism risk. Total volume of IV fluids administered was 1500mls. The patient was not catheterised.
The patient was listed as the first case on our theatre list. Her anaesthetic start time was 09.03 and we transferred into theatre at 09.21. Preparation, positioning, time out and draping was performed, and incision was at 10.02. Total surgical time was 2hours 28mins. The patient was extubated in theatre and then transferred to our main theatre primary recovery area at 12.40. She was alert and conversant rapidly and confirmed she was comfortable. A build up drink (Fortisip) was provided and oral fluids commenced. Shortly after this she was transferred to our day surgery unit to complete her recovery.
She was discharged home at 17.59hrs, 5 hours 20mins after leaving theatre.
Discharge medication included: oxycodone 10mg MR bd 2/7 (5 tablets only issued); ondansetron 4mg tds 2/7; paracetamol 1g qds 5/7; macrogols bd 5/7. On day 3 analgesia was stepped down to codeine qds.
The post-discharge analgesia plan was modelled on our successful day case hip replacement pathway.
(Obviously, there can be some concern about sending patients home with strong opioids and potential for addiction. We have a dual documentation approach to this whereby there is an automated entry on the computerised GP discharge summary as well as dedicated patient documentation which reinforces the non-continuation of this medication after the initial 5 doses.)
When developing the patient pathway for our daycase hips a patient medication administration sheet was developed which tabulates when next doses are due and gives patients explanations of what each of their issued TTA medications are for, dose frequency and duration. Feedback from this was that it was highly user friendly and patients felt supported and confident in self-managing their pain control at home.
This chart has been adapted for our shoulder replacement pathway. In addition to information on self-administered analgesia, patients are also given post-operative information about caring for their ‘numb’ arm along with contact information for support/concerns.
On the day; surgical aspects
The surgical procedure was revision of an uncemented Epoca hemiarthroplasty to an Exactech reverse shoulder replacement (uncemented). It was performed by standard surgical technique via a deltopectoral approach. There were no surgical complications. Post op X-Ray was performed and reviewed by the surgeon before the patient was discharged.
Post op
Telephone feedback was taken on days 1, 4 and 7. The patient reported herself absolutely delighted with her care and experience as a day case and felt her care had been friendly and efficient and she had been well supported throughout. Her nerve block wore off overnight on the day of surgery (approximately 15hours) and there was zero sensory or motor deficit by 24 hours post op. At this point she had had two doses of oxycodone (10mg as a pre-med and 10mg at 1900hrs on day 0). Her pain was well controlled, and she found the transition when her block wore off very manageable. She reported feeling ‘Very Good’ and quoted ‘none’ when asked about her level of pain. When she stepped down to the codeine, she reported that her pain control was satisfactory, but she felt more sleepy. No nausea, vomiting or dizziness was experienced at any time. She was able to stop the codeine before day 5. Under guidance from her GP she had also started to slowly wean the gabapentin she had been on before her surgery.
Surgical follow up at 6 weeks showed excellent progress. The patient was completely pain free. Her range of functional movement was improving with physiotherapy & strengthening exercises.
The future
As shown with our hip experience, achieving these procedures as day cases is about building an effective pathway that allows the same high-quality operation to be performed alongside active patient engagement to create a safe and acceptable care pathway. We were able to translate learning from our daycase hip pathway to help shape the design of this pathway - particularly the analgesia and post-operative patient information provision for patients.
Given the increasing pressure on NHS services and the escalating demand for orthopaedic procedures, often compounded by rising waiting list times due to winter bed pressures and cancellations, being able to successfully perform a given procedure as a day case offers significant advantages both to the trust and the patient. Previously published articles have demonstrated patient acceptance and feasibility for daycase shoulder arthroplasty [2]. Indeed, significant reductions have been reported for post-operative complications and 30-day mortality rates in matched cohorts when comparing total shoulder replacement as a short stay procedure versus an inpatient stay [3]. In Duchman et al’s review, out of numerous variables studied only ‘inpatient stay’ was independently identified as a risk factor for 30 day mortality in total shoulder arthroplasty; age, diagnosis of COPD, functional status (dependent/independent) and ASA (1-2/ 3-4) all had odds ratios with 95% confidence intervals spanning 1.
The drive to translate historically inpatient surgical procedures to day case ones where possible is not just founded on economics, it often translates into health benefits for the patients and excellent patient satisfaction. Our day surgery unit has a motto, “the best bed is your own bed’. Continuous innovation is at the heart of care planning for the future.
We are still at the start of our journey with daycase shoulder replacements but aim to continue. We have since identified a further four patients from our current waiting list and successfully performed two more daycase shoulder replacements (including one since COVID precautions). Our current daycase discharge rate is 100%. As we progress, we will continue to learn and refine our processes. We would encourage other centres to look at their current care pathways and consider what changes could be made to facilitate day surgery pathways.
References
- National Joint Registry, 36-month practice profile- Torbay Hospital. Accessed via www.surgeonprofile.njrcentre.org.uk on 6th January 2020.
- Leroux TS et al. Safety and patient satisfaction of outpatient shoulder arthroplasty. JESS Open Access. 2018 Feb 15;2(1):13-17. doi: 10.1016/j.jses.2017.11.002. eCollection 2018 Mar.
Accessed via https://www.ncbi.nlm.nih.gov/pubmed/30675561 on 19 October 2019 - Duchman KR, Anthony CA, Westermann RW, Pugely AJ, Gao Y, Hettrich CM. Total Shoulder Arthroplasty: Is Less Time in the Hospital Better? Iowa Orthop J. 2017;37:109–116.
Accessed via www.ncbi.nlm.nih.gov/pmc/articles/PMC5508292/ on 19 October 2019
NOTE: Patient consent for this report publication has been sought.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40116/303-translating-learning-to-achieve-day-case-total-shoulder-arthroplasty.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse5
Miss Gwen Bromley Specialist Registrar, Queen Elizabeth Hospital Gateshead
Dr Claudia Wilson Foundation Doctor, Queen Elizabeth Hospital
Miss Annie Chan Specialist Registrar, Queen Elizabeth Hospital Gateshead
Mr Mujahid Pervaz Consultant Oncoplastic Breast Surgeon, Queen Elizabeth Hospital Gateshead
Corresponding Author. Email: Gwen.bromley@nhs.net
Keywords: Mastectomy; Day Case; Target; Same Day Discharge
Acknowledgements Mr S Amonkar, Mr K Clarke, Ms T Fasih, Ms L Jalini, Mr R Milligan
Abstract
Introduction: Mastectomies are a common procedure in the management of breast cancer. National guidelines now recommend that we aim to carry out 50% of mastectomy procedures as day-cases. We evaluated all mastectomies carried out during a 6-month period after the introduction of a programme of education. Specifically investigated, was the frequency of day-case mastectomies highlighted as an area requiring considerable improvement following a previous study.
Methods: mRetrospective cohort analysis using electronic patient records for all patients who underwent mastectomy over a defined 6-month period.
Results: Data from 82 patients collected with an average age of 58. Overall rate of day-case mastectomy was 54.9%, including patients with immediate reconstruction and nodal procedures. 62% of patients who underwent simple mastectomy had their procedures performed as day-cases compared to 35% of patients in 2017. Mean length of stay decreased for all types of mastectomy over this period compared to previous.
Conclusion: The rate of day-case mastectomy improved significantly. This can be attributed to a drive-in managing patient expectation and re-education of staff. However, many factors still contribute to overnight stay such as post-operative intravenous antibiotics and the use of drains. Optimising theatre lists and careful planning will allow maximum recovery time for mastectomy patients and improve the chances of a day-case outcome.
Introduction
Mastectomies are carried out regularly in the UK for the treatment of breast cancer. These procedures historically required prolonged hospital stays post-operatively, however there is currently a drive towards carrying out most mastectomies as day-case procedures. Indeed, the British Association of Day Surgery (BADS) released national targets stating that 50% of simple mastectomies, with or without axillary procedures, should be performed as day-case procedures [1]. Most clinicians are keen to encourage day-case surgery both for improved patient satisfaction, but also to maximise financial benefits.
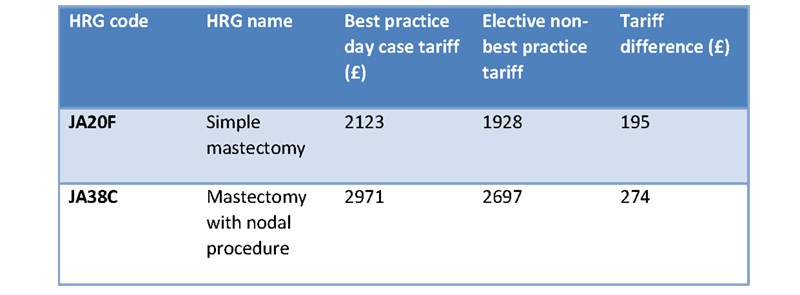
The financial incentives for day-case mastectomy surgery are considerable, both regarding tariffs and excess bed-day cost. If mastectomies are carried out as day-cases (under the payment by results system) the best practice tariff is received. For a simple mastectomy, the day case tariff is £2123 compared to the inpatient tariff of £1928, representing a saving of £195 per patient. Similarly, for a mastectomy with a nodal procedure the day-case tariff is £2971 compared to £2697, representing a saving of £274 per patient, see Table 1 [2]. Furthermore, the excess bed day cost is estimated to be £300 per patient per day. These savings are significant, especially given the frequency of mastectomy in breast surgery practice.
Table 1: Best Practice Day Case Tariff Rates for mastectomies [2]
A retrospective study was undertaken at our UK centre. We are a high-volume breast screening unit and therefore perform a moderate number of mastectomies each year. This study evaluated all mastectomies carried out over a 6-month period looking specifically at how many of these were performed as day-cases and specific reasons for those that resulted in a post-operative overnight stay.
Over the study period, 106 mastectomy cases were performed and of these, 35% were day-cases. This percentage was well below the 50% target set out by BADS. It is suggested that the top 5% of centres in the UK should achieve day-case mastectomy rates of 44% for simple mastectomies without axillary surgery and the top 25% of centres achieving a day-case rate of 12%. BADS also make a recommendation for mastectomy with axillary surgery; the top 5% of centres achieving rates of 42% for day-case procedures and similarly the top 25% having rates of 11% [1]. Therefore, our centre was performing within the top 25% of centres, however, was falling short of the top 5% of centres.
Reasons as to why we were falling short of the top 5% of performing centres nationally were discussed and efforts were made to educate the breast surgery department (clinicians and breast care specialist nurses) in the advantages of day case mastectomy for both patient satisfaction and the financial benefits for the trust. We focussed heavily on shifting patient expectations and ensuring that, where appropriate, patients would be counselled from the outset that their procedures would be carried out as day-case procedures and that this is now standard operating practice across the department. The two study periods were compared to see if improvements had been made, specifically in day case mastectomy rate.
Methods
Patient details were collected for all patients who were coded as having a ‘mastectomy’ procedure over a 6-month period and a retrospective analysis of these patients was carried out. We used electronic patient records to collect our data from operation notes and GP handover letters and collected the data in the same format as our initial study.
Results
Over the re-audited period, 90 patients were coded as ‘mastectomy’. Of these, 8 were excluded due to being incorrectly coded, for example some cases were ‘revision of mastectomy scar’. Therefore 82 patients were included in our data set, 80 of these were female and 2 were male. 24 patients had immediate reconstruction surgery. 43 patients had simultaneous sentinel lymph node biopsies (SNLB), 22 had axillary node clearances (ANC) and 18 had no nodal surgery. The average age of our patients in this cohort was 58 with 17 patients aged 75 or over.
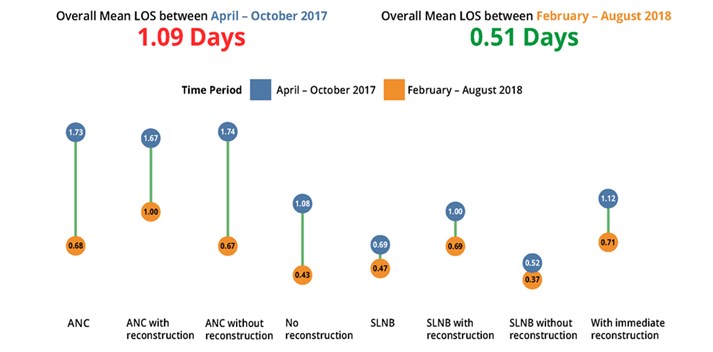
Of the 82 cases, 45 were carried out as day-cases. This gave an overall day-case rate for all mastectomy procedures of 54.9%. Indeed, the mean length of stay (LOS) for all types of mastectomy decreased from 1.09 to 0.51 over the two study periods. Of the cases which were ‘simple mastectomies’, 62% of these were carried out as day-cases.
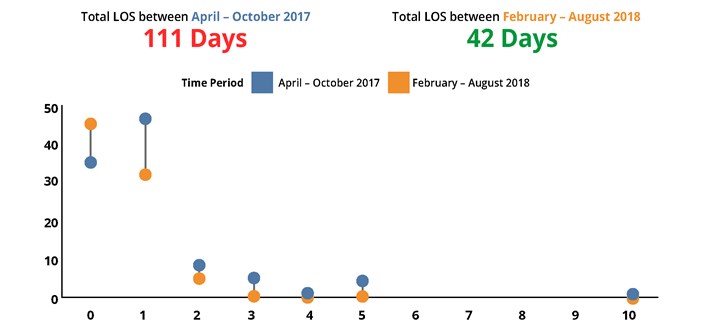
Mean LOS improved for all mastectomy procedures, be that with nodal clearance or reconstruction, see Figure 1.
Figure 1: The Difference in Mean Length of Stay Between the Two Cohorts (according to type of procedure).
Most cases in the latest cohort were carried out with a one-day hospital stay or less. The longest in-patient stay in the later cohort was 2 days, this contrasts with the results from 2017 where a higher proportion of patients stayed for 3 days or more, as shown in figure 2.
Figure 2: Change in total Length of Stay.
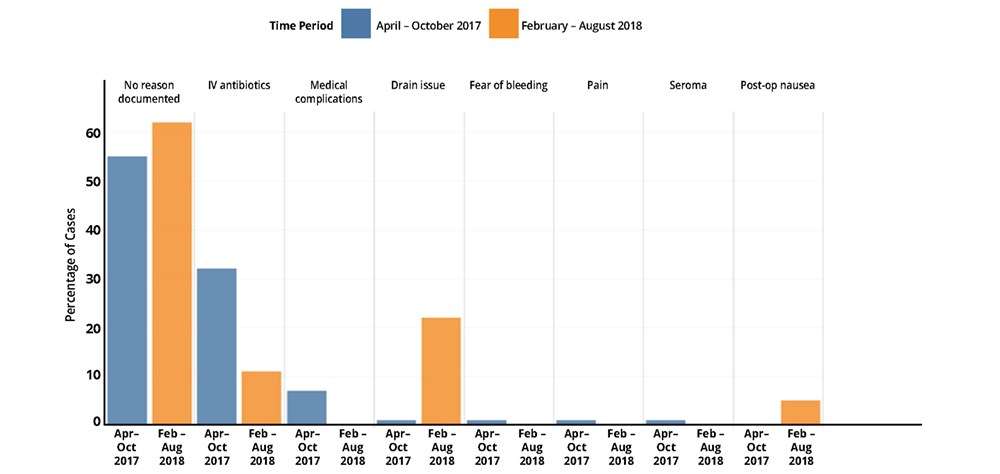
We also reviewed the reasons why patients were not discharged on the day of surgery. Unfortunately, analysis showed that in most cases these reasons are not recorded on the operation note or discharge documentation. However, the use of drains and IV antibiotics were consistently shown as reasons for patients to remain in hospital overnight. See figure 3 for a breakdown of these reasons in both cohorts.
Figure 3: Reasons Recorded for Increased Length of Stay.
Discussion
Mastectomies remain common procedures in the UK. It is an operation which is relatively short in duration with low levels of post-operative pain and minimal serious complication, therefore it is a good candidate for a day-case procedure. Indeed since 2007, as part of the Cancer Reform Strategy [3] work has been done to improve and streamline the breast cancer surgical pathway. It was noted that in doing so, length of stay could be reduced by 50% and therefore over 25% of unnecessary bed days could be released for 80% of major breast surgery [3]. The financial implications of this are remarkable. As noted earlier, the difference in tariff between the day-case and non-day case rate for a simple mastectomy is £195 [2]. With 43% of women who have surgery for breast cancer each year opting for mastectomy, this relatively small saving would lead to a monumental saving.
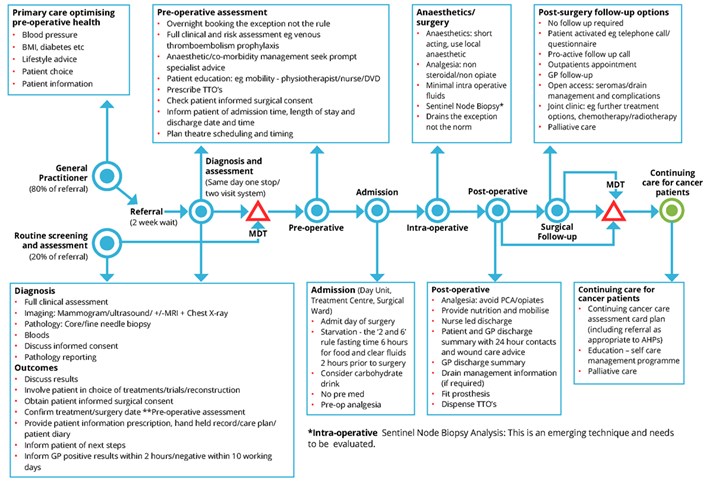
Improvements are being made on a national level. An NHS Improvement project into delivering day-case surgery safely revealed a 52% improvement in length-of-stay from 2007 to 2011. This was attributed mainly to improving the day case breast surgical pathway, as shown in figure 4.
Figure 4: Day Case Breast Surgical Pathway (excluding reconstruction) [3]
Our study observed that, although many patients who have a drain sited do still achieve a same day discharge, in a small percentage of patients the drain caused issues such as pain or significant amounts of fluid leakage which was documented as the reason for their overnight stay. The use of drains is a contentious issue with a large volume of published literature both in favour and against the use of drains. Indeed, many surgeons have adopted techniques such as quilting or tissue adhesives to avoid drain placement. In contrast, some clinicians feel that having a no-drain mastectomy is feasible and safe with no influence on seroma formation. Despite surgeon preference, no single technique has proven superiority, this remains a point for debate and further formal research is ongoing in multiple centres to provide some clarification on this for example the SAM trial [4].
Our data highlighted the prescribing of post-operative IV antibiotics as a reason for overnight stay post-mastectomy. Research into this shows that post-operative antibiotics are rarely indicated and, even in the presence of reconstructive surgery, guidelines are inconsistent and vague. This is an area where further research/clarification may assist in further reducing overnight stay post mastectomy [5].
When we discussed the results of this study, it was felt that further work should be done to look at whether the position of the mastectomy case on the list has any impact on whether the case is done as a day-case. There may be a correlation between cases done at the end of an afternoon list and a longer length of stay, simply due to observation time post-operatively. This is an area which we hope to look into more in future studies because there may be scope to prioritise mastectomies at the start of lists in order to increase the likelihood for the case to be done as a day-case.
The psychological benefit of day-case mastectomy surgery is important with many patients preferring to return to their own environment as soon as they are able. This is in addition to the other benefits of day-case surgery which are well documented such as earlier mobility and therefore decreased risk of DVT and lowered risk of hospital acquired infections [6].There is limited literature about how to best to psychologically prepare patients for breast cancer surgery and this is perhaps a field in which more work can be done.
Conclusion
This study has shown that the rate of day-case mastectomies has improved considerably at our centre and that the BADS targets are achievable. We feel that the main driving force behind our improvement in day case mastectomies comes from shifting patient expectations. We hope that by continuing to communicate more thoroughly with our patients about their anticipated journey through the mastectomy process these rates will only improve further. Inevitably some cases will require a prolonged hospital stay due to reasons beyond our control such as co-morbidities or unanticipated surgical complications leading to a deviation from the normal post-operative plan, however on the whole, day case mastectomy is an achievable and sustainable goal. It is important that improving day-case rates should not be prioritised over patient safety however where possible, day-case surgery is now the expectation and not the exception for our patients.
References
- British Association of Day Surgery (2019) Trust Performance. Available at https://daysurgeryuk.net/en/resources/trust-performance/ (Accessed June 2019)
- National Health Service (2018) National tariff payment system 2017/18 and 2018/19. Available at https://improvement.nhs.uk/resources/national-tariff-1719/ (Accessed May 29th 2019).
- National Health Service (2011) Delivering major breast surgery safely as a day case or one-night stay. Available at www.improvement.nhs.uk/cancer (accessed May 30th 2019)
- J. van Bastelaar, R. Granzier, L. M. van Roozendaal, G. Beets, C. D. Dirksen, and Y. Vissers (2018). ‘A multi-center, double blind Randomized Controlled Trial evaluating flap fixation after mastectomy using sutures or tissue glue versus conventional closure: protocol for the Seroma reduction After Mastectomy (SAM) trial.’ BMC Cancer (2018) 18:830
- Ariyan S1, Martin J, Lal A, Cheng D, Borah GL, Chung KC, Conly J, Havlik R, Lee WP, McGrath MH, Pribaz J, Young VL (2015). ‘Antibiotic prophylaxis for preventing surgical-site infection in plastic surgery: an evidence-based consensus conference statement from the American Association of Plastic Surgeons.’ Plastic Reconstruction Surgery 2015 Jun; 135(6):1723-39
- International Association of Ambulatory Surgery (YEAR/YEAR). Policy Brief- Day Surgery Making It Happen. Available at http://www.euro.who.int/__data/assets/pdf_file/0011/108965/E90295.pdf (Accessed May 30th 2019)
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40117/303-day-case-mastectomy-target-achievable-and-sustainable-for-the-future-of-the-nhs.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse6
Mr David Griffith*, Ms Alexandra Millerǂ, Mr Michael Hutton†, Mr James Clark*, Mr Allwyn Cota*, Mr Ian Finlay*, Mr Paul Peyser* and Mr Michael Clarke*
*Consultant ǂCore Trainee †Staff Grade doctor
Upper GI Surgery Department, Royal Cornwall Hospital, Truro, Cornwall, TR1 3LJ, United Kingdom
Corresponding author: Email: davidgriffith1@nhs.net
Keywords GORD; Fundoplication; Day Case
Abstract
Background: Laparoscopic anti-reflux surgery is an effective treatment for gastro-oesophageal reflux disease (GORD). Recent publications have highlighted the low national day case rate for this procedure with wide variation in conversion and volume by centre. Our unit has performed this procedure as day case since 2014 and we report our outcomes.
Method: Patients were suitable for day case, unless they had a hiatus hernia containing more than half of stomach or no adequate home support. Patients underwent pre-operative endoscopy +/- oesophageal physiology studies. A standardised evidence-based peri-operative protocol was developed after reviewing our initial experience. Patient information leaflets were provided with counselling in clinic. Nissen and anterior fundoplications were performed across 2 sites by 5 surgeons. Patients were not randomised to treatment.
Results: Since 2014 there have been 202 primary fundoplications with equal sex distribution and median age 49 years. The day case rate was 86.6%. There were 97 Anterior and 105 Nissen fundoplications. Our 2 day readmission rate was 4.95% (n=10) and 30 day readmission 8.4%, with pain (4.5%) and dysphagia (3.5%) the most common reasons for readmission. 0 cases were converted to open and there were 0 mortalities. Patients had recurrent symptoms in 11.9% however the revision surgery rate was 4%. There were no significant differences in complications between anterior and Nissen fundoplication other than gas bloat (11 (6.9%) vs 3 (2.9%) Fisher’s Exact p=0.002).
Conclusion: Using a standardised peri-operative protocol, patient counselling and early telephone follow up, a day case rate of >80% for laparoscopic anti-reflux surgery is achievable. This is in keeping with the recently published Getting It Right First Time (GIRFT) document for General Surgery.
Introduction
Laparoscopic anti-reflux surgery is an effective treatment for gastro-oesophageal reflux disease (GORD) in those patients who fail or are unable to tolerate medical treatment1,2. Outcomes are similar for different laparoscopic fundoplication techniques3-6 with laparoscopy offering advantages over open surgery with regards reduced length of stay and decreased post-operative pain 7-9. A number of studies have also demonstrated the feasibility of performing anti-reflux surgery as a day case procedure10-15. This is in keeping with the recently published ‘Getting It Right First Time’ (GIRFT) document for General Surgery in the UK16, recommending increased uptake of anti-reflux surgery as a day case procedure. However, a recent review of 12,086 patients undergoing anti-reflux surgery in the UK highlighted a day case rate of only 15.1% 17. Previously published data from our institution demonstrated our initial success in achieving a 70% day case rate, with the most common barriers to discharge including post-operative pain and nausea18. This study was to assess the impact of introducing a new standardised protocol for day case anti reflux surgery and the iterative process to improve day case rates, address barriers to discharge and reduce readmission rates.
Methods
Data were collected prospectively and analysed retrospectively for all consecutive patients undergoing primary laparoscopic anti-reflux surgery (both Nissen and anterior fundoplication) between December 2014 and April 2019. Patients were offered fundoplication according to surgeon expertise and gave fully informed consent. Ethical approval was not required as treatment was decided between surgeon and patient as per routine practice. This retrospective data analysis was not registered as a trial. Data analyses were performed between anterior and Nissen groups using Chi-Squared test (χ2) and Fisher’s exact test when the frequencies were less than 5. All available medical records were used to reduce missing data. Data analyses were performed by one author not responsible for patient selection or inpatient observation.
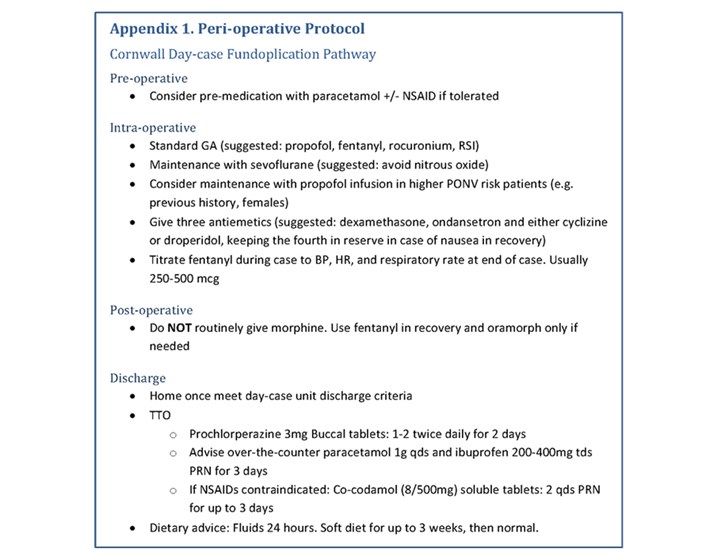
Following literature review, retrospective data analysis and collaborative consultation with the anaesthetists, a standardised peri-operative protocol was developed (Appendix 1).
Eligibility Criteria
Eligibility criteria included those patients deemed suitable for day case surgery, with GORD, American Society of Anesthesiologists (ASA)19 grade of I - III and adequate home support. Patients were not considered eligible if there was no responsible adult at home after surgery for the first 12 hours. Patients were excluded from day case surgery where a hiatus hernia was known to contain more than half of the stomach.
Pre-operative Management
All patients underwent upper gastrointestinal endoscopy pre-operatively. In patients without endoscopic evidence of GORD or HH oesophageal physiology studies including a combination of high resolution manometry, pH and impedance studies were undertaken. Patients were counselled in the outpatient clinic, provided with an information leaflet about day case anti-reflux surgery and scheduled at the start of the operating list, with all surgery performed within a facility able to discharge patients up to 22:00.
Intra-operative Management
Laparoscopic Nissen 360 degree or anterior fundoplication was performed according to surgeon preference, across two sites by five surgeons.
A standardised anaesthesia protocol was used as follows. Pre-medication with paracetamol +/- non-steroidal anti-inflammatory (if tolerated) was considered. A standard general anaesthesia was induced with propofol, fentanyl and rocuronium and maintained with sevoflurane, avoiding nitrous oxide. For those patients with documented higher post-operative nausea and vomiting risk anaesthesia was maintained with propofol. Three antiemetics were used where possible including dexamethasone, ondansetron and either cyclizine or droperidol, keeping the fourth in reserve in case of nausea in recovery. Intra-operative analgesia was fentanyl titrated to blood pressure, pulse, and respiratory rate.
Patients were placed in lithotomy position with table tilted head up. Laparoscopic anterior fundoplication was performed with standardised 4 port and liver retractor technique. A 10mm port placed superior to umbilicus for laparoscope, a 10mm left mid clavicular line sub costal port, left anterior axillary line 5mm port, right mid clavicular line 5mm port and epigastric 5mm port for Nathanson liver retractor (Cook Medical Technology, Bloomington, USA), Hiatal dissection was performed with combination of blunt and sharp dissection with ultrasonic energy device (Lotus, BOWA Medical, UK). The oesophagus was mobilised and encircled with a nylon tape, to allow minimum of 2.5cm of intra-abdominal length and visualisation of both hiatal pillars, preserving the vagus nerve. Posterior crural 2-0 Ethibond sutures (Johnson & Johnson, Belgium) were placed with the use of Teflon pledgets (Johnson & Johnson, Belgium). Tension free anterior 180° partial wrap was performed with 2-0 Ethibond sutures (Johnson & Johnson, Belgium). The right side of the fundus is sutured to the adjacent left side of the oesophagus with two interrupted sutures to accentuate the angle of His. A top suture is placed through the top of the fundus, the oesophagus immediately below the hiatus, and the apex of the hiatus. Next the fundus is sutured to the right lateral wall of the abdominal oesophagus and to the right hiatal pillar using two interrupted sutures.
Nissen fundoplication was performed with identical laparoscopic port positioning, initial dissection and crural repair. The short gastric vessels were not routinely divided. Posterior 360° complete, floppy, fundoplication was performed with 3 or 4 anterior securing 2-0 Ethibond sutures (Johnson & Johnson, Belgium). The cranial suture was gastro-gastric including a bite of anterior oesophageal wall and the inferior sutures gastro-gastric. This allows a 2-3cm floppy fundoplication anchored to oesophagus.
Routine post-operative intravenous morphine was avoided, using fentanyl in recovery and oral morphine only if needed (Appendix 1). 20ml of 0.5% levobupivacaine was infiltrated in the wounds at completion of surgery.
Post-operative Management
When patients satisfied the discharge criteria encompassing pain score, responsiveness, normal observations, and tolerance of liquids they were discharged with prochlorperazine 3mg buccal tablets: 1-2 twice daily for 2 days and advised over the counter soluble analgesia.
A standardised post-operative dietary plan was followed with further information contained in patient information leaflets. This included fluids for 24 hours, soft diet for three weeks then reintroduction of normal diet.
Specialist nurse telephone follow-up occurred on day 1, week 1 and patients had a follow up clinic appointment with the surgeon at 6 weeks to ensure patient safety. Any re-presentations over the 5-year period were recorded and patient notes reviewed for previous procedures.
Results
All data were prospectively maintained in a database. Between 2014 and 2019, 202 consecutive primary laparoscopic fundoplications were performed. The study period captured data over 5 years with patients having planned follow up as outlined previously. 86% (174/202) of patients were successfully discharged from clinic at 6 weeks follow up and were not referred back in the study period.
Primary Anti-reflux Surgery
There was an equal sex distribution and median age 49 years (Range 16.9 to 84.1 years). The median BMI was 29 (Absolute range 17.8 – 39.1 Kg/m2). There were 101 patients classed as ASA class 1(50%), 90 class 2 (44.6%) and 11 class 3 (5.4%). There were 97 Anterior (48.01%) and 105 Nissen (51.98%) fundoplications performed by 5 surgeons. 135 patients (66.8%) underwent oesophageal physiology studies.
The day case rate was 86.6% (155/179) with a 23-hour stay rate of 95.5% (193/202). In 23 patients it was not clearly documented for that episode to be intended as day case. The mean LOS was 0.4 days (median = 0, SD 1.7). Our 2-day readmission rate was 4.95% (n=10) and 30-day readmission 8.4% (n=17), with pain (4.5%, n=9) and dysphagia (3.5%, n=7) the most common reasons for readmission. During the study period, for the four complete calendar years (2015-2018) we demonstrated a statistically significant improvement in our day case rate χ2(n= 174, (p = 0.0036)).
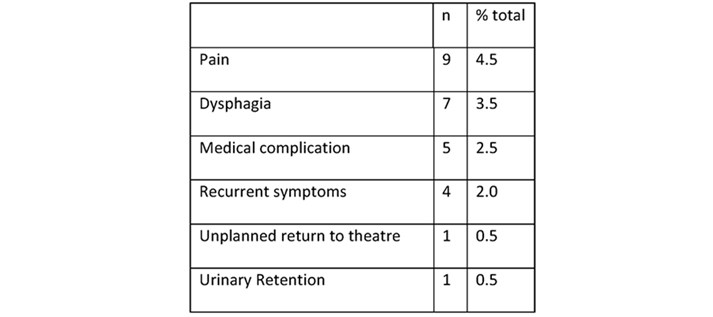
There were 0 conversions to open and 0 mortalities in study period. Two patients had unplanned return to theatre before they met discharge criteria. One for bleeding and one for oesophageal injury requiring transfer to tertiary centre (Table 1). Reasons for delayed discharge included pain (n=2), nausea (n=2) and medical complications (n=2).
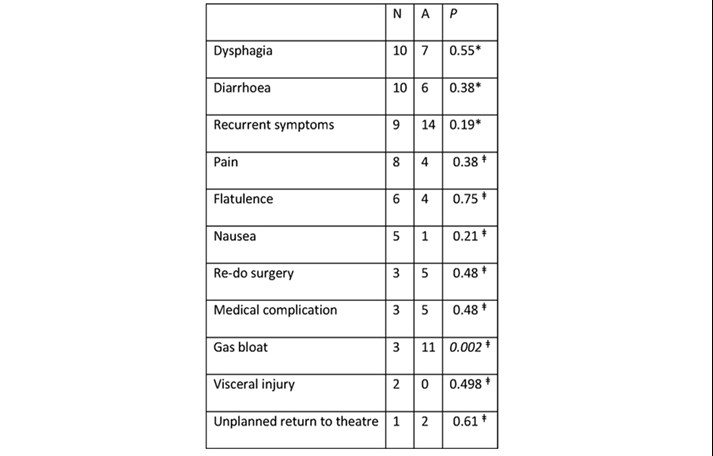
The median follow-up period was 2 years (743 days, min 66, max 1965). 18 patients (8.9%) complained of ongoing dysphagia at clinic review and three had endoscopic dilatation. During the 5-year study period, 24 patients (11.9%) were referred back with recurrent symptoms. The overall revision surgery rate in the study period was 4% (n=8). There were no significant differences in complications between anterior and Nissen fundoplication other than gas bloat (11 (6.9%) vs 3 (2.9%), Fisher’s Exact p=0.002).
Discussion
This study has several limitations. Data regarding patient symptoms were subjective and not measured using validated HRQL questionnaires introducing the possibility of observation bias. Follow-up duration was variable, with those undergoing recent surgery having shorter follow-up. Patients were not randomised introducing the possibility of selection bias. Recurrent symptoms were recorded at clinic review if present or from re-referral in the study period. It is possible that more patients had recurrent symptoms but did not seek medical attention and this was not routinely captured using a validated questionnaire.
Overall, our results indicate the safety and reproducibility of anti-reflux surgery as a day case procedure using a standardised treatment protocol. 86.6% of patients were performed as day case, which is significantly higher than the 15.1% national rate published by Palser et al (2018)17. This also compares favourably to other published series12-15.
In keeping with the experience of1, 12, 13, 17, 20 our operative complication rate was low, but we had a higher than expected rate of early readmissions (Tables 1 & 2). Early readmissions were mainly related to post-operative pain, odynophagia and dysphagia. Our protocol does encourage the use of soluble analgesia at home with a supply of anti-emetic medication to counteract nausea. It is our practice to stop antacid medications on discharge. Despite the early planned telephone follow up and availability of contacting the surgical service out of hours, one third of all readmissions were related to pain (Table 2). The majority of readmissions did not require any intervention other than analgesia at supportive treatment. Early telephone follow up, to maintain patient safety, may lower the threshold at which we review patients in preference to management in the community. Overall, our 30-day readmission rate has improved from 14% in 201618 to 8.4% in 2019.
Table 1.
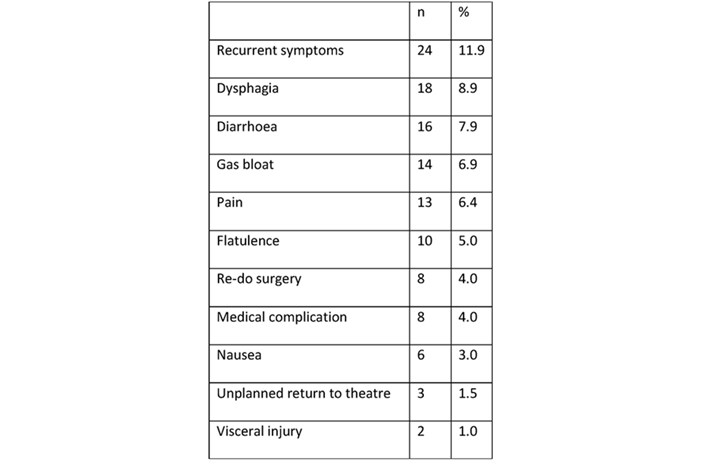
Table 2.
From our discharge data it is possible to see the time of day at which patients were discharged home, with many leaving in the evening. It is important that a day case ward has the staffing and operational hours to facilitate safe discharge up to 220012, 14. Patients undergoing anti reflux surgery can require multiple anti emetics to be able to tolerate oral fluids and time to recover from the process, hence we suggest placing these patients first on the operating list.
Early dysphagia is well recognised complication of treatment for GORD, occurring in a greater proportion of surgically treated than medically managed patients1, but becoming more comparable in the long term1. Overall, our dysphagia rate was 8.9% with three patients requiring endoscopic dilatation (1.5%), comparing favourably to other studies 1, 12, 15.
The long-term efficacy of anti-reflux surgery is well documented 1, 12, 15, 21, 22 but recurrent symptoms and PPI use have been documented in up to 48% of patients6. Review of cases over the study period indicated 11.9% of patients complained of recurrent symptoms and were reinvestigated. 1 patient had early recurrence with incarceration after retching and was re-operated on as an emergency. 7 patients (3.5%) had later revisional surgery. Some authors have reported on revision surgery occurring up to 10 years after first primary surgery22.
In our cohort there was no statistically significant difference in complications between anterior and Nissen fundoplication cases apart from an increase in gas bloat in anterior operations (Table 3). Dysphagia rates were similar between operation types as were readmissions and total complications.
Table 3.
Subsequent to this data set we have continued our protocol and anecdotally continue to have similar results. Despite the potential methodological biases this protocol is likely to have external validity and be reproducible at other centres. Those patients deemed high peri-operative risk by surgeons and anaesthetists may benefit from modified approach and longer period of observation.
Conclusion
Using a standardised peri-operative protocol, patient counselling and early telephone follow up, a day case rate of >80% for laparoscopic anti-reflux surgery is achievable. This is in keeping with the recently published Getting It Right First Time (GIRFT) document for General Surgery.
Conflict of interest statement
There were no funding sources for this study and no conflict of interest declared.
References
- Garg, S.K. and Gurusamy, K.S., 2015. Laparoscopic fundoplication surgery versus medical management for gastro‐oesophageal reflux disease (GORD) in adults. Cochrane Database of Systematic Reviews, (11).
- Galmiche, J.P., Hatlebakk, J., Attwood, S., Ell, C., Fiocca, R., Eklund, S., Långström, G., Lind, T., Lundell, L. and LOTUS Trial Collaborators, 2011. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. Jama, 305(19), pp.1969-1977.
- Watson, D.I., Jamieson, G.G., Pike, G.K., Davies, N., Richardson, M. and Devitt, P.G., 1999. Prospective randomized double‐blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. British journal of surgery, 86(1), pp.123-130.
- Booth, M.I., Stratford, J., Jones, L. and Dehn, T.C.B., 2008. Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro‐oesophageal reflux disease based on preoperative oesophageal manometry. British Journal of Surgery, 95(1), pp.57-63.
- Memon, M.A., Subramanya, M.S., Hossain, M.B., Yunus, R.M., Khan, S. and Memon, B., 2015. Laparoscopic anterior versus posterior fundoplication for gastro-esophageal reflux disease: a meta-analysis and systematic review. World journal of surgery, 39(4), pp.981-996.
- Robertson, A.G., Patel, R.N., Couper, G.W., de Beaux, A.C., Paterson‐Brown, S. and Lamb, P.J., 2017. Long‐term outcomes following laparoscopic anterior and Nissen fundoplication. ANZ journal of surgery, 87(4), pp.300-304.
- Nilsson, G., Larsson, S. and Johnsson, F., 2000. Randomized clinical trial of laparoscopic versus open fundoplication: blind evaluation of recovery and discharge period. British Journal of Surgery, 87(7), pp.873-878
- Ackroyd, R., Watson, D.I., Majeed, A.W., Troy, G., Treacy, P.J. and Stoddard, C.J., 2004. Randomized clinical trial of laparoscopic versus open fundoplication for gastro‐oesophageal reflux disease. British Journal of Surgery, 91(8), pp.975-982
- Bammond, C., 2005. BADS Fellowship report: developing day case Nissen fundoplication. JOURNAL OF ONE DAY SUroeders, J.A., Rijnhart-de Jong, H.G., Draaisma, W.A., Bredenoord, A.J., Smout, A.J. and Gooszen, H.G., 2009. Ten-year outcome of laparoscopic and conventional nissen fundoplication: randomized clinical trial. Annals of surgery, 250(5), pp.698-706
- Salminen, P., Hurme, S. and Ovaska, J., 2012. Fifteen-year outcome of laparoscopic and open Nissen fundoplication: a randomized clinical trial. The Annals of thoracic surgery, 93(1), pp.228-233.
- HRGERY, 15(4), p.89.
- Jensen, C.D., Gilliam, A.D., Horgan, L.F., Bawa, S. and Attwood, S.E., 2009. Day-case laparoscopic Nissen fundoplication. Surgical endoscopy, 23(8), pp.1745-1749
- Khan, S.A. and Stephens, L., 2012. Day-case laparoscopic Nissen fundoplication. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 16(1), p.50.
- Brown, J.J., Bawa, S., Horgan, L.F. and Attwood, S.E., 2013. Achieving day-case laparoscopic nissen fundoplication: an analysis of patient and operative factors. Journal of Laparoendoscopic & Advanced Surgical Techniques, 23(9), pp.751-755
- Mistry, P., Zaman, S., Shapey, I., Daskalakis, M., Nijjar, R., Richardson, M., Super, P. and Singhal, R., 2018. Building a model for day case hiatal surgery-Lessons learnt over a 10 year period in a high volume unit: A case series. International Journal of Surgery, 54, pp.82-85.
- https://gettingitrightfirsttime.co.uk/wp-content/uploads/2018/08/GIRFT-GeneralSurgery-Aug17-O1.pdf. NHS Improvement. Accessed 12.8.19
- Palser, T.R., Ceney, A., Navarro, A., Swift, S., Bowrey, D.J. and Beckingham, I.J., 2018. Variation in laparoscopic anti-reflux surgery across England: a 5-year review. Surgical endoscopy, pp.1-7.
- Javed, O., Maitland, L., Peyser, P., Finlay, I. and Clarke, M., 2017, September. Day-case laparoscopic anti-reflux surgery: experience in Cornwall. In BRITISH JOURNAL OF SURGERY(Vol. 104, pp. 18-18). 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY
- https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. American Society of Anesthesiologists. Accessed 4.5.20
- Barthelsson, C., Lützén, K., Anderberg, B., Bringman, S. and Nordström, G., 2003. Patients’ experiences of laparoscopic fundoplication in day surgery. Ambulatory Surgery, 10(2), pp.101-107
- Galmiche, J.P., Hatlebakk, J., Attwood, S., Ell, C., Fiocca, R., Eklund, S., Långström, G., Lind, T., Lundell, L. and LOTUS Trial Collaborators, 2011. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. Jama, 305(19), pp.1969-1977
- Castelijns, P.S.S., Ponten, J.E.H., Vd Poll, M.C.G., Bouvy, N.D. and Smulders, J.F., 2018. Quality of life after Nissen fundoplication in patients with gastroesophageal reflux disease: Comparison between long-and short-term follow-up. Journal of minimal access surgery, 14(3), p.213.
Appendix
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40118/303-achieving-success-in-day-case-laparoscopic-anti-reflux-surgery-using-a-standardised-peri-operative-protocol-in-a-cornish-cohort.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse7
Sian Davies, Ghaleb Goussous, Amaar Aamery, Aliyah Choudray & Mangta Manu
Royal Wolverhampton NHS Trust
Conflicts of Interest Statement
We can confirm that we have no conflicts of interest to disclose.
Abstract
Background: An important risk factor for gallstone disease is obesity which poses a significant problem for surgical management. The aim of our study was to show that laparoscopic cholecystectomy is still safe to be performed as a day case or short stay procedure (<24hrs) in the obese and morbidly obese patient in a non-bariatric center.
Method: A retrospective observational study analysing all patients who underwent laparoscopic cholecystectomy at Royal Wolverhampton Hospital between January 2013 and January 2017 was performed. Patients were identified using RWH HES data and Length of stay, operative duration, and readmission rates were compared for BMI categories. Statistical analysis was performed by Chi-square test and one-way Anova test as appropriate. A p-value of <0.05 was considered significant.
Results: We identified 1055 cases. Male to female ratio was approximately 1:3. There was no significant difference between the primary outcomes of length of stay, Number performed as day case, operative duration and 30-day readmission rates between all BMI groups. In all groups the number of cases being performed as day case with same day discharge was 70-78% with no significant difference between the groups. The mean operative duration for the highest BMI group (BMI>41) of 59.78 mins compared to the lower BMI groups (BMI 26-30) of 55.25 mins this was not significantly different. 30-day readmission rates for all BMI groups were comparable (P = 0.61).
Conclusion: Our results highlight that obese (BMI 35-39) and morbidly obese (BMI >40) patients can have a laparoscopic cholecystectomy performed safely in a non-bariatric center and as day case/short stay procedure (discharge within <24hrs) with no significant increase to operative duration, LOS or 30-day readmissions rates.
Introduction
Laparoscopic cholecystectomy is one of the most common elective operations in the UK with over 60,000 cases performed each year (1). It is associated with a very low morbidity and mortality and often performed as a day case procedure in most centres with a very low risk of conversion to an open procedure. The main indication for performing this procedure is cholelithiasis which has a UK population incidence of 10-15%. An important risk factor for gallstone disease is obesity (2) and with an obesity crisis in the UK this presents a significant problem for surgical management. Currently 1 in 4 people in the UK are obese (BMI >30 (28.1%)) with 1 in 10 being morbidly obese (BMI>40 (2.9%)) (3). These are set to rise over the next 10 years and its predicted that more than a 3rd of the UK population will be obese by 2020 (4).
Obese and morbidly obese patients post a significant challenge both anesthetically (5) and surgically with some studies suggesting increased operative times and increased LOS, and previously there has been a hesitancy to offer these patients a laparoscopic cholecystectomy in a non-bariatric center (6). However increasing evidence has shown that laparoscopic cholecystectomy is safe even in the morbidly obese patient and have also suggested that they can also be performed as a day case safely (7) (8) (9). The aim of our study was to show that laparoscopic cholecystectomy is still safe to be performed as a day case or short stay procedure (<24hrs) in the obese and morbidly obese patient in a non-bariatric center.
Methods
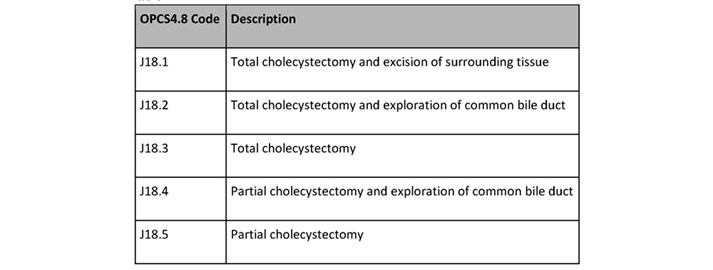
A retrospective observational study was performed analyzing all patients who underwent laparoscopic cholecystectomy at Royal Wolverhampton Hospital between January 2013 and January 2017. Patients were identified using the Royal Wolverhampton Hospital HES (Hospital episode Statistics) data coded for elective laparoscopic cholecystectomy using the OPCS4.8 codes for cholecystectomy (table 1)
Table 1.
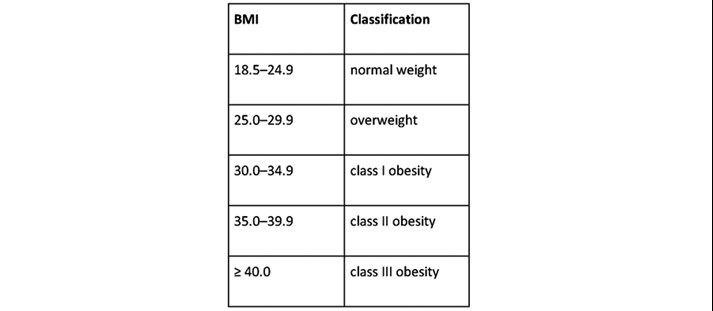
Patients were divided into individual BMI groups based on WHO anthropometry guidance on obesity classification (Table 2).
Table 2.
Primary outcomes include length of stay and operative duration were compared for BMI categories. Secondary outcomes were post-operative morbidity rates, conversion to an open procedure and readmission rates. Post-operative 30-day morbidity was classified using the Clavien-Dindo classification. Patients with a prolonged LOS (>24hrs) had their notes and discharge letters assessed and complications classified.
Exclusion criteria included those admitted as emergencies and non-standard laparoscopic cholecystectomy (single incision laparoscopic surgery, and those patients who had previous surgery and an adaptive approach was used). Statistical analysis was performed using GraphPad Prism software V7 (GraphPad Software Inc). Statistical analysis was performed by Chi-square test and one-way Anova test as appropriate. A p-value of <0.05 was considered significant.
Results
A total of 1055 cases were identified that met our inclusion and exclusion criteria. Male to female ratio was approximately 1:3 (803 females, 252 males). In the higher BMI groups, there was a significantly higher ratio of females of males (p= <0.0001) and the higher BMI groups were generally younger patients as demonstrated in table 1.
Operative and Post-operative results are shown in Table 2. There was no significant difference between the primary outcomes of length of stay (LOS), Number performed as day case, operative duration and 30-day readmission rates between all BMI groups. In all groups the number of cases being performed as day case with same day discharge was 70-78% with no significant difference between the groups. The mean operative duration for the highest BMI group (BMI>41) of 59.78 mins compared to the lower BMI groups (BMI 26-30) of 55.25 mins this was not significantly different.
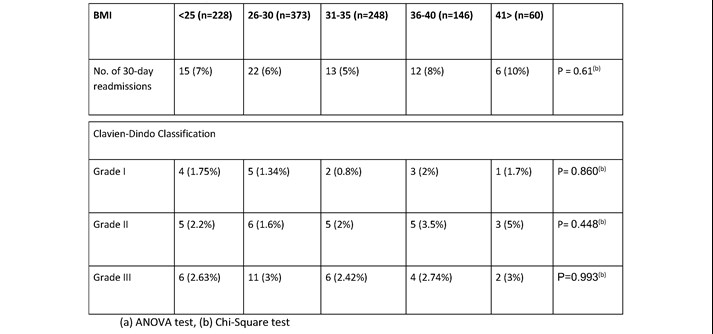
When analysis was performed looking at the reasons for prolonged stay (>24hrs) using the Clavian-Dindo classification there was no significant difference in complications. The most common reason for prolonged stay was post-operative pain (1.9%), and urinary retention (0.6%). Other more clinically significant complications included post-operative bleeding (1.3%) and bile duct injury (table 3). 30-day readmission rates for all BMI groups were comparable (P = 0.61). On specific analysis of the reasons for readmission these were again also comparable across the groups with the majority of readmissions for wound infections (1.2%) and missed or retained stones (0.8%) (table 4).
Table 1. Patient Demographics for BMI categories.
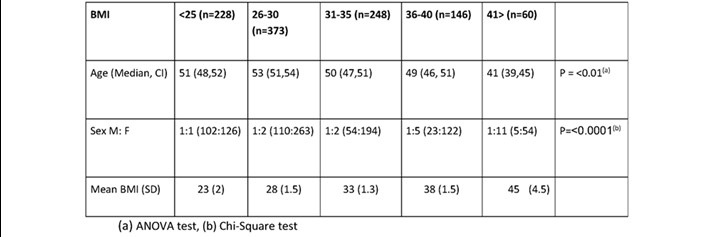
(a) ANOVA test, (b) Chi-Square test
Table 2. Operative and Post-operative results for BMI categories.
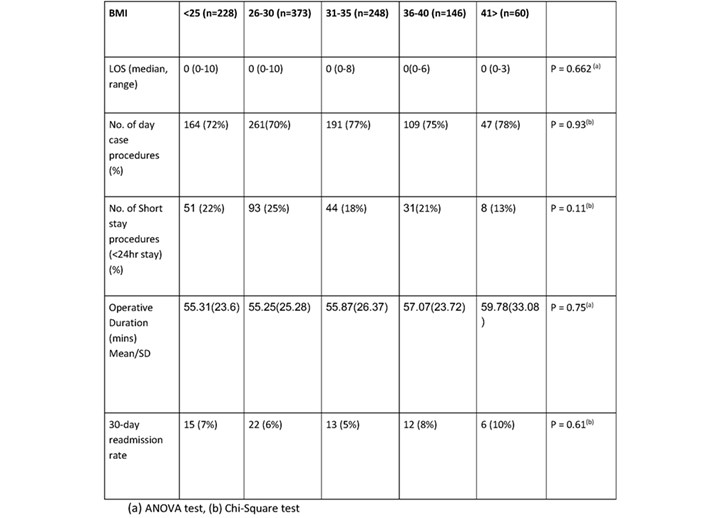
Table 3. Post-operative complications resulting in length of stay >24hrs.
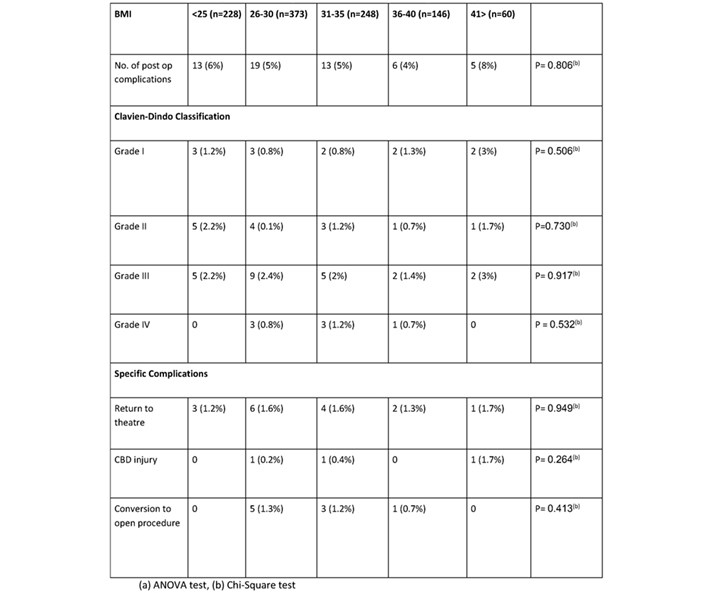
Table 4. 30-day Readmission related to operative complications.
Discussion
Increasing evidence has shown that laparoscopic cholecystectomy is safe in the obese patient and our large cohort study builds on this data by showing no significant difference in length of stay, 30 day rea30-dayon rates, post-operative complications or operative duration between BMI groups for patients undergoing laparoscopic cholecystectomy in a no bariatric center. We have also shown that these potentially higher risk groups of patients can still have their procedures performed as day case without any serious risk of complication which is highlighted by the lack of difference in 30-day readmission rates. The fears of operating on the group maybe allayed when data from study shows that the higher BMI group tend to be a younger cohort of patients (median 41 (Class III obesity), median age 51 (normal weight)) and higher female prevalence, in whom fat distribution tends to be subcutaneous rather than internally (9). There was a small difference in operative duration between the normal weight patients and the class III obese patients (mean = 55.31 vs. mean = 59.78, p=0.75) this was not significant. There is an appreciation that this increase can be accumulative during a list, but overall difference would still be marginal, and this could be taken into account during list design. There was also no difference in the rate of conversion to an open procedure between the BMI groups.
With higher national tariff payments for day case procedures and no significant increase risk of post-operative complications, or 30-day readmission rates, these higher BMI groups should still be considered for day case management wherever possible even in a non-bariatric centre. Not offering these higher group patients a cholecystectomy put this group at a higher risk of the complications of gallstones disease particularly in gallstones pancreatitis. Studies have shown that obese patients are at higher risk of necrosis and complications of pancreatitis and is proportional to their BMI (10) (11) (12).
Operating on the obese and morbidly obese patient is a growing issue globally and our practice needs to adapt to account for this. Our study has shown that it is safe to offer a laparoscopic cholecystectomy to the obese (class I to III) patient as a day case in a non-bariatric centre and BMI should not be a limiting factor. We recognize limitations of this study include a retrospective methodology using HES Data which relies on accurate data entry and coding which in recent years has improved. Also, we did not include seniority of surgeon which may be a confounding factor in shorter operative duration, and this could be an area for future research.
References
- NICE and RCS of England. [Online] Dec 2016. Commissioning guide: Gallstone disease. https://www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=10&ved= 2ahUKEwi0nJyQwe3hAhWXRxUIHeHFB9oQFjAJegQIAhAC&url=https%3A%2F%2Fwww.rcseng.ac.uk%2F-%2Fmedia%2Ffiles.
- Epidemiology of gallbladder disease: cholelithiasis and cancer. Stinton LM, Shaffer EA. 2, 2012, Gut Liver, Vol. 6, pp. 172-187.
- Baker, Carl. Obesity Statistics. s.l. : House of Commons Library, 2018.
- Morbid obesity in the UK: A modelling projection study to 2035. Keaver L, Xu B, Jaccard A, Webber L. 2018, Scand J Public Health.
- Anaesthesia and morbid obesity. Sharmeen Lotia, Mark C. Bellamy,. 5, 2008, Continuing Education in Anaesthesia Critical Care & Pain, Vol. 8, pp. 151-156.
- Laparoscopic cholecystectomy in morbidly obese patients. Ammori BJ1, Vezakis A, Davides D, Martin IG, Larvin M, McMahon MJ. 11, 2001, Surg Endosc, Vol. 15, pp. 1336-9.
- Obesity: an indication rather than contraindication to laparoscopic cholecystectomy. Unger WS, Unger MH, Edelman SD et al. 1992, Obes Surg, Vol. 2, pp. 29-31.
- Day case laparoscopic cholecystectomy in patients with high BMI: Experience from a UK centre. A Tandon, G Sunderland, QM Nunes, N Misra1, M Shrotri. 2016, Ann R Coll Surg Engl, Vol. 98, pp. 329–333.
- Sex differences in human adipose tissues - the biology of pear shape. Karastergiou K, Smith SR, Greenberg AS, Fried SK. 1, s.l. : Biol Sex Differ, 2012, Vol. 3, p. 13.
- Obesity and pancreatitis. Khatua B, El-Kurdi B, Singh VP. 5, s.l. : Curr Opin Gastroenterol, 2017, Vol. 33, pp. 374-382.
- Obesity-Related Effects on Pancreatic Disease . Zyromski, Nicholas J. s.l. : Pancreapedia: Exocrine Pancreas Knowledge Base, 2015.
- Combination of APACHE-II score and an obesity score (APACHE-O) for the prediction of severe acute pancreatitis. Johnson CD1, Toh SK, Campbell MJ. 1, s.l. : Pancreatology, 2004, Vol. 4, pp. 1-6.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42062/303-the-increasing-challenge-of-managing-morbidly-obese-patients-with-gallstone-disease-in-a-non-bariatric-centre.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse8
Razi, Kasra ST5 General Surgery KSS Deanery, East Sussex Healthcare NHS Trust
Cullen, Jack F2 East Sussex Healthcare NHS Trust
Arbis, Alex F1 East Sussex Healthcare NHS Trust
Shah, Elizabeth Breast Consultant, Conquest Hospital, East Sussex Healthcare NHS Trust
Corresponding author: Kasra Razi, 79 Redington Road, London NW3 7RR
Abstract
Aim: The use of drains in breast surgery is decreasing, and various methods of reducing the dead space after mastectomy have been described such as quilting of skin flaps and the use of adhesive tissue glues. The British Association of Day Surgery (BADS) outlines a 30% day-case target for simple mastectomy procedures. We conducted a feasibility study using a fibrin sealant spray (ARTISS) instead of drains in mastectomy without reconstruction, to reduce patient length of stay (LOS) & post-operative complications.
Method: A consecutive series of 50 patients, irrespective of age, BMI, social demographics & co-morbidities were included in the study. All surgical and theatre staff had appropriate training and data including day-case rates, seromas requiring aspiration and post-operative complications were prospectively collected.
Results: The mean age was 65 years; average BMI was 29.4kg/m2 and the average mastectomy weight was 712.4g. A day-case rate of 52% (26/50) was achieved. Of the day-case patients, 7 developed seromas requiring aspiration and one was re-admitted 7 days later with a haematoma. The overall seroma rate was 28% (14/50).
Conclusions: This study demonstrates that drain-free mastectomy is possible using ARTISS. The use of this product facilitates early discharge in all demographic groups and adherence to the national standard is achieved.
Introduction
Women undergoing a mastectomy for breast cancer have traditionally stayed overnight in hospital. Day-case surgery over the last decade has experienced an increase in practice with better outcomes for patients and improved cost-effectiveness for the NHS. The British Association of Day Surgery (BADS) advocates a 30% day-case target for simple mastectomy procedures (1), however overnight stay is still common practice. In our unit (East Sussex Foundation Trust) there has been a problem with establishing a day-case mastectomy programme for various reasons: our geographical location in the South East of England is home to one of the highest over 65’s population in the UK (2). An elderly patient demographic with multiple social issues can pose difficulties in initiating a day-case programme and the perceived complications associated with discharge to the community with drains in situ can increase hospital stay further. Our second stumbling block was a lack of nursing resource for drain removal. Nurses at our hospital did not have the physical space or time to remove drains in patients discharged home with drains in-situ, either in the community setting or as return ward attenders. The third hurdle was the mindset of patients and nursing staff towards early discharge of mastectomy patients for emotional and psychological reasons. Our patients had no confidence going home with their drain, as they were concerned about the drain-related pain. They were anxious about the drain not working or a complication forming or having a drain in-situ with children and family being around.
Seroma formation is the most common sequelae of breast surgery, with rates ranging between 15 to 81% of patients being affected (3). Seroma is the accumulation of clear serous fluid containing blood plasma and inflammatory fluid following surgery, however the pathogenesis and ways in which to reduce its formation are still poorly understood (4). The complications associated with seromas include infection, delayed wound healing, patient discomfort and skin flap necrosis, all of which can increase the likelihood of needing fluid aspiration of the seroma. Obliteration of the dead space between the wound surfaces following mastectomy appears to be fundamentally important in reducing seroma formation. Several methods have been proposed to prevent this; quilting of skin flaps, closed suction drainage and the application of adhesive tissue glues have all been described, however there is still no clear superior method (5).
The fibrin sealant spray Artiss® (Baxter, UK) is composed of a sealer protein solution with both human fibrinogen and human thrombin solutions. This allows for an extended polymerization time and full skin flap adherence to the wound bed. It is designed to reduce the formation of post-operative seroma and haematoma, thereby enabling a drain-less procedure (6). The literature evaluating the use of Artiss® in mastectomy is limited, however a series of studies have indicated a clear relationship between the use of Artiss® and the reduction of post-operative seroma (7,8). A recent study demonstrated a decrease in patient length of stay post procedure however the complication rate remained unchanged (9).
The purpose of this study was to analyse the efficacy of low-thrombin fibrin sealant (Artiss®) to reduce the length of hospital stay post mastectomy, and to additionally decrease the rate of seroma and haematoma formation.
Methods
Study Design
We designed a single centred unblinded prospective observational study looking at the effect of Artiss® on increasing day-case mastectomy rates. The trial was conducted between April 2018 and July 2019. All patients who required a simple mastectomy were given the option of using Artiss® instead of having the conventional Redivac drain. All patients who fitted the criteria of requiring a simple mastectomy regardless of breast size, body mass index (BMI) and co-morbidities were eligible. The primary aim was to increase the number of day-case mastectomies and reduce the hospital length of stay for all patients undergoing a simple mastectomy. The secondary aims were to reduce seroma and haematoma formation rates.
Prior to commencing the study all staff who made up the breast team including theatre nurses and breast care nurses were trained by a Baxter pharmaceutical company representative. A standardized protocol was used for the application of Artiss® in all patients. Only those trained in applying the product were able to use the sealant on a patient. (Protocol Inserted here)
Artiss® is a fibrosealant spray which has dual property which allows for tissue adherence and haemostasis. It is made up of two human plasma derived components. A sealer protein solution containing human fibrinogen and a synthetic fibrinolysis inhibitor that helps delay the premature breakdown of the clot at the site of application. A low-concentration human thrombin solution in a calcium chloride solution, which allows an extended polymerization time of 60 seconds compared to other fibrin sealants that can contain 500 IU/mL or more of thrombin. Each mastectomy flapped received 4mls of Artiss® spread evenly across the fascia covering pectoralis major. The mastectomy flap was then positioned neatly down on to the chest wall with 3 minutes of equal compression using a damp gauze. The skin edges were stitched using 3-0 vicryl and monocryl for the skin. All patients that had axillary lymph node dissection (ALND) had a size 10 Redivac drain placed in the axilla which was removed either when less than 50 ml output per 24 hours or after 5 days at the latest.
Postoperative Care
Patients were reviewed post surgery at the end of the day and assessed by the consultant before being discharged home. All patients were followed up in clinic two weeks after their operation by the consultant. At any time if patients felt that they may have developed a seroma or haematoma after they had been discharged they were seen by the breast enhanced recovery nurse and the breast consultant. If patients were symptomatic with either of these they were drained in clinic under an aseptic technique and the aspirated fluid was measured via the syringe. All measurements were recorded by the enhanced recovery after surgery (ERAS) nurse who was trained in aspirating mastectomy seromas.
Results
50 consecutive patients enrolled into this study. The mean (range) age of the patients was 65 (40-88) years with a mean (range) BMI of 29 (19-42) kg/m2. The average breast weighed 712g (143g to 2412g). 28 (56%) patients has invasive ductal carcinoma (IDC), 13 (26%) had invasive lobular carcinoma, 3 had ductal carcinoma in situ (DCIS), 1 lobular carcinoma in-situ (LCIS), 3 had risk reducing mastectomy and the remaining two had one had tubular carcinoma and the other papillary carcinoma. 25 patients (50%) had simple mastectomy with sentinel lymph node biopsy, 12 patients (24%) had simple mastectomy with ALND. All of those with ALND had a Redivac drain placed in the axilla which was removed when drain output was less than 50mls over 24 hours or at the very latest day 5 post operation. 26 patients (52%) went home the same day. 7 of those developed seromas (14%), 1 patient had their seroma drained twice. 21 out of the 24 patients (48%) who stayed longer stayed an extra day and 1 patient stayed 4 days. Of those who stayed longer, the majority of patients 15/24 (62.5%) stayed in longer due to patient choice, of those nearly half of them had a drain in their axilla. Other reasons for staying in longer included post-operative nausea and vomiting, blue dye reaction and cardiac complications. Overall, our hospital LOS for a simple mastectomy patients was reduced to a day-case procedure, previously 23-hour stay. On average the hospital LOS has reduced to half a day, prior to using Artiss® the average LOS was 1.5 days. Our day-case mastectomy rate has gone from 0% to nearly 50%. In total, 14 patients (28%) developed seromas requiring needle aspiration. 1 patient out of the fifty patients (2%) developed a haematoma which required evacuation in theatre. Our seroma rates have fallen from 40% previously audited by the department to 28%. It is too early to say whether Artiss® can reduce haematoma rate but the results so far as very promising.
Table 1 Demographic factors and clinical characteristics of all patients.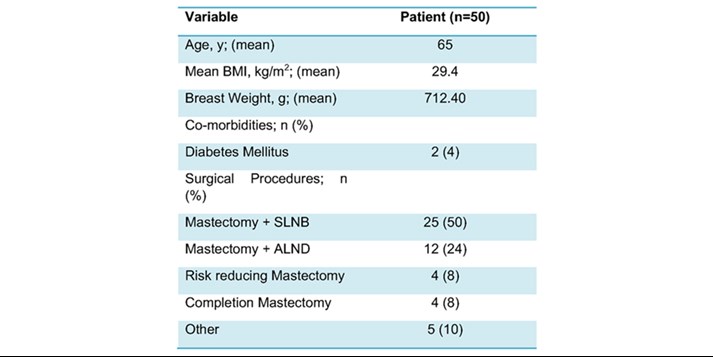
Discussion
Day-case rate
Our results have clearly demonstrated that Artiss® can help reduce hospital length of stay in patients who have a mastectomy. We have also managed to increase our day-case simple mastectomy rates from 0% to over 50%. By replacing the Redivac drain with Artiss® we have eliminated one of the main factors for delayed discharge. Having a drain in-situ and discharging patients with it can be anxiety inducing and often patients are reluctant to go home with a drain making it difficult for our unit to perform day-case mastectomies. The patient demographic in East Sussex varies compared to other parts of the country; the patients are generally older and for social reasons, some are simply unable to go home on the same day of procedure (1). Added to that the limited outpatient support for breast patients due to lack of resources makes it difficult for the clinicians to discharge the patient home safely with drains. Within the first year, our unit surpassed the 30% day case target from the British Association of Day Surgery (1). The introduction of this technique enabled a day-case mastectomy programme in our unit, which had previously faced challenges to achieving this. The cooperation between different members of the patient care pathway including surgeons, specialist breast nurses and enhanced recovery nurses supported the implementation of this change in practice.
Seroma and Haematoma Rate
Drains also pose other problems such as introducing infections into the wound, becoming blocked allowing for haematomas to form and cause patient discomfort. Other techniques have been used to mimic the effects of the drain without needing to worry about the issues that come with them such as quilting but with the properties of Artiss® we thought we could tackle other issues associated with mastectomies such as seroma and haematoma formation. The haemostatic properties of Artiss® speed up the process of coagulation, which reduce the likelihood of haematoma formation. The human fibrinogen component can enable lymphatic vessel closure, hence reducing postoperative dead space and seroma formation through tissue adhesion (4). Although we only had one haematoma however with the small number of patients, we have it is too early to say whether Artiss® has led to any improvement.
Thirteen patients had drains placed in their axilla following ALND. Only two of these patients went home the same day and on average stayed one day longer than those without. It was the patient’s choice to stay in a day longer, none of these patients felt comfortable going home with a drain. This clearly demonstrates the hindrance drains have on performing day-case mastectomy. Seroma formation is a common complication of breast mastectomies. The current literature quotes incidence of up to 90%. Various studies which have investigated this have identified that seroma incidence rates can be reduced by flap fixation (Kuroi K et al).
Before introducing Artiss® the department seroma rates were around 40% this has now reduced to 26%. When analyzing the data on those who developed seromas there is no clear reason for this; they were not necessarily older or bigger breasted. The mean (range) weight of those who developed seromas was 636.7mg (385-866mg) below that of the cohort average. Of those that developed seromas and went home the same day 5 had simple mastectomy and SLNB the others had ALND instead. The mean BMI was also 27.2 kg/m2 in seroma cohort, 2 units below the entire group mean BMI.
The aspiration of seromas from the surgical wound is a significant cause of patient discomfort, can delay further treatment, increase the rate of wound infections and lead to repeated outpatient visits (3). The importance of reducing seroma formation is clinically relevant for our cohort of patients – the introduction of Artiss® has slightly reduced the frequency of seromas however their incidence remains significant.
Remission Rates
We had a 0% remission from our cohort of patients.
Limitations
The main limitation of this study is that it is a prospective observational study with no control group. No statistical analysis of the data has been performed and the lack of a control group and group randomisation would question the validity of the results. The trial is also at risk of the Hawthorne effect since both the clinician and patient were aware that they were receiving a new treatment to increase day case mastectomy rates. Behaviours and decisions from both patient and clinician may be influenced therefore questioning the validity of the results of this study. To improve our study and assess the validity of the result further trial in the form of randomised control trials (RCTs) are needed.
Conclusion
It is feasible to use Artiss® instead of drains to allow earlier discharge of patients and make day-case mastectomy a reality. The product can also helped reduce both the number and the size of the seroma in mastectomy patients by obliterating the dead space. To develop this project further a trial looking at cost-analysis and patient satisfaction is required to help us decide whether there is any place for drains in patients with a simple mastectomy.
References
- Skues M. BADS directory of procedures (4th edn). London: British Association of Day Surgery; 2012.
- Office for National Statistics (ONS) 2017: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/july2017
- Pogson CJ, et al. Seroma following breast cancer surgery. Eur J Surg Oncol. 2003; 29:711–717. doi: 10.1016/S0748-7983(03)00096-9.
- R. Benevento, A. Santoriello, G. Pellino, G. Sciaudone, G. Candilio, G.S. De Fatico, F. Selvaggi, E. Colo, S. Canonico. The effects of low-thrombin fibrin sealant on wound serous drainage, seroma formation and length of postoperative stay in patients undergoing axillary node dissection for breast cancer. A randomized controlled trial. Int. J. Surg., 12 (2014), pp. 1210-1215
- van Bastelaar, J., Beckers, A., Snoeijs, M. et al.Flap fixation reduces seroma in patients undergoing mastectomy: a significant implication for clinical practice. World J Surg Onc14, 66 (2016) doi:10.1186/s12957-016-0830-8
- van Bastelaar, J., Theunissen, L.L.B., Snoeijs, M.G.J., Beets, G.L. & Vissers, Y.L.J. 2017, Flap Fixation Using Tissue Glue or Sutures Appears to Reduce Seroma Aspiration After Mastectomy for Breast Cancer.
- Sakkary MA. The value of mastectomy flap fixation in reducing fluid drainage and seroma formation in breast cancer patients. World J Surg Oncol. 2012;10.
- Ten Wolde B, Van Den Wildenberg F, Keemers‐Gels ME, Polat F, Strobbe L. Quilting prevents seroma formation following breast cancer surgery: closing the dead space by quilting prevents seroma following axillary lymph node dissection and mastectomy. Ann Surg Oncol. 2014; 21:802‐807.
- Harrison C, Remoundos DD, Harvey KL, Stoker GV, MacLean G, Adwani A et al (2019) Increasing the incidence of drain-free day-case mastectomies with the use of a fibrin tissue sealant; data from a single surgical center in the United Kingdom. Breast J 25(6):1090–1096
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42064/razi_-day-case-mastectomy.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse9
Harmeet Khaira & Julian Hull
(This article was originally published in the Journal of One-Day Surgery Vol. 23 No. 3, 2013. It was Number 6 in the 'How i Do It' series, updated in 2020)
Patient Selection
- Standard day case criteria
Anaesthetic Techniques
- General anaesthesia:
TIVA (Total IntraVenous Anaesthesia) comprising propofol and remifentanil as target controlled infusions.
Intubation or Laryngeal Mask and IPPV ventilation. Air/O2 only.
Short duration muscle relaxants as these operations can take less than 20 minutes.
Routine iv fluids (minimum 1000ml Hartmann’s).
Routine anti-emesis (iv ondansetron 4mg and iv dexamethasone 4mg) as lap. Cholecystectomy has a high incidence of post-operative nausea and vomiting (PONV).
Surgical Technique
- Standard positioning of patient with slight head-up tilt and table rotation towards surgeon. Use intermittent pneumatic compression for DVT prophylaxis.
- Local anaesthetic infiltration to all port sites before insertion of ports (20ml 0.25% chirocaine).
- Use of three 5mm ports and one 10mm port.
- Low pressure CO2 insufflation (10mmHg)
- Meticulous washout at end of procedure.
- Instillation of 500ml warm saline containing 20ml 0.25% chirocaine around liver and gallbladder bed.
- No drains.
Peri-operative Analgesia
- Peri-operative analgesia utilising a multi-facetted approach with NSAID, paracetamol, iv fentanyl (250-300mcg), local anaesthetic to wound sites and local anaesthetic wash to gall bladder bed
- Post-operative analgesia:
Analgesia requirements vary hugely between patients. Group directive allows recovery staff to titrate iv fentanyl or oral morphine for rapid relief of post-operative prior to return to DCU ward.
Regular paracetamol and ibuprofen.
Take Home Medication
- Regular oral paracetamol 1g qds and ibuprofen 600mg qds.
Organisational issues
- Ensure admission to day-case ward only.
- Early introduction of fluids, diet and mobilization.
- Allow home even if not passed urine
Common Pitfalls
- Care should be taken not to inflate stomach prior to intubation.
Pain and PONV need to be treated aggressively
Anticipated day case rates
- 90%
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40115/hidi-kaira_lapchole-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse11
Nuala Campbell & Jonathan Hindley
(This article was originally published in the Journal of One-Day Surgery Vol. 23 No. 1, 2013. It was Number 2 in the 'How i Do It' series, updated in 2020)
Patient Selection
-
Any woman listed for laparoscopic hysterectomy who fulfills DSU criteria and desires day surgery pathway – patient led
-
We have tended to avoid women with chronic pain either incidental to or being treated with hysterectomy as we feel that their postoperative pain management is more complex. This is a pragmatic rather than evidence based criterion and is flexible on discussion with patient.
-
We have avoided women with large (greater than 14 week equivalent) uteri or other pathology that we feel increase the likelihood of conversion to laparotomy
Anaesthetic Techniques
- Induction and maintenance with target controlled propofol and remifentanyl infusions.
- Intubation and controlled ventilation using Pressure Controlled Ventilation- Volume Guaranteed and 5 mmHg of PEEP – this procedure requires very steep trendelenberg, and this mode keeps barotrauma to a minimum whilst reducing atelectasis.
- Large suction beanbag behind shoulders to prevent patient slipping when tipped.
- Minimum 3 metre infusion line for TIVA and a tap and extension on the fluid line: arms are tucked to the side and inaccessible during the case.
- Always give 1 litre crystalloid as this reduces PONV and dizziness: usually do not need more than this.
- IV Dexamethasone 4mg, cyclizine 50mg. Give the cyclizine just before pneumoperitoneum as the tachycardia side effect is useful at this stage!
- Subcutaneous fragmin 5000u at end of procedure
Surgical Technique
- Standard Total Laparoscopic Hysterectomy with or without removal of ovaries
- Verres entry with high CO2 pressures then operating at 12 to 15mmHg. Three or four port laparoscopy
- RUMI manipulator with balloon colpo-pneumo-occluder and KOH cups to manipulate uterus and maintain pnuemoperitoneum (Have previously used McCartney tubes)
- Pedicles secured with bipolar diathermy throughout (reusable instruments)
- Vault sutured laparoscopically – needle introduced through 11mm port
Peri-operative Analgesia
- Pre medication with oral Ibuprofen Retard 1600mg and Paracetamol 1G
- Intra operative: IV fentanyl 2 mcg/kg.
- Post operative IV fentanyl, then oramorph and regular paracetamol.
Take Home Medication
- Paracetamol 500 mg/ codeine 30mg po qds, laxido 1 sachet bd, plus ibuprofen 400 mg po qds
- Organisational issues
- Pre operative brief to include PACU staff member as anticipation of individual patient issues hugely valuable in this patient group
- Day Surgical Unit theatre team experienced in major gynaecological laparoscopic cases with skills that enable conversion to open procedures – staff rotate to main theatres if unfamiliar with open cases.
- Urinary catheter throughout procedure but removed in theatre prior to reversal of anaesthesia
Organisational issues
- Pre operative brief to include PACU staff member as anticipation of individual patient issues hugely valuable in this patient group
- Day Surgical Unit theatre team experienced in major gynaecological laparoscopic cases with skills that enable conversion to open procedures – staff rotate to main theatres if unfamiliar with open cases.
- Urinary catheter throughout procedure but removed in theatre prior to reversal of anaesthesia
Common Pitfalls
- Fluid redistribution from positioning: warn patient beforehand of periorbital/facial swelling
Anticipated day case rates
- 75%
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse12
Ian Smith, Anurag Golash & Clare Hammond
(This article was originally published in the Journal of One-Day Surgery Vol. 23 No. 1, 2013. It was Number 1 in the 'How i Do It' series, updated in 2020)
Patient Selection
- Non-functioning kidney or renal cell carcinoma
- T1 tumour <7 cm
- Typical day surgery criteria, of which a well motivated patient is by far the most important
Anaesthetic Techniques
- We use a standardised protocol which is similar to that used for laparoscopic cholecystectomy
- Induction with fentanyl and propofol. Tracheal intubation and controlled ventilation breathing sevoflurane in air-oxygen
- Long acting intraoperative opioids are avoided
- Multimodal antiemesis with dexamethasone and ondansetron
- Intravenous hydration with 1 or (maximum) of 2 litres Hartmann’s solution
Surgical Technique
- Standardised transperitoneal laparoscopic approach with patient in lateral recumbent position
- Staples or locking clips to renal pedicle
- Infiltration of trocar ports and extraction site with 30 ml of 0.5% levo-bupivacaine
- No urinary catheter or routine drains
Peri-operative Analgesia
- Preoperative oral slow-release ibuprofen, 1600 mg
- Intraoperative iv paracetamol near end of case
- Fentanyl 2mcg/kg towards the end of the case
- Postoperative regular paracetamol and codeine, if needed
- Rescue intravenous fentanyl, if required
Take Home Medication
- Slow release ibuprofen, paracetamol and codeine for 5 days
- Buccal antiemetics if PONV problematic while in hospital
Organisational issues
- Surgeon must be experienced in laparoscopic perirenal procedures with a low rate of complications
- District nurse follow-up after discharge (at least during early phase of learning curve)
- Written information listing warning signs of serious postoperative complications and patients encouraged to self-refer to the surgical assessment unit if these signs are present
- As with cholecystectomy, immediate postoperative outcome is difficult to predict, so increasingly a default to day case booking strategy is adopted
Common Pitfalls
- Wound drains are not a substitute for careful haemostasis
- We do not routinely measure urine output or renal function as small, asymptomatic changes do not alter management
- Anticipated Day Case Rates
- 15–20% (for both benign and malignant)
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40111/hidi-smith_lapneph-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse13
Click on the image to be taken to the HCUK page about the conference or download the pdf
from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42053/bads-day-case-major-knee-surgery-oct-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse14
Click on the image to be taken to the HCUK page about the conference or download the pdf
from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42054/bads-day-case-hip-nov-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse15
Click on the image to be taken to the HCUK page about the conference or download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42055/bads-day-surgery-gynaecology-nov-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse16
Click on the image to be taken to the page about the event or download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42060/siva_virtual_event_flyer_2020__1_.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse17
Click on the image to be taken to the HCUK page about the conference or download the pdf
from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42056/breast-surgery-manc-dec-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse18
Click on the image to be taken to the HCUK page about the conference or download the pdf
from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42057/bads-general-surgery-dec-2020.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse19
General Guidelines
The Journal of One-day Surgery considers all articles of relevance to day and short stay surgery. Articles may be in the form of original research, review papers, audits, service improvement reports, case reports, case series, practice development and letters to the editor. Research projects must clearly state that ethics committee approval was sought where appropriate and that patients gave their consent to be included. Patients must not be identifiable unless their written consent has been obtained. If your work was conducted in the UK and you are unsure as to whether it is considered as research requiring approval from an NHS Research Ethics Committee (REC), please consult the NHS Health Research Authority decision tool at http://www.hra-decisiontools.org.uk/ethics/.
Articles should be prepared as Microsoft Word documents with standard line spacing and normal margins. Submissions must be sent by email to the address below.
Copyright transfer agreement and submission
As of 7th November 2019, the JODS copyright transfer agreement must be downloaded from the resources section (tab) via the BADS website:
https://daysurgeryuk.net/en/resources/documentation/
Each named author should complete and sign a copy. Scanned copies/legible photos should be sent via email together with the main manuscript to the JODS editor: davidbunting@nhs.net
Any source of funding should be declared and authors should also disclose any possible conflict of interest that might be relevant to their article.
Submissions are subject to peer review. Proofs will not normally be sent to authors and reprints are not available.
Manuscript preparation
Title Page
The first page should list all authors (including their first names), their job titles, the hospital(s) or unit(s) from where the work originates and should give a current contact address for the corresponding author.
The author should provide three or four keywords describing their article, which should be as informative as possible.
Abstract
An abstract of 250 words maximum summarising the manuscript should be provided and structured as follows: Introduction, Methods, Results, Conclusions.
Main article structure
Manuscripts should be divided into the following sections: Introduction, Methods, Results, Discussion and References. Tables and figures should follow, with each on a separate page. Each table and figure should be accompanied by a legend that should be sufficiently informative as to allow it to be interpreted without reference to the main text.
All figures and graphs are reformatted to the standard style of the journal. If a manuscript includes such submission, particularly if exported from a spreadsheet (for example Microsoft Excel), a copy of the original data (or numbers) would assist the editorial process.
Copies of original photographs, as a JPEG or TIFF file, should be included as a separate enclosure, rather than embedding pictures within the text of the manuscript.
Tables, Figures and Graphs
Please submit any figures, graphs and images as separately attached files rather than embedding non-word files into the Word document. Tables constructed in MS Word can be left in their original MS Word file including the manuscript if this is where they were drawn.
Figures and graphs can be presented in STRONG colour (please avoid tints and shades which may be too light to view onscreen in tablets). Try to avoid 3-d effects etc. Figures and graphs may be redrawn if the quality is not in keeping with the Journal. Please make it clear within the manuscript text where you would like tables, graphs or images to be placed in the finished article with the use of a brief explanatory legend in the manuscript file where you wish the item to be placed, e.g.
Table 1. Patient demographic details.
Figure 1. Proportion of procedures performed as a day-case each year between 2005 and 2018.
Photographs
Photographs can be provided as jpg or tiff files but should be included as a separate enclosure, rather than embedded within the text of the manuscript. This ensures higher quality images. However, we will accept images within Word documents but image quality might suffer!
References
Please follow the Vancouver referencing style:
- References in the reference list should be cited numerically in the order in which they appear in the text using Arabic numerals, e.g. 1, 2, 3, 4 etc.
- The reference list should appear at the end of the paper. Begin your reference list on a new page and title it 'References.'
- Cite articles in the manuscript text using numbers in parentheses and the end of phrases or sentences, e.g. (1,2)
- Abbreviate journal titles in the style used in the NLM Catalogue: https://www.ncbi.nlm.nih.gov/nlmcatalog?Db=journals&Cmd=DetailsSearch&Term=currentlyindexed%5BAll%5D
- The reference list should include all and only those references you have cited in the text. (However, do not include unpublished items such as correspondence).
- Check the reference details against the actual source - you are indicating that you have read a source when you cite it.
- Be consistent with your referencing style across the document.
Example of reference list:
- Ravikumar R, Williams J. The operative management of gallstone ileus. Ann R Coll Surg Engl 2010;92:279–281.
- Dybvig DD, Dybvig M. Det tenkende mennesket. Filosofi- og vitenskapshistorie med vitenskapsteori. 2nd ed. Trondheim: Tapir akademisk forlag; 2003.
- Beizer JL, Timiras ML. Pharmacology and drug management in the elderly. In: Timiras PS, editor. Physiological basis of aging and geriatrics. 2nd ed. Boca Raton: CRC Press; 1994. p. 279-84.
- Kwan I, Mapstone J. Visibility aids for pedestrians and cyclists: a systematic review of randomised controlled trials. Accid Anal Prev. 2004;36(3):305-12.
- Barton CA, McKenzie DP, Walters EH, et al. Interactions between psychosocial problems and management of asthma: who is at risk of dying? J Asthma [serial on the Internet]. 2005 [cited 2005 Jun 30];42(4):249-56. Available from: http://www.tandf.co.uk/journals/.
Mr David Bunting
Editor, Journal of One Day Surgery
Consultant Upper GI Surgeon
North Devon District Hospital
[These guidelines were last revised on 02.11.2019]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/39964/author-guidelines.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=2008#collapse21