Tim Rowlands
Tim Rowlands
We end one year and move into 2018. We’ll no doubt see many new day case developments in the coming year.
In this edition there are several widely different articles which I hope you will find topical and interesting. I mention several here: Raja et al looked at the implementation of a pathway for improving post operative discharge, demonstrating reduced rates of urinary retention. Deshmukh and Belfield looked at a rather neglected topic of compartment syndrome in the day case orthopaedic setting. Howard Cox presents questionnaire results from a study of patients’ attitudes to physician assistants in anaesthesia in his institution.
I am about to step down as Editor of the Journal of One-Day Surgery; for edition 28.1 we will have a new one, David Bunting, a consultant surgeon and current member of BADS Council. I would like to wish him every success in the role. I would also like to thank our President, Mary and the rest of the team at BADS past and present who have helped and supported me (or aided and abetted; delete as appropriate) in my time as Editor and on Council.
Tim Rowlands
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6170/273-editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse0
 Mary Stocker
Mary Stocker
I hope that you enjoy this second electronic edition of JODS and in particular the reflections, reports and photographs from our Annual Scientific Meeting in Southport. Once again, our Conference Secretary Kian Chin pulled off an outstanding programme of speakers. There were many highlights during the two days however for me one of the biggest revelations was that in Southampton it is possible to have neurosurgery as a day case. BADS has been working tirelessly with innovators and enthusiasts across the country for years to see opportunities to bring new procedures into the day surgery arena and encourage those who do so to spread the work and support other trusts to follow. Ten years ago we are tackling cholecystectomies and tonsillectomies. Now these are routinely undertaken as day surgery in most trusts across the country however that was certainly not the case 10-15 years ago. Since that time, we have seen innovations up and down the country which have brought, hysterectomies, nephrectomies, mastectomies, thyroidectomies, unichondylar knee replacements into the realms of day surgery and now neuro-surgery. There has been a seismic shift over the past decade and the fact that in some centres day surgery is the norm for these major procedures demonstrates that we really are able to support the claim that day surgery should be the standard of care for the majority of elective surgery. The delegate feedback from our ASM was once again outstanding however we could not fail to notice that delegate numbers were significantly down on previous years. We are aware that in these cash-strapped times it is difficult for staff to be released from work to attend such meetings and that the costs can also become prohibitive. At our council meeting in September we will be considering what we can do to make the ASM more accessible to you our membership. We would greatly value your input into these discussions so please do get in touch with the bads office if you have any suggestions. If you did not join us in Southport what stopped you from doing so? In particular should we be looking at more central venues? Is the delegate registration price too high? If we had a one day meeting rather than two would that make you more or less likely to attend? All options are on the table but your input would be hugely helpful. If you were unable to attend the meeting as usual all the lectures were recorded and are now available to watch via the members area of the website. They are highly recommended.
Last week the “Getting it Right First Time” programme published their National Specialty Report for General Surgery. Getting it right first time is a national programme designed to improve medical care within the NHS by reducing unwarranted variations and sharing best practice between trusts. In this report they have once again stressed the importance of embracing day surgery and reducing the variation in day surgery rates between trusts. The GIFT programme aims to serve as a further catalyst to enhance patient care, improve outcomes and drive efficiency. We very much hope that further adoption of day surgery will be a major focus within this.
Finally I hope you have managed to access this edition of JODS successfully. As with all new ventures there may be feedback from our users that we need to receive, please send it in so we can strive to continue to improve the service we offer to you our members.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6169/273-pres.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse1
Katharine Davies, Ingrid Hinden, Rachel Fletcher, Venkat Srinivasan
Abstract
Introduction
Day-case thyroid surgery isn’t routine practice in many hospitals due to fear of potentially life-threatening complications. This single-hospital study reviewed all patients listed for hemi-thyroidectomy as day-cases over a 26-month period assessing what factor(s) influenced successful same-day discharge.
Methods
We analysed notes of patients listed between October 2012 and January 2015 with special reference to delayed discharge, complications and re-admission.
Results
We performed 95 hemithyroidectomies that had been listed as a day-case (81 females, 14 males), 56% were discharged on the same day. Of the 53 patients who were on the morning lists, 79% were discharged home the same day. Of the 42 afternoon patients, 74% had to stay overnight. No patients were re-admitted with haematoma or bleeding.
Conclusion
We show that day-case hemithyroid surgery can be safely performed without occurrence of delayed bleeding or haematoma. The key factors for successful discharge include adequate time for observation post-operatively, low volume thyroids and the intra-operative use of energy sources for haemostasis.
Introduction
In the current climate of increasing pressure on the NHS, surgeons are continually reassessing their surgical practice and the surgical procedures that can be managed as a day-case without compromising patient safety. This would not only produce cost benefits but also mean fewer cancellations due to lack of inpatient beds and more resources being available for emergency patients. It has been shown to provide greater patient satisfaction and also reduces the risk of hospital acquired infections.1 Above all else, patient safety is the most important priority for all day-case surgical procedures and therefore, day-case thyroid surgery can only be advocated if patient safety is ensured. The National Health Service set out the plan in 2000 to try and achieve a 75% day-case rate on elective procedures.2 The British Association of Day Surgery, in 2001, added that we should be trying to achieve a 50% same-day discharge rate for partial thyroidectomy; however this practice does not seem as common in the UK as elsewhere, as less than 1% of all thyroid cases are done in this manner.3-6
The main complications leading to concern about day-case thyroid surgery are: hypocalcaemia, recurrent laryngeal nerve damage and delayed post-operative bleeding leading to airway compression. Post-thyroidectomy haemorrhage associated with laryngeal oedema and airway compromise has been reported to occur after 0.9-2.1% of all thyroidectomies.5 The major argument against day-case surgery is the prospect of delayed bleeding and haematoma after discharge.6
Much of the literature on day-case surgery pools together both hemithyroidectomy and total thyroidectomy cases, whereas in our practice we are advocating hemithyroidectomy only to be performed as a day-case procedure in a carefully selected patient population, and there is inadequate information in this select group to arrive at meaningful conclusions. If only hemi-thyroidectomy procedure is considered for its suitability as day-case, the potential complications would be delayed bleeding and haematoma that can lead to airway compromise and one of the main objectives of this study is to assess the occurrence of these events.
In this retrospective study, we have reviewed the data on a group of patients who underwent planned day-case hemi-thyroidectomies in an attempt to ascertain any factors which enabled or precluded same day discharge.
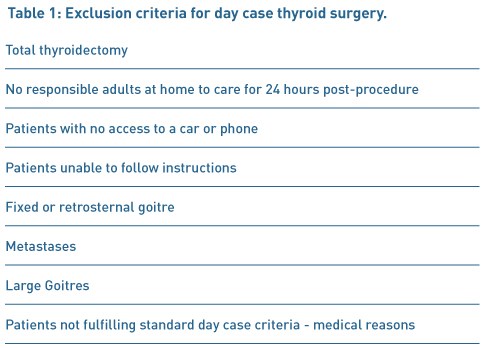
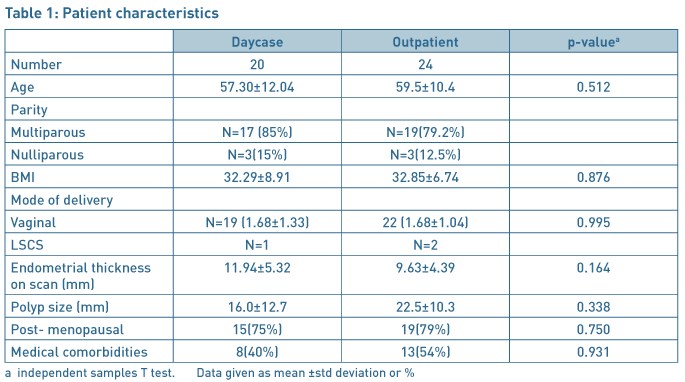
Methods
A retrospective study was completed on data from all patients who had undergone hemithyroidectomy as a day-case procedure between October 2012 and January 2015. A total of 132 hemi-thyroidectomies were performed during this period by a single surgeon (VS) with 95 fitting the criteria for day case discharge. Of the 95 patients that were included in the study, 14 were men (mean age 60 years with a range of 41-82) and 81 were women (mean age of 52 years with a range of 18-98). All the patients were appropriately consented with explanation of all possible complications. The prospect of delayed bleeding was particularly mentioned and the need to return to the hospital immediately, in case of neck swelling and bleeding, was emphasised. All patients underwent pre-operative assessment to ensure their suitability for day-case care and had their vocal cord movement checked and recorded when being listed for the procedure (Table 1).
Patients were admitted to the day-case unit on the morning of the procedure and once again the possible complications were explained to the patients. A standard hemi-thyroidectomy technique was employed and all through the procedure, energy source (Ligasure, Covidien) was used for dissection and haemostasis. When dissecting closer to the nerve, bipolar diathermy was used. Continuous laryngeal nerve monitoring was used in all cases. Drains were used in most of the cases. A continuous prolene suture with beads at both ends was used to close the external wound; this was removed at their local GP practice a week later. Patients were managed post-operatively on the day-case ward. They were reviewed by the senior author prior to discharge. Those with stable observations for 6 hours and without any complication were considered suitable for discharge home into the care of a responsible adult, after fulfilling the day-case discharge criteria. Patients were followed up in the out-patient clinic around 3 weeks or sooner, if necessary. Chi-squared testing was used to see if there was a significant difference between patients operated on in the morning and in the afternoon
Results
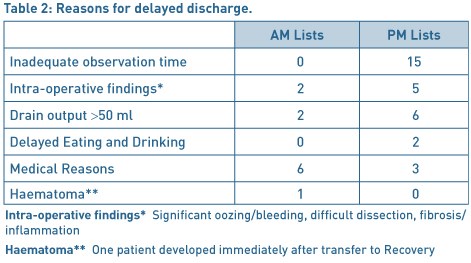
Fifty three patients (56%) were successfully discharged home on the day of surgery with 42 patients having to remain in hospital for at least one night. The reasons for overnight admission are given in Table 2. Out of the 53 patients operated in the morning lists, 42 were discharged home (79%) the same day as compared to only 11 patients (26%) out of the 42 patients from the afternoon lists (p<0.01). The most common reason for overnight admission in the case of afternoon patients was the lack of observation time available. In some cases, a decision was made during the surgery to keep the patients overnight due to intra-operative findings such as difficult dissection, excessive bleeding or adherence due to inflammation. Medical reasons were mainly relating to delayed recovery including nausea and vomiting. One patient developed haematoma immediately after transfer to the recovery and therefore she was taken back to theatre for exploration and haemostasis. There were no readmissions from the discharged group, due to haematoma or bleeding.
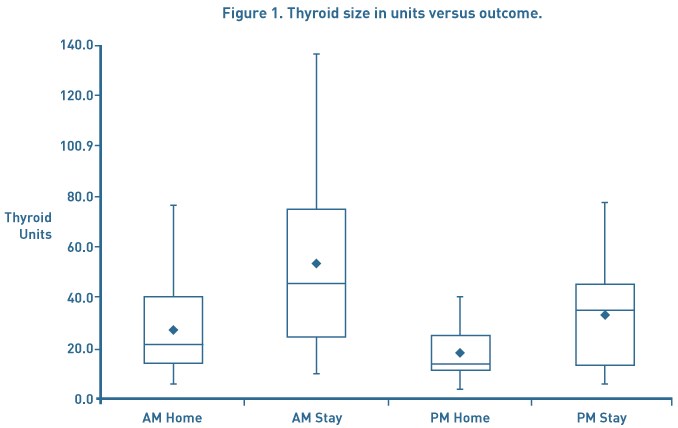
Thyroid size was calculated using the method described by Shabana et al. who multiplied the volume of each lobe by a correction factor of 0.529. This was used as it is not our routine practice to get pre-operative CT scans unless clinically indicated.7 The thyroid volume was analysed to assess whether this had any impact on discharge. Overall the average thyroid size was 32.8mls. Patients operated on in the morning who stayed at least 1 post-operative day had an average thyroid volume of 50.3mls compared to those who were discharged of 30.8mls. A similar pattern was seen in the afternoon patients with those being discharged home the same day having a thyroid volume of 19mls compared to 33.6mls (see Figure 1).
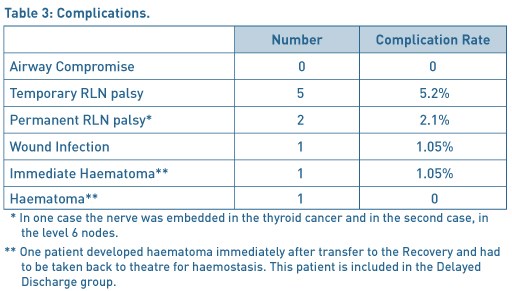
Overall there were 9 complications (9.4%) as documented in Table 3.
Discussion
Steckler in 1986 and then Mowschenson in 1995 were the first authors to suggest day-case thyroid surgery and came under intense scrutiny and criticism for advocating this.8,9 Steckler performed 48 hemithyroidectomies as day-case procedures of which 4 were kept in due to intra-operative findings. None of the discharged patients were readmitted with complications. Mowschenson successfully discharged 39 hemithyroidectomy patients home after observation of 6 - 8 hours and also had no re-admissions. Since then it has become increasingly popular in clinical practice, particularly in the USA. Some surgeons favour 23-hour surgery and feel this should be the case until a strict criteria for patient selection and better research into who is at risk of post-operative bleeding can be ascertained.5,10
The main concerns with day case thyroid surgery are unilateral recurrent laryngeal nerve damage with dysphagia and possible aspiration in some cases, bilateral recurrent laryngeal nerve damage leading to airway compromise, delayed post-operative bleeding and hypocalcaemia.11 Our study concerns only hemithyroidectomies and the relevant factors against day case surgery would be delayed bleeding and haematoma leading to airway compromise. Multiple authors have shown successful day case thyroid procedures without readmission due to bleeding. Teoh et al. performed 50 hemithyroidectomies with a discharge rate of 98%.12 Symes et al. successfully discharged 73 out of 75 patients within 8 hours of the procedure.13 The other two were kept for medical reasons. Howat et al. and Terris et al. discharged 75% and 83% of hemithyroidectomies home as day case respectively with no readmissions due to haematoma or bleeding.14, 15
The surgical techniques have evolved over time particularly for dissection and for achieving haemostasis. The newer technologies, used for haemostasis, have a significant effect in reducing the post-operative bleeding rate. Historically sutures such as silk and vicryl were used for tying the blood vessels with the potential for slippage and consequent bleeding after a few hours. In the recent years, the use of ties has declined and increasingly energy sources such as Harmonic and Ligasure are employed during surgery. Lepner demonstrated that the use of the LigaSure decreased the operation time with lower drain volume, hospital stay and a lower complication rate.16 This was felt to be due to the fact that LigaSure delivers precise amounts of energy resulting in less thermal damage to the surrounding tissues such as the RLN and parathyroid glands. Multiple papers add weight to the argument that Ligasure decreased the operating time, ensured adequate haemostasis and they had no re-admissions with post-operative haemorrhage.17-20 Inabnet felt that the use of sutureless vessel ligation was superior over older techniques and that the important consideration was meticulous haemostasis of both the upper and lower pole.19 The paper showed that they only had one haematoma within an hour of the operation in a group of 224 patients but it does not mention whether it was a total or partial thyroidectomy. Interestingly, sutures were not used at all for haemostasis in any of the cases in our series.
Currently there is no consensus regarding the optimal duration of observation in the post-operative period, before the patient can be discharged safely. Delayed bleeding, after 24 hours, has been reported, with Leyre et al having 7 bleeds after 24 hours, however, apart from one case these were all total thyroidectomies.22 Burkey et al looked at 13,817 thyroid and parathyroid surgeries and showed there to be 18 bleeds within 6 hours, 16 from 6 until 24 hours and 8 cases after 24 hours.23 This being the case it argues against even 23-hour surgery and the patient should stay for at least 24 hours but can this really be justified when there is substantial evidence involving high volume of patients, showing large results with no readmissions due to post-operative bleeding? 11,15
In 1998 Lo Gerfo et al. performed a review of post-operative bleeding over a 20 year period where they identified 21 cases 24. They found that there was a critical period of time in which most bleeding occurred and in all cases the patient showed signs of bleeding within a few hours and the potential for airway compromise was recognised within 4 hours. This supports the early discharge of patients and is mirrored in our results where no patients were re-admitted due to bleeding or neck swelling. In our series one patient developed significant haematoma but this occurred soon after the patient was transferred to the Recovery and this patient was taken back to theatre for haemostasis. It should be noted that none of the patients in our series developed delayed bleeding after transfer back to the ward or after discharge from the hospital.
As in all surgical disciplines, it is difficult to try and predict which patients will have post-operative bleeding, following thyroid surgery. Leyre in 2008 analysed 6830 cases of which 70 had bleeding post-operatively.22 They found that age, gender and the type of thyroid disease were not related to haematoma formation. They also found that anticoagulation or antiplatelet therapy did not have an influence on bleeding. As regards the timing of the bleeds they found that 37 happened within 6 hours, 26 up until 24 hours and 7 after 24 hours. The majority of these were total thyroidectomies which is not a direct comparison with our study. Looking at their hemithyroidectomy bleeding rates they found that they had 7 (0.4%) within 6 hours, 4 (0.2%) up until 24 hours and 1 (0.06%) after 24 hours. In this paper they do not comment on the haemostatic technique and it could be that the more traditional methods were used.
A parallel can be drawn between day case thyroid surgery and adeno-tonsillectomy. Surgical practice has evolved and changed from the era of keeping adenoidectomy and tonsillectomy patients for several days to the current practice of discharging them on the same day, including the paediatric population. The paper by Leyre et al is quoted by Doran et al as a reason why thyroid surgery should not be done as a day case but when looking at the data and seeing that only 0.3% of all hemithyroid cases had haematoma formation with no further information about these individual cases and what techniques have been used can it really be the reason why all day case surgery should not be considered at all?
Materazzi et al. have devised strict selection criteria for day-case thyroid surgery.25 Anaesthetic criteria includes ages 10-85, ASA grade 1 or 2, a low intubation score and BMI less than 32. Surgical criteria included primary neck surgery, being euthyroid, gland size less than 80ml and no locally advanced malignancies or intra-thoracic goitres. Social criteria includes adequate home support, a suitable living situation and the possession of a telephone. This is a very reasonable selection criteria and is the policy that we adopt with the exception that we do not do total thyroidectomies or children as day case procedures.
We are aware that one of the limitations of our study is the small number but we feel that our series can help arrive at reasonable conclusions, particularly with regard to patient safety. Increasing use of energy sources for dissection and haemostasis has transformed the thyroidectomy surgical procedure in terms of reducing the surgical time and ease of operating. We also feel that the energy sources are helpful in preventing delayed bleeding and haematoma after a reasonable period of monitoring post-operatively. We strongly feel that our number in this study, though small, is adequate to show that with the use of energy sources and adequate post-operative observation time, day-case hemithyroidectomy can be done safely in a selected patient group.
Conclusion
We believe that consideration should be given to perform hemithyroidectomy as day case procedure. Our results have shown that this can be done safely in a reasonable number of patients. We conclude that with careful patient selection and at least 6 hours of post-operative observation day-case hemithyroidectomies can be performed safely. In order to ensure safety, there does need to be strict case selection and thorough information provided to the patients. Our results show that patients operated on the morning lists are more likely to be discharged home on the same day, mainly due to the adequate observation period. It is our opinion that with the use of energy sources for haemostasis and dissection, delayed bleeding can be prevented. In this paper we have shown that with a carefully selected group of patients the overall day case rate can be higher than 50%, as advocated by the day-case surgery group, and can be safely improved upon if operated in the morning. We will continue to audit our practice to assess whether this improved discharge rate continues.
Financial Support
This study received no specific grant from any funding agency, commercial or not-for-profit sectors.
References
- Sahmkow S, Audet N, Nadeau S, Camire M, Beaudoin D. Outpatient Thyroidectomy: Safety and Patients’ Satisfaction. Journal of Otolaryngology- Head and Neck Surgery. Vol 41. No S1 (April), 2012: ppS1-S12
- Department of health. The NHS Plan. London: DH; 2000
- Cahill CJ. Basket cases and trolleys - day surgery proposals for the millenium. Journal of one-day surgery. 1999 ,9. 11-12
- Sahai A, Symes A, Jeddy T. Short-stay thyroid surgery. Br J Surg 2005; 92: 58-59
- Doran H.E, England J, Palazzo F. Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl 2012; 94: 543-547
- Doran H.E, Palazzo F. Day-case thyroid surgery. BJS 2012;99: 741-743
- Shabana W, Peeters E, De Maeseneer M. Measuring Thyroid Gland Volume: Should We Change the Correction Factor? AJR: 186, January 2006
- Steckler RM. Outpatient thyroidectomy: a feasibility study. Am J Surg 1986; 152: 417-419
- Mowschenson PM, Hodin R. Outpatient thyroid and parathyroid surgery: a prospective study of feasibility, safety and costs. Surgery 1995; 118: 1051-1053
- Mirnezami R, Sahai A, Symes A, Jeddy T. Day case and short stay surgery: the future for thyroidectomy? Int J Clin Prac 2007; 61: 1216-1222
- Snyder S, Hamid K, Roberson C, Rai S, Bossen A, Luh J. Outpatient thyroidectomy is safe and reasonable: experience with more than 1000 planned outpatient procedures. J Am Coll Surg 2010; 210:575-584
- Teoh AY, Tang Y, Leong H. Feasibility study of day case thyroidectomy. ANZ J Surg 2008; 78: 864-866
- Symes A. et al. Daycase thyroidectomy. Annual meeting of the British Association of Endocrine Surgeons, Lund, Sweden, 2004. (Abstract)
- Howat G, Weisters M, Sames M, Mclaren M. A Pilot Study of Day Case and Short-stay Thyroid Surgery. The Journal of One-Day Surgery (2006) Vol 16, No 1
- Terris D, Moister B, Seybt M, Gourin C, Chin E. Outpatient thyroid surgery is safe and desirable. Otolaryngology – Head and Neck Surgery (2007) 136, 556-559
- Lepner U, Vaasna T. LigaSure vessel sealing system versus conventional vessel ligation in thyroidectomy. Scan J Surg 2007, 96 (1) 31-4
- Lachanas V, Prokopakis, Mpenakis A, Karatzanis A, Velegrakis G. The use of ligasure vessel sealing system in thyroid surgery. otolaryngol head neck surg march 2005 volume 132 number 3 487-489
- Schiphorst A, Twigt B, Elias S, Dalen T. Randomized clinical trial of LigaSure versus conventional suture ligation in thyroid surgery. Head & Neck Oncology 2012, 4:2
- Inabnet WB, Shifrin A, Ahmed L, Sinha P. Safety of same day discharge in patients undergoing sutureless thyroidectomy: a comparison of local and general anaesthesia. Thyroid 2008; 18: 57-61
- Seybt MW, Terris D. Outpatient thyroidectomy: experience in over 200 patients. laryngoscope 2010; 120: 959-963
- Rosenbaum MA, Harida M, McHenry C. Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg. 2008 Mar; 195 (3): 339-43
- Leyre P, Desurmont T, Lacoste L, Odasso C, Bouche G, Beaulieu A et al. Does the risk of compressive haematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg 2008; 393: 733-737
- Burkey SH, van Heerden JA, Thompson GB, Grant CS, Schleck CD, Farley DR. Re-exploration for symptomatic haematomas after cervical exploration. Surgery 2001; 130:914-919
- Lo Gerfo P, Gates R, Gazetas P. Outpatient and short-stay thyroid surgery. Head Neck 1991; 13: 97-101
- Materazzi G, Dionigi G, Berti P, Rago R, Frustaci G, Docimo et al. One-day thyroid surgery: retrospective analysis of safety and patient satisfaction on a consecutive series of 1,571 cases over a three year period. Eur Surg Res 2007; 39: 182-188
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6168/273-davies.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse2
Crispin Weidmann Consultant Neuroanaesthetist, Wessex Neurological Centre, University Hospital Southampton NHS Foundation Trust, Southampton SO16 6YD
Paul Grundy Consultant Neurosurgeon, Wessex Neurological Centre, University Hospital Southampton NHS Foundation Trust, Southampton SO16 6YD
Introduction
Cranial neurosurgery undertaken as daycase or ambulatory surgery (discharged home within 24hours of surgery) is not universally accepted within neurosurgical units in the United Kingdom.
In 2006 University Hospital Southampton set up a cranial neurosurgical daycase service for brain biopsy and tumour resection by craniotomy.
We undertook the first reported daycase awake craniotomy1 by the end of that year.
The service challenged practice in the United Kingdom, but mirrored services in Toronto, Canada, led by Mark Bernstein (consultant neurosurgeon).
Rationale
The NHS plan in 2000 had ambitious targets of 75% of elective surgery being undertaken as daycases. This was supported by the operational guide for day surgery in 2002. Enhanced recovery programmes have shown improved patient outcomes in multiple surgical specialties 2 with reduced length of stay.
Concerns about risk in discharging patients the same day or within 24hours were assessed prior to the service starting. The timing of intracerebral haemorrhage after craniotomy has been studied3 and all patients receive a CT brain scan 4 hours after surgery if going home the same day. Patient discharged home within 24hours receive either and MRI or CT Brain the morning after surgery. Any patient with asymptomatic haematoma is kept in hospital. Seizure activity after cranial neurosurgery is a risk, but it can occur at any time after surgery.
(Article continues after advertisement. Click on image to go to the company website.)
Implementation
Setting up such a service relies on team work. Enhanced recovery methodology was used, addressing various parts of the patient pathway. Focus was given to outpatient clinics, surgery, post operative care and early mobilisation.
Setting expectation in clinic, such as sedation rather than general anaesthesia and daycase or discharge within 24hours is seen as a key to success. We aimed to reduce operative stress by using improvements in neuro-navigation systems, coupled with the evolution of anaesthetic delivery equipment. This, in addition to better short acting titratable anaesthetic drugs such as propofol, remifentanil and more recently dexmedetomidine, allow shorter craniotomy times with either sedation or general anaesthesia.
Conscious sedation throughout is our technique of choice for brain biopsy and awake craniotomy for tumour resection close to or within ‘eloquent’ brain.
Patient satisfaction questionnaires post operatively have shown that this is extremely well tolerated 4
General anaesthesia using target controlled infusions (TCI) of propofol and remifentanil allows rapid wake up with minimal hangover effect. Early mobilisation in the evening of the operative day is important for those going home the following morning. Empowering ward staff to drive the enhanced recovering programme is vital.
Results
Since 2006 we have undertaken over 650 brain biopsy around half of which were daycases. Our length of stay data for malignant brain tumours (GIRFT)5 after craniotomy is 1 day median (2.4 days mean) compared with over 6 days as national average, with the majority of cases discharged home by lunchtime the day after surgery.
Future
Sustainability and transformation plans require health care providers and local councils to coordinate delivery and timing of health care in England. The way healthcare is provided and the way it is delivered needs to change. Neurosurgery should not be immune to this.
References
- Weidmann C, Grundy PL. Day case awake craniotomy for tumour resection. Journal of One-Day Surgery 2008; 18(2):45-7
- Nicholson A, Lowe M C, Parker J, et al. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. British Journal of surgery 2014; 101: 172–188
- Taylor WA, Thomas NW, Wellings JA, Bell BA. Timing of postoperative intracranial hematoma development and implications for the best use of neurosurgical intensive care. Journal of Neurosurgery1995; 82:48–50
- Wahab SS1, Grundy PL, Weidmann C.Patient experience and satisfaction with awake craniotomy for brain tumours. British Journal Neurosurgery. 2011 Oct;25(5):606-13
- GIRFT Neurosurgery Review University Hospital Southampton NHS Foundation Trust
Dept of Health, Aug 2016, 21-22
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6167/273-weidmann.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse3
Dr Bhawana Purwar ST4 O&G, The Royal Wolverhampton Hospitals NHS Trust, United Kingdom
Dr Joanne Ritchie ST1 O&G, The Royal Wolverhampton Hospitals NHS Trust, United Kingdom
Dr Aditi Desai Consultant Obstetrician and Gynaecologist, The Royal Wolverhampton Hospitals NHS Trust, United Kingdom
Corresponding author: Dr Bhawana Purwar, 5, Cricket close, Walsall WS53PU. Tel: (+44) 7963881231.
E-mail: drbhawanapurwar@yahoo.com
Abstract
Outpatient and daycase hysteroscopy and polypectomy are widely recognised methods for the treatment of endometrial polyps. There have been concerns regarding pain affecting satisfaction and tolerability of the outpatient procedure.
We conducted a service evaluation of our outpatient hysteroscopy and polypectomy (OPHP) and compared it with our daycase procedures, which has shown excellent success rates and overall good satisfaction for both the services.
Introduction
Abnormal uterine bleeding accounts for as many as one-third of presentations to gynaecologists and requires further evaluation to establish a diagnosis in the most efficient and least invasive manner possible1, 2. Endometrial polyps are one of the major causes of abnormal uterine bleeding (AUB). The incidence rises steadily with the increasing age, peaks in the fifth decade of life and gradually declines after the menopause3. Hysteroscopy is considered the gold standard method for diagnosing the endometrial polyps. Endometrial polyps associated with AUB necessitate their removal and sometimes they may harbour malignancy as well (1-1.6%)(4). Despite the increasing popularity of office hysteroscopy, routine hysteroscopy is still performed in an operating theatre and require anaesthesia and hospitalization4.
In the UK, Royal College of Obstetricians and Gynaecologists (RCOG) recommends there is increased need for one-stop clinics where diagnosis and treatment can be done simultaneously. The Department of Health in the UK aims to provide two-week wait clinics for all suspected cancers to provide better services and to make or refute the diagnosis of endometrial cancer earlier. Office based diagnostic/therapeutic hysteroscopy is pivotal in providing these services.
Endometrial polypectomy can be successfully performed in the outpatient setting with minimal intraoperative discomfort, a significantly shorter time away from home and faster recovery and is preferred by women when compared with day case polypectomy(5). In our hospital, outpatient service for hysteroscopy and polypectomy (OPHP) is running successfully since Jan 2011. The service evaluation for outpatient or inpatient hysteroscopy and polypectomy has not been carried out in the department till date.
Methodology
Our aim was to evaluate the outpatient and day case hysteroscopy and polypectomy services by determining patient satisfaction, treatment outcomes, efficiency and cost-effectiveness of both services.
All patients over a period of October 2012 to April 2014 who had polyp confirmed on ultrasound scan, and who were booked for hysteroscopy & polypectomy were approached. Ethical approval was not needed as per advice from our local ethics committee as it was considered a service evaluation. The data was collected prospectively regarding patient demographics, indication for referral, menopausal status, operating time, complications, and failure rate, type of analgesia, number & size of polyps removed, recovery time and duration of inpatient stay.
Patient satisfaction questionnaire designed by the authors was given to the patients on the day of the procedure. A further questionnaire was sent to the patients by post after 3 weeks of discharge from the hospital to those who did not return the questionnaire. The patients were enquired about the leaflet given, pre-op analgesia, information given on the day of the procedure, pain during the procedure and following the procedure, maintaining their privacy and dignity, length of stay in hospital, post-op instructions and their overall satisfaction.
Pain was measured on a 0–10 visual analogue score (VAS) for pain with a score of 0 indicating no pain and a score of 10 indicating the worst pain imaginable. A Likert-type Scale was used for satisfaction with the explanation of the procedure, maintaining privacy and dignity of the patient and overall satisfaction with the service.
A semi-rigid hysteroscope (Karl-Storz), outer diameter- 3.5mm with bipolar electrode (versapoint)/ grasper forceps for polypectomy was used for OPHP with or without the use of local anaesthetic (LA); 0.9% normal saline was used as distension media. A rigid hysteroscope- Olympus (6.5mm with 4mm telescope) was used for the daycase hysteroscopy under general anaesthetic (GA). In daycase procedures, polyp forceps were mainly used for polypectomy with the occasional use of operating hysteroscope.
All patients had pre-assessment for suitability of the procedure for both LA and GA. All the women who presented with abnormal uterine bleeding had an ultrasound scan performed. Those women who were referred for OPHP procedure had polyp first confirmed on diagnostic outpatient hysteroscopy and then booked for the procedure slot. This was done to ensure the maximum utilisation of procedure slots and use trained personnel effectively. There were only few surgeons who could do both diagnostic and therapeutic procedures.
The data was analysed with Microsoft excel 2007 and SPSS 24.0 for mac.58 patients over a period of October 2012 to April 2014 consented to participate in the study. The pictorial histograms were used to check if the data was normally distributed and where appropriate, either Chi-square or independent sample T test was used. A p value of <0.05 was considered significant.
Results
14 patients were excluded as they did not fill the questionnaire or had no polyp found on hysteroscopy. Out of the 44 patients who returned the questionnaire, 24 patients had outpatient hysteroscopy and polypectomy and 20 patients had day case surgery done.
The groups were similar in terms of age, parity, BMI, mode of delivery and menopausal status (Table 1). There were more women with significant co-morbidities in the outpatient group than the daycase surgery group but it did not reach statistical significance (Table 1). In both the groups most of the women were parous and had achieved normal vaginal delivery.
The size of the polyp ranged from 20–30mm in outpatient group and 20-50mm in daycase surgery group. The patients who had polyps more than 30mm were booked for daycase surgery. The most common indication for referral for hysteroscopy was the post-menopausal bleeding with 13/20 (65%) and 17/24(71%) in daycase and outpatient groups respectively. Other indications were menorrhagia, irregular bleeding and incidental finding of polyp on the ultrasound scan.
17 % of patients in OPHP and 20% of patients in daycase group did not receive the pre-operative leaflet. In the OPHP cohort, patients did not take any oral analgesia prior to coming for the procedure. In 14/24 (58%) cases local analgesia (lignocaine 1% with 1:200,000 adrenaline) was used. In one patient, OPHP procedure had to be abandoned because of the pain and in one patient, there was no documentation for the use of local analgesia. Vaginoscopy was attempted in 3 patients but one of them needed cervical dilatation and speculum insertion, while the other 2 had successful vaginoscopy. Most patients had mild to moderate pain as shown in table for visual analogue score (Table 2). All the histology samples were followed up in each group and in one case adenocarcinoma of uterus identified on histology.

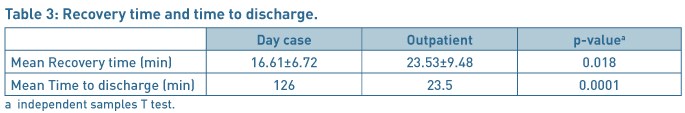
The mean time in recovery room just after the operation and mean time for discharge from the hospital was significantly different for both the groups as shown in Table 3. The polyp removal was successful in 23/24 (96%) women in the OPHP group. The patients were highly satisfied or satisfied with the explanation of the procedure in both the groups apart from 2/20(10%) patients in daycase group who were dissatisfied with the services provided as daycase.
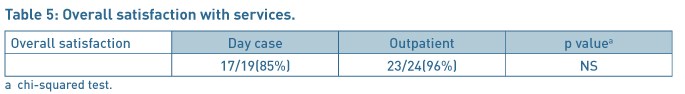
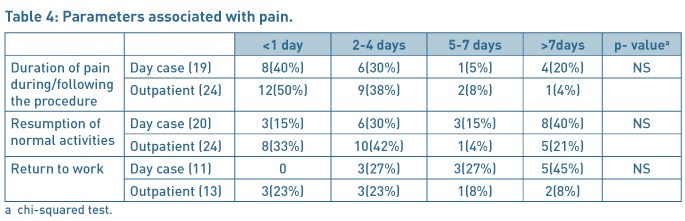
Patients (22/24 (92%)) were highly satisfied or satisfied with the privacy and dignity provided in the OPHP before /after surgery and 16/20(80%) patients in the daycase group. The severity of pain after the discharge to home, and duration to return to work and resumption of normal activities were comparable in each group (Table 4). 96% patients were highly satisfied or satisfied with the procedure for the outpatient services as compared to 85% in the daycase group (Table 5). 60% of patients in the daycase group had a preference to opt for the outpatient procedure next time, 15% would like to have the procedure done as daycase procedure and 25% had no preference given the choices. In the OPHP 46% would like the procedure to be done as outpatient, 29% would prefer to be asleep and have it done as a daycase procedure and 21% expressed no preference.
Discussion
Our study highlights that the outpatient management of endometrial polyps is safe, efficacious and feasible as supported by other studies(5–7). In a study by Litta et al(7), 253 polyps were removed as outpatient procedure with median time of 10min and a VAS ≤4 was obtained for polyps were ≤2 cm and menopausal status and vaginal deliveries were not significantly related to the VAS (visual analogue pain score). In our study, 7(42%) patients had VAS ≤4 and 12(50%) patients had VAS of 5-7 in OPHP. The mean VAS score was 4.69 for OPHP and 5.57 for daycase after the operation for daycase group, which did not reach statistical significance, most likely due to small numbers.
The time taken for the resumption of daily activities and the return to work was also less in the OPHP group then the daycase group, though not statistically significant. Our data demonstrates statistically significant reduction in recovery and discharge times as compared to daycase group. The mean time for discharge in daycase group was 126 min and 23.2 min for outpatient cohort (P=0. 0001). Similarly, in a randomised controlled trial by Marsh et al(5) women from the outpatient cohort had a significantly faster mean return to preoperative fitness (1 [0–4] day versus 3.2 [1–13] days; P = 0.001) and required less postoperative analgesia than the daycase cohort; women undergoing outpatient endometrial polypectomy had a significantly shorter mean time away from home than those undergoing the daycase procedure. This is likely to have significant positive implications on the bed capacity and the costs involved in achieving the treatment for women.
The Versapoint electrode fits easily into the semi-rigid hysteroscope and provides removal of polyps under direct vision. This ensures complete removal of the polyp and hence the better resolution of the symptoms. The average polyp size in our study population was 2–3 cm and was mostly single polyp. In our unit, most of the daycase polypectomy procedures are still performed as a blind procedure.
We would also like to emphasize that most patients done as OPHP cohort had significant morbidities including previous deep vein thrombosis, cardiac bypass, hypertension, diabetes, unstable angina and obstructive sleep apnoea which can prove challenging for general anaesthesia. The risks of general anaesthetic are conveniently avoided in the outpatient procedures.
The accessibility of OPHP services and shorter waiting time is likely to lead to quicker histological diagnosis. This could help us to lead to give prompt counselling and treatment in pre-cancerous cases. In terms of financial implications, the cost of surgeon, 2 nurses, kit and drugs for outpatient procedure was £423 while inpatient costs for surgeon, anaesthetist, nursing staff, drugs, kit and inpatient bed was £958.68. So there was a net saving of £535 per patient.
A recent review of ambulatory hysteroscopy by Cooper et al suggests that the current literature on these outpatient hysteroscopic techniques has demonstrated safety and feasibility, but evidence of effectiveness, patient acceptability and cost-effectiveness is lacking8.
In a multicentre randomised controlled non- inferiority study by Cooper et al, outpatient polypectomy was non-inferior to inpatient polypectomy. Failure to remove a uterine polyp was, however, more likely with outpatient polypectomy and acceptability of the procedure was slightly lower9. Our study also looked into the success rates and overall satisfaction of the outpatient procedure.
Our success rates were good and only 1 patient needed to be booked for inpatient procedure because of pain and inability to gain access. The reason for our higher success rates is that all the patients booked for OPHP were initially assessed first by diagnostic hysteroscopy. This resulted in not only high success rates but also better utilisation of services with appropriate allocation of time and staffing for the procedure lists. Our study demonstrated that, indeed, 96% of patients were satisfied with the outpatient hysteroscopy services.
To conclude the OPHP is cost-effective and efficient method with reasonable acceptability. It is well tolerated with remarkable success rates and excellent patient satisfaction. As compared to daycase group, it requires less time for recovery and sooner returns to work.
References
- Hatasaka H. The evaluation of abnormal uterine bleeding. Clinical Obstetrics and Gynecology. 2005;48(2):258–273.
- Readman E, Maher PJ. Pain relief and outpatient hysteroscopy: a literature review. Journal of the American Association Gynecologists Laparoscopists. 2004;11(3):315–319.
- Annan JJ A, Ball E. The management of endometrial polyps in the 21st century. The Obstetrician & Gynaecologist. 2012(14).
- Clark TJ, Khan KS, Gupta JK. Current practice for the treatment of benign intrauterine polyps: a national questionnaire survey of consultant gynaecologists in UK. European Journal of Obstetrics Gynecology and Reprod Biology. 2002;103(1):65–67.
- Marsh FA, Rogerson LJ, Duffy SR. A randomised controlled trial comparing outpatient versus daycase endometrial polypectomy. British Journal of Obstetrics and Gynaecology. 2006;113(8):896–901.
- Garuti G, Cellani F, Colonnelli M, Grossi F, Luerti M. Outpatient hysteroscopic polypectomy in 237 patients: feasibility of a one-stop "see-and-treat" procedure. Journal of the American Association Gynecologists Laparoscopists. 2004;11(4):500–504.
- Litta P, Cosmi E, Saccardi C, Esposito C, Rui R, Ambrosini G. Outpatient operative polypectomy using a 5 mm-hysteroscope without anaesthesia and/or analgesia: advantages and limits. European Journal of Obstetrics Gynecology and Reprod Biology. 2008;139(2):210–214.
- Cooper NA, Clark.T.J. Ambulatory hysteroscopy. The Obstetrician and Gynaecologist. 2013;15(3):159–166.
- Cooper NA, Clark TJ, Middleton L, Diwakar L, Smith P, Denny E, Roberts T, Stobert L, Jowett S, Daniels J, Group OPTTC. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. British Medical Journal. 2015;350:h1398.
(Click on image to go to the company website.)
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6163/273-purwar.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse4
Tim Rowlands
It was a pleasure to review the posters at this years annual scientific meeting in Southport. Although less in number than previous years, they covered a wide variety of topics relevant to daycase practice with many novel approaches to aspects of care and quality. As usual the standard of the posters was high and exceptional in presentation. We recognise the hard work for all concerned that goes into converting an abstract into an interesting and meaningful presentation. Certificates are awarded to those posters where the judges felt the work was particularly outstanding.
The judges this year were Theresa Hinde (Anaesthetist), Fiona Hindle (Nursing and Management) and myself (Surgeon). We would like to thank everyone who submitted abstracts and exhibited posters this year. I would particularly encourage you to consider expanding your work as seen in the posters and submitting for consideration for publication in the Journal of One Day Surgery as soon as possible.
Gold awards
P12 Reaudit of Day Case ACL Reconstruction at RJAH NHS Foundation Trust
P Craig, A Jaiswal, P Gallacher, R Longfellow
RJAH NHS Foundation Trust, Oswestry Shropshire, UK
P16 Mired in Inertia – A Drive to Increase Day Case Laparoscopic Cholecystectomy Rates
Margaret Aslet, Steven Wasawo
York Hospital NHSFT, York, UK
Silver awards
P7 Our patients are a fire hazard! Time for a culture shift in daycase fluid starvation?
Mark Abou-Samra, Katharine Stenlake
Musgrove Park Hospital, Taunton and Somerset NHS Trust, Taunton, UK
P15 Patient reported postoperative outcomes following day surgery in Leeds Teaching Hospitals NHS Trust (LTHT): Guiding quality improvement using TheatrePro
Lilian Loh, Monalisa Marbaniang, Indu Sivanandan
Leeds Teaching Hospitals NHS Trust, Leeds, UK
Bronze awards
P4 Audit of the Recording of Hba1c, Blood Pressure and BMI in Elective Surgical Referrals From Primary Care
Nazrul Islam2, Thazin Wynn2, Joseph Pease2, Anna Lipp1,2
1Norfolk and Norwich University Hospitals NHS Foundation Trust, Norwich, UK, 2Norwich Medical School, Norwich, UK
P5 Developing a laparoscopic cholecystectomy “recipe”
Anna Dunkley1, Kim Russon2, Helen Thornley1
1Sheffield Teaching Hospitals, Sheffield, South Yorkshire, UK, 2Rotherham Hospital, Rotherham, South Yorkshire, UK
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6166/273-posters.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse5

Paul Rawling
Your council team arrived on Wednesday prior to the opening of the Annual Scientific Meeting (ASM). The weather was pleasantly warm in Southport, the venue for our ASM for the 3rd time. A preview inspection of the venue was good and highlighted the bright, open spaces and excellent accessibility we had for the ASM this year. I was a little apprehensive this year as it had felt more difficult to mobilise the membership in the build up toward the ASM which is the major event we hold each year.

Day 1
After the official opening of the ASM by the President of BADS Dr Mary Stocker providing a very warm welcome to all the speakers and delegates the ASM was under way and immediately in full swing. Numbers of delegates were at a lower level this year than previously, which I personally was disappointed with, especially with the exceptional programme of speakers and workshops on offer this year. However the delegates who attended really privileged and were provided with a treat with the speakers within the programme providing some excellent discussion areas for the rest of the ASM and beyond. I continue to have discussions about the topic areas discussed over the 2 days. The enthusiasm of those in attendance was extremely pleasing for all the council members to see, as was the fact we had the opportunity to meet up with old friends and see so many new faces whom I hope feel engaged enough to submit an abstract or a poster of their great work for next years event in the fabulous city of Sheffield.
Following the introductions from Dr. Mary Stocker (President) and brief housekeeping notes from Paul Rawling (Honorary Secretary) we were straight into the first plenary session of the conference. The presentation of the European fasting guidelines for surgery which although not new still appear to be a secret from most of us despite being endorsed by the college of anaesthetists and AAGBI. These guidelines were delivered in 2011. Dr. Stocker was one of our speakers in this session and started that the guidelines had 'transformed my practice in the past 12 months’. As an experienced consultant Anaesthetist this is a powerful statement and is not to be taken lightly. It was also of benefit to hear of the work carried out in Torbay by Dr Mike Swart whose work developing high risk assessment clinics and shared decision making is well renowned and has been found to be extremely beneficial to patients.
Each year at BADS ASM we try to showcase a particular surgical specialty which is pushing previously unthinkable boundaries of day surgery. This year we were delighted to welcome a very special team from Southampton, Mr Paul Grundy and Dr Crispin Weidmann who shared their experiences of delivering a day surgical neurosurgery service. I have worked, in Operating Theatres, in Education as a lecturer and have spoken both nationally and internationally at conferences. This session left me nothing short of speechless, which I can assure you, does not happen often. I never imagined in my 38 years of experience in healthcare that I would hear the terms neurosurgery and day surgery mentioned in the same sentence. As our President suggested ‘Yes it can be done’. There is some fantastic work carried out all the UK everyday which leaves me in awe of my ultra talented colleagues. This for me was astonishing and a fantastic move forward within the day surgery speciality.
Following up on the previous sessions we have known for many years that good IT systems can help transform day surgery services and the team from Chester, Professor Paul Edwards and Dr Steven Moore shared their experiences with us. The overarching message from this session was the sharing of information in a logical and efficient manner. Clearly this is not effective enough in some areas. The current issues in healthcare informatics were discussed at length and included all the issues that appear relevant to all clinical practice at the moment. These areas included access to shared data, which was hoped to be dealt with with a computer system installed across the NHS and beyond, the role of the CCIO in clinical practice, the findings of the Wachter Report, standards in clinical correspondence as recommended by the Academy of Royal Colleges, clinical coding standards, tracking of patients and equipment and STPs and the link to informatics development across their footprints. Standardisation and sharing is the overarching key to success.
The free paper session is a very good way for all staff who wish to present their own or colleagues work from practice, in a relatively non-threatening environment. A variety of topic areas were presented this year including Mastectomy surgery, Day case Paediatric Tonsillectomy, Management of Abscesses using the ambulatory care abscess pathway, the implications of unplanned admissions in stand-alone units, the re-audit of unplanned admissions and the diagnosis of serious co-morbidities at pre-operative assessment. I would encourage members and non-members alike to work together and have a go at submitting an abstract or producing a poster. These are really good ways of getting your work recognised and even published in the Journal of One Day Surgery and will enhance any CV. The second free paper session was again well attended and had a really strong clinical feel about it. The sessions were again varied and included TURP Safety, cost benefit and patient satisfaction, the consenting process for elective inguinal hernia and the question of are we doing it right? The implementation of a protocol led anaesthetic approach to reduce day case gynaecological surgery failure rate, Hand and Wrist Day Surgery – Dream or Disaster? Unplanned admissions on a split site trust: The difference a day surgery unit makes and finally An Audit of Unplanned Admissions Following Arthroscopic Shoulder Surgery. I have an interest in the free papers as I believe publishing of work is vital to move the speciality forward and new writers are required all the time. The JODS Editor is awaiting your papers. Please do not let him down. The papers were well written and well delivered and essentially kept to the time allocated for each paper. These are skills which are learned and are transferrable and are worth having in your personal armoury.
This year there were 4 workshops planned during the conference. Each one was very well attended which I was delighted with. I am sure every delegate came away with some information and discussion of benefit to their practice, which could be fed back to teams and if possible implemented in practice. The workshops included Training in Day Case Surgery: Dilemmas and Tips with Mr. Dave Bunting, Miss Emma Court and Dr Teresa Hind, Sending patients home with Local Anaesthetic infusions with Dr. Robert Erskine, Day Case Breast Surgery with Mr. Kian Chin and Nursing Dilemmas in Day Surgery: An MDT Discussion with Ms Fiona Belfield and Mr. Paul Rawling. Being personally involved in the latter workshop I can say it was excellent, a great deal of discussion took place around a variety of issues, which were predominantly common amongst all in attendance. Standardised processes, outlier activity, discharge criteria, staggered admissions and staffing of day surgery departments. Yes a variety of issues, but common to most of us in the room. I was encouraged with the attendance and the multidisciplinary mix within the delegates in the session. This was also demonstrated across all the other workshops.
This year saw a reduced number of high quality posters accepted and they were all professionally formatted and beautifully produced. The posters were popular during breaks and lunch periods and did get a lot of views and I spoke with a number of presenters and onlookers during the break periods and the feedback was largely positive. The topic areas were numerous and included Laparoscopic Cholecystectomy and surgical outcomes, Solving the consent problem, Post-Operative Pain Relief after discharge, Audit of recording of HBA1C, BMI and BP in Primary Care, Pre-operative fasting, Paediatric Tonsillectomy, Audit of ACL reconstruction, Mastectomy, Post-Operative patient reported outcomes, Increasing Laparoscopic Cholecystectomy rates and Streamlining emergency ureteric colic management. I have never produced a poster and I always admire the skill required to do so, in selecting what to include and what to leave out. Well done to everyone who took part and congratulations to those who received a Gold, Silver or Bronze certificate. Again a great way to get your work published and viewed by colleagues and friends which is a step in the right direction for our professions and for you personally.

The Annual General Meeting indicated the end of day one of the ASM. A good number of members attended this meeting. Council members with officer roles provided there brief annual reports to the meeting including the treasurer, honorary secretary and publications officer. A small number of resolutions were put forward, voted on and passed at this meeting. Following the AGM everyone went away to prepare for the Networking Dinner. This was a standout event and everyone enjoyed the occasion, well attended and well behaved and an excellent way for networking to take place. The food and drink were excellent and this proved to be a very pleasant social event for all.
Day 2
The day saw a plenary session around Ambulatory Emergency Care from Dr. Vincent Connelly, Deborah Thompson and Darren Leech. The team from NHS Elect delivered some thought provoking discussion worthy of further consideration. The session included a variety of people issues and process matters, as well as a practical guide to optimizing the clinical working environment to encourage the Day surgery emergency care process to develop locally and flourish. A lot was said in 2016 at the ASM about emergency care in day surgery and yes it can be done, but requires specific management and processes to be in place. I enjoyed the session and found that the issues are not insurmountable at all some of us just think they are as we have not considered them previously.
The prize paper presentations are always hotly contested and 2017 was no exception. The diversity of these presentations is a joy to behold and demonstrates that Day Surgery is at the cutting edge (excuse the pun) of current surgical care. The topic areas were very much forward thinking and included Patient satisfaction with being cared for by Physicians Assistants (Anaesthesia), Paediatric Urology Day Case Surgery: A 5 year closed loop audit of length of stay, Can Regional Anaesthesia facilitate day case Mastectomy surgery? A quality improvement project, Does Intra-operative Cholangiography reduce the 28 day readmission rate following Day Case Laparoscopic Cholecystectomy, Reconfiguration of Anaesthetic Services at a Short Stay Satellite Unit to support and help relieve winter pressures and The Effect of Pre-Operative Pain on Day Surgery Outcomes. For me the delegates who, work on, write and present these prize papers are all winners in my eyes. Your work is on view for discussion and I am always grateful for your efforts and diligence with this work. You are all to be commended and especially the prize winners.

The next session was again interesting, thought provoking and a very real issue which started more debate between the delegates. The Post-Operative Carer: An Absolute or Relative Necessity? Drs Rachel Morris and Johannas Ratief were eloquent in their arguments and discussions. I had not previously considered this as an issue it was a proverbial ‘done deal’ for me but perhaps not anymore. Do fit and well patients require an inpatient bed due to not having a carer available at home? Social care and health care perhaps require further links but that is another discussion for another event. Over the years patients have been telephoned 24 hours post-operatively and have not answered. It is suspected some were out and about perhaps even shopping and taking part in their normal daily routine. Perhaps no need for a carer for 24 hours. That said I have my own views in relation to the more complex surgery now being managed on a day case basis. Indeed a cost saving could be had here. However what price safety? That said I am not sure that I would require a carer for 24 hours post-surgery, dependent upon the type and complexity of the surgery I required. Interesting and continuing debate for another day and perhaps a future ASM.
Final session of the 2017 ASM was no less thought provoking and outstanding. Delivering a day Case Spinal Anaesthesia Service is an area to develop throughout day surgery. Drs Robert Erskine and Kim Russon and Ms Debbie Timms Day Surgery Matron. The session included Targeting your day case spinal to the surgical procedure, How to introduce the service to your Day Surgery Unit and What are the Matrons Dilemmas. The issues discussed were clear, how do you get this implemented in to practice? Choosing the key personnel who need to be convinced and won over, Surgeons, Anaesthetists, Managers, All day Unit Staff. How is this done? how long will it take? Targeting patients is also crucial to the effe3ctiveness of short acting spinal anaesthesia as is trust between the surgical and anaesthetic teams. This session was a terrific way to close the 2017 BADS ASM in Southport with yet more food for thought. I have no idea how I will process all the new ideas I have come away with.
My final thoughts are that the 2017 BADS ASM in Southport has been a great success, stimulating, eye opening, progressive and reflexive. I am astounded at the brilliant work taking place throughout the country and how many patients are benefitting from your knowledge and skill. I am eternally grateful to our speakers this year who have given us there time and effort. It was great to meet up with colleagues and friends again this year and to discuss current issues that everyone appear to be experiencing in difficult fiscal times in the NHS and the wider community. Finally with everything else said and we are all back at the clinical interface, caring for our patients and carers, I would just like to say I would be delighted to see you all in 2018 at the ASM in Sheffield.

Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6165/273-reflections.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse6

Helen Ball, Sue Hull, Anna Lipp, Helen Lloyd, David Ralphs, Jill Solly
Sandra Meaden’s nursing career was committed to the development of day surgery and she achieved a huge amount both locally in Norwich and nationally through her role as a Council member and treasurer for the British Association of Day Surgery and as a founder member of the Royal College of Nursing Day Surgery Forum.
Sandra’s first achievement was the opening of the short stay ward at the old Norfolk and Norwich hospital, Claxton ward. Following that success, she was appointed as Day Procedure Unit Nurse Manager and together with David Ralphs the Director of Day Surgery, was a key figure in the commissioning and subsequent running of the first Arthur South Day Procedure Unit which was a truly innovative unit and fore runner of many of the day surgery units now in existence in nearly every hospital in UK.
Her experience in day surgery was recognised with her election as a Council member to the British Association of Day Surgery Council in 1995 and subsequently as Treasurer. Her colleagues in BADS remember her as always speaking from a wealth of experience, to be relied upon to deliver any project she was asked to undertake and as treasurer, an efficient and conscientious custodian of the Association’s finances. She was a delightful colleague retaining more than a hint of her Welsh roots and a whole-hearted participant in the Ceilidhs which were an integral part of the entertainment at BADS ASM in the past.
Sandra’s skills in management were continuing to develop and she became the service manager for DPU and plastic surgery and achieved an MBA in Business studies in 1997. She was actively involved in the planning and commissioning of the 6 theatre Arthur South day procedure unit at the new Norfolk and Norwich University Hospital. The fact that together these two units were awarded three Charter Marks over a 12-year period reflects Sandra’s ability to build around her a dedicated team that continued to provide excellent care. She was subsequently appointed as general manager for service improvement and inevitably the development of day surgery services remained a key focus. Sandra was always prepared to take on a new challenge, however difficult and give it her best shot, and her commitment to the introduction of Choose and Book in Norwich in 2001 was one such project.
Her final major project was to lead the rebuild and planning of the new Cromer Hospital on the Norfolk coast between 2003 and 2012. She worked closely with the operational team, architects and the construction company spending hours planning and developing existing and new services that would be suitable for transfer into the new day case facility. Under her leadership services such as pain management, simple chemotherapy, laser varicose vein treatments and one stop urology sessions were introduced in the new Cromer hospital. They ensured treatment closer to home for patients and expanded the remit of day surgery treatments. In the first three years, the new Cromer hospital saw a large increase in day procedure treatments for patients - treating its 500,000th patient in autumn of 2015. Sandra's expertise and determination to make the hospital visit for patients a smooth and efficient experience was evident throughout this period. Despite many challenges during the rebuild of Cromer hospital including withdrawal of additional funding, possible listed building status and the bat preservation trust, Sandra kept the teams focus on the task in hand and promised that she would not begin her (well deserved) retirement until the new Cromer hospital opened. The new hospital opened finally on 20 March 2012 and Sandra retired on 31 March 2012 - her vision achieved. After her retirement, she continued to contribute with her work for the Friends of the Hospital.
Colleagues who worked with Sandra for many years recall her as a very lovely, strong willed lady, who led by example and never appeared daunted by the challenges of working in the NHS. She instilled her interest in day surgery in many of those she worked with, including many of the current staff in DPU in Norwich. She inspired and more importantly, encouraged people to look inwards, enabling them to reach their full potential; she believed in her staff and fought for her beliefs.
We feel so lucky to have known and worked with Sandra and I am sure she would be very happy for us to raise a glass (or two) in her memory and to celebrate all she achieved, especially the continuing development of the day surgery services in Norwich and the DPU team which she established in 1991.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6162/273-sandra.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse7
Dr Steven Moore Consultant in Emergency Medicine, Countess of Chester Hospital, UK.
Health informatics – the discipline that brings clinicians and information technologists together – has an important role to play in almost all aspects of surgical care. Its value in day case surgery lies in supporting processes to ensure clinical safety and efficiency within the framework of high caseload wherein might lie unanticipated clinical risk. In preoperative assessment, it is important for practitioners to be able to access reliable medical data such as contemporaneous medication records, allergies and comorbidities. This can be achieved through systems such as the National Summary Care Record or more bespoke local solutions such as the Cheshire Care Record, providing more detailed records concerning other care providers. New tools are being developed to facilitate effective informed consent with web based systems allowing patients more time to digest and understand treatment options. Clinical documentation, as the NHS looks to a digital future, will be subject to various internationally recognised coding systems, such as SNOMED CT, ICD-10 and OPCS v4.x Such coded data will support business and clinical intelligence systems in analysing outcomes as well as developing more accurate costing data allowing more accurate remuneration. Informatics work can also support new ways of working with particular regard to patient and equipment tracking. A number of suppliers are now offering tools to follow patients, equipment and prostheses using standardised bar codes and RFID technology. Clinical correspondence can be supported by all the above if data is collected and stored in formats that allow export into Primary care systems without the need for further data entry. The delivery of informatics supported process change requires clinical leadership – the appointment of a Chief Clinical Information Officer within each health care organisation will enable clinical engagement in new systems development from the outset, to ensure that benefits are properly realised in the clinical workplace. The Wachter Report has set out the infrastructure required to develop a cohort of clinicians in this role.
(Click on image to go to the company website.)
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6164/273-health-informatics.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse8
Dr Darren Leech Director, NHS Elect
At the BADS conference this year, ambulatory care in surgery was a hot topic1. It is increasingly recognised that safeguarding an effective and efficient ambulatory care service - both medical and surgical - is a key step towards any hospital ensuring sustainable patient flow for urgent and emergency care patients2.
With an updated directory of ambulatory sensitive emergency conditions3, an ambulatory model of care is something that many hospitals are currently looking to introduce, or to develop further.
Clinical teams already running ambulatory care services have previously cited the ‘invasion and closure’ of their units as a risk to service continuity and quality. Typically, a depressing pattern of overnight invasion and incremental retreat the following day occurs. Of course, all hospitals face ‘peaks and troughs’ in demand, on a fairly predictable basis. Operationally, clear plans are needed to deal ‘everyday business’ along with ‘escalation plans’ for situations where demand and flow conspire to cause problems. Of course, clinicians need to influence both ‘everyday business’ and the process of escalation by engaging in the design and review of policy and practice at their hospitals.
Clinicians determined to ‘protect’ precious ambulatory care areas may be interested in a series of practical design ‘tips’ for the built environment, developed by the Ambulatory Emergency Care (AEC) network4. Derived from experiences across a broad range of hospital sites, the primary objective of these straightforward measures is to help safeguard the provision of ambulatory emergency care and in doing so, support the effective flow of emergency patients in hospitals.
The design ‘tips’ are as follows;
- Use recliner chairs and trolleys, not beds (the greater the proportion of chairs, the better)
- Ensure any space designated for a chair or trolley space, is smaller than that required for a hospital bed
- Reduce the width of access doorways, to allow the safe entry and exit of mobile, wheelchair and trolley bound patients but not those in hospital beds
- Use partial partitions, not curtains and remove curtain tracking
- Use clinic rooms for consultation and examination wherever possible, to maintain privacy and dignity
- Ensure that lighting is configured in such a way that all lights are either ‘off’ or ‘on’ - preventing the use of dimmers or zoned lighting commonly used in areas where patients sleep
- Aim for open plan design, ensuring ambulatory care areas are as flexible as possible in terms of the location and ratio of chairs and trolleys
- Restrict key-holding wherever possible
- Decorate (or redecorate) the area in the style of a clinic, not a ward - for example look at Dialysis or Macmillan Units
- Create a clear external AEC Unit entrance that is well signposted
- If possible, avoid connecting thoroughfares from/to wards and wherever possible, corridors through which beds are routinely transported
- Use cylinders for medical gas supply rather than piped gases
- Remove dedicated kitchen areas (vending perhaps, as per clinic design – remember, it is not a ward)
- Think carefully about toilet configuration and privacy and dignity requirements for an ambulatory unit - people will be dressed, unlike requirements for bedded single sex inpatient areas
It is recognised of course that hospitals will often be creatively adapting clinical or non-clinical space when developing or expanding ambulatory care services and each hospital site is different. That said, it is still recommended that as many of these practical design features are adopted, wherever possible. For new units, there is obviously a greater opportunity to design these features in, at the outset.
Architects and estates professionals have no authoritative guidance on how to design an ambulatory care facility, having only guidance for A&E or Ward areas to adapt. This can also lead to problems when new units are commissioned for what is still a relatively new concept for the NHS. The AEC network is currently working with the Department of Health to promote the development of a ‘Hospital Building Note’ (HBN) specific to ambulatory care environments - in the meantime, it is hoped that these practical measures might help.
References
- BADS – 28th Annual Scientific Meeting & Exhibition, 23rd & 24th June 2017
- Transforming urgent and emergency care services in England. Safer, Faster, Better: good practice in delivering urgent and emergency care. A guide for local health and social care communities. Department of Health, August 2015
- Directory of Ambulatory Emergency Care for Adults (5th Edit). Ambulatory Emergency Care Network, August 2016
- www.ambulatoryemergencycare.org.uk
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6159/273-environmental.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1148#collapse10