Dave Bunting
Dave Bunting
This edition of JODS follows the very successful Annual Scientific Meeting (ASM) held in June at the Sheffield City Hall. As promised all abstracts presented whether in poster or oral format are published in this edition of the Journal and are citable as peer-reviewed abstract publications. Feedback from the meeting was very positive, the overall programme content was rated as good or excellent by 93% attendees, overall timetabling was rated as good/excellent in 95% and the venue was rated as good/excellent in 94%. Preparations are well underway for next year’s ASM, which is to be held at the Royal Society of Medicine in London.
Since introduction of the application and web-based platforms last year, The Journal of One-Day Surgery is continually striving to improve the service it provides to its subscribers, to increase the accessibility of articles and to enhance the functionality of its electronic platforms. This month brings a new and important development whereby individual articles are available to view and download in PDF format, directly from the JODS app and JODS section of the BADS website.
This edition of JODS features full manuscript publications from work presented at the ASM this year. They include an audit of operation note documentation comparing practice with guidelines issued by the Royal College of Surgeons; a report of a single unit’s experience in ureteroscopy and lasertripsy for renal stone management; a service evaluation of major ear surgery performed as a day surgery and a study on the factors associated with successful day case tonsillectomy.
NHS England’s monthly performance statistics have this month shown that the number of patients waiting over a year for planned treatment has reached the highest level in over 6 years. Planning guidance issued by NHS England suggests that the number of patients waiting more than 52 months for treatment should be halved by next year and eliminated where possible, however, it seems unlikely that this will be achievable in many trusts. Maintaining highly productive day-surgery units is vitally important in helping to achieve these targets by reducing elective waiting times, especially as the majority of patients waiting over a year will be suitable for day surgery procedures.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6003/editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1287#collapse0
 Mary Stocker
Mary Stocker
I am sure like myself many of you are enjoying the last few days of a long glorious summer and preparing for the beginning of new academic terms and the return of some normality to the routine of home and work. As I look back over the summer the highlight for BADS was our Annual Scientific Meeting held this year in the lovely city of Sheffield. This was our first visit to Sheffield as a society and one we are very likely to repeat. The success of the meeting was a tribute to our Conference Secretaries Kim Russon and Fiona Belfield, along with our Honorary Secretary Paul Rawlings and of course Nicola Adams and Janet Mills. Huge thanks to this team who provided us with such an outstanding conference but also to all our members who submitted abstracts, posters and oral presentations and came to Sheffield in such great numbers and with such enthusiasm. It was so lovely to once again have a conference with large delegate numbers and such enthusiastic participation from all who attended. The details of the meeting are to be found elsewhere in the Journal but with day surgery neurosurgery last year, day surgery hip and knee replacements this year I really am left thinking will there be any elective inpatient activity left at all in a few years’ time. The ever-increasing expansion of the day surgery repertoire is a real tribute to those of you who work up and down the country to bring the day surgery agenda to the forefront of your trusts attention and to develop ever improved pathways of care for your day surgery patients, such that it is no longer inconceivable to be approaching such major surgery on a day case basis.
Looking forward to the new year for BADS I am delighted to announce some new appointments to council and some new officer roles. We welcome Alex Alen, Jan Howells-Johnson and Sandra Briggs to full members of council having all been co-opted council members for the last 12 months. All three bring nursing expertise to our ranks. We are also delighted to welcome Dave Bunting our to full council membership. Dave was previously a representative of the Association of Surgeons in Training (ASIT), however after securing an consultant surgeon position he was no longer eligible to remain in that role and we are delighted to have him as a full council member.
We will also see some changes in the societies officers this year. I am delighted to announce that Kim Russon will be succeeding me as President of the Society in June next year. Theresa Hinde is taking over from Paul Rawlings as Honorary Secretary and Jo Marsden joins Kim Russon and Fiona Belfield within the conference planning team.
If you were unable to join us in Sheffield or even if you were there and would like to hear more about day surgery hip and knee replacement surgery we will be running a joint conference with Healthcare Conferences in London on September 20th. Details are on the website for what looks to be a very useful day, do come along. Other developments on the horizon include the imminent launch of the model hospitals day surgery benchmarking compartment details will be on the BADS website as soon as this is available.
We are still trying to update our list of contacts for day surgery teams up and down the country so please e-mail the office if you have details of the lead medic and nurse for your day surgery unit. We look forward to hearing from you.
Finally do put the dates of our 30th Anniversary meeting at the Royal Society of Medicine in your dairy now – we hope to see you there!
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6005/presidents-letter.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1287#collapse1
Authors
William A Butterworth (Core Surgical Trainee, Princess Royal University Hospital, Bromley).
Rahul Lunawat (Consultant Urologist, Princess Royal University Hospital, Bromley)
Corresponding Author Address
William A Butterworth Flat 18 Rhodes Court. 5 Jefferson Place. Bromley BR2 9FY.
Abstract
Introduction: Incidence of renal stones is increasing worldwide and varies from 58 to 900 per 100,000, with a 9% lifetime risk of having renal stone related symptoms. Increasingly ureteroscopy (URS) coupled with laser fragmentation is being used safely within the day surgery setting for ureteral and renal stone management, with associated high stone-free levels and patient satisfaction. This audit set out to explore whether URS guided lithotripsy could be delivered effectively as a day surgery procedure within the District General Hospital (DGH) setting.
Method: Retrospective analysis of seventy seven (n = 77) day surgery patients who underwent URS guided lasertripsy for ureteric and renal calculi in a DGH between November 2016 – November 2017. All patients underwent ureteric stenting prior to the URS guided lithotripsy. Outcomes were compared against European Association of Urology (EAU) guidelines on the best clinical practice in use of URS in urolithiasis.
Results: Of the 77 patients who underwent URS and laser fragmentation, the average patient age was 54 years and there was a 2:1 male:female ratio. The total number of stones treated in all patients was 94. Of stones treated, 62% were ureteric (67% upper, 8% middle and 25% distal ureter), and 38% renal (11% upper pole, 22% middle pole and 67% lower pole). Average renal stone size was 8.9mm, with 64% ‹1cm, 36% 1-2cm and 0% ›2cm. The average ureteric stone size was 9.5mm, with 70% ‹1cm, 26% 1-2cm and 4% ›2cm. The average number of stones treated per case was 1.3, with an average 0.989 Watts of energy used. 88.3% of patients following URS guided stone fragmentation were stone-free. There was a 1.3% additional procedure rate, with one re-do URS and lasertripsy performed. The complication rate was 6.5% (n = 6), with only 2.6% (n=2) patients requiring admission for post-operative pain management.
Conclusion: The increasing prevalence of renal stones globally, associated with factors such as dietary changes and global warming, emphasises the need to develop effective management strategies. This audit demonstrated that URS guided stone fragmentation can safely deliver high stone free and low complication rates within the DGH setting.
Introduction
The worldwide incidence of renal stones (RS) varies from 58 - 900 per 100,000, whilst the UK lifetime prevalence of renal stone disease is 13% (1,2). There has been a significant worldwide increase in RS incidence over the past 15 years, which has been linked with an ageing population, higher levels of obesity and diabetes, plus environmental factors such as dietary and climate change (1). This has translated into a 70% increase in UK hospital attendances with RS, from 51,035 attendances in 2000 to 86,742 in 2015 (2). This increased RS disease burden and hospital attendance has seen RS treatment increase disproportionately compared to other urological activity; with ureteroscopy (URS) guided lasertripsy being performed more frequently than cystectomy, nephrectomy and radical prostatectomy combined (3). Although there are European guidelines for the ureteroscopic management of RS, this audit has looked to address that there is little published evidence demonstrating the safety and efficacy of URS lasertripy within district general hospital setting (4).
Methods
Retrospective analysis of seventy seven (n = 77) day surgery patients who underwent URS guided lasertripsy for ureteric and renal calculi in a DGH between November 2016 – November 2017. All patients underwent ureteric stenting prior to the URS guided lithotripsy. Outcomes were compared against European Association of Urology (EAU) guidelines on the best clinical practice in use of URS in urolithiasis.
Results
Of the 77 patients who underwent URS lasertripsy, the average patient age was 54 years and there was a 2:1 male:female ratio. he total number of stones treated was 94, of which 62% were ureteric (67% upper, 8% middle and 25% distal ureter, and 38% renal (11% upper pole, 22% middle pole and 67% lower pole). The average ureteric stone size was 9.5mm, with 70% <1cm, 26% 1-2cm and 4% >2cm. The average renal stone size was 8.9mm, with 64% <1cm, 36% 1-2cm and 0% >2cm. All renal stones treated via URS lithotripsy were ˂2cm, which is in compliance with EAU guidelines that Percutaneous Stone Removal (PSR) should be first line for renal stones >2cm. Also in accordance with the EAU guidelines, all cases were undertaken with the use of a holmium laser and placement of safety wire or ureteral access sheath. he average patient stone burden was 12.1mm. The average number of stones treated per case being 1.3, with an average 0.989 Watts of energy used. At three month follow up clinic, 88% of patients following day surgery URS lasertripsy were found to be stone-free on abdominal X-ray (AXR). Of the 12% of patients who were not stone-free at this 3 month follow up, only one re-do URS lasertripsy was performed; with the other patients successfully passing their residual fragments after a further 3 month period of surveillance. The re-do URS was required due to an inaccessible ureter despite the use of guidewires/access sheaths; and was successfully performed two months later with a stone-free outcome. The complication rate was 6.5% which was below the acceptable complication rate of 9-25% stated by the EAU guidelines. The Clavian Dindo classification of these complications would be 2 x(I), 2x(II), 1x(IIIb); including two patients requiring overnight admissions for analgesia, two patients representing and requiring intravenous antibiotics for post-operative urosepsis and one patient requiring a re-do URS.
Discussion
The surgical management of RS can be dictated by several factors including stone size and location, as well as patient preference plus available local facilities and expertise (2). The management of RS has gravitated towards minimally invasive interventions such as Shock Wave Lithotripsy (SWL), URS Lasertripsy and Percutaneous Stone Removal (PSR) (5,6). This can be largely attributed to the vastly improved morbidity and complication rates associated with these modern endourological procedures (7). The number of URS lasertripsies performed in the UK has increased by 127% over the past 10 years, with 14,242 cases in 2015 compared to only 6283 in 2000 (3,5). There was also a 55% increase in the number of SWL cases performed, and a 149% increase in PSR (3,6). The inverse pattern has been observed in open surgery for RS, with an 83% decrease from 278 cases in 2000 to only 47 cases in 2010 (3).
The increasing use of URS lasertripsy can be accounted for by the technological advancements made in optics and endoscope miniaturisation, allowing URS to be performed quicker and more efficiently with improved stone free rates (SFR) (4). Furthermore, the progression from electrohydraulic and ultrasonic lithotripsy to Holmium lasertripsy has seen a reduction in ureteral injuries and increased efficiency in fragmentation of all stone compositions (8).
URS is being utilised in both standard RS patients but also increasingly in complex stone disease and patients with complicating comorbidites such as obesity, bleeding diathesis, pregnancy and solitary kidney (5).
Conclusion
URS lasertripsy achieves high SFR and low rates of additional procedures, however has been associated with high complication rate in the past (9). This audit however has demonstrated how URS lasertripsy is increasingly achieving higher SFR (88%) and lower levels of re-do procedures (1.3%); whilst maintaining an acceptably low complication rate (6.5%). This audit demonstrated that URS guided stone fragmentation can safely deliver high stone free and low complication rates within the DGH setting.
References
- Romero V. Akpinar H. Kidney Stones: A Global Picture of Prevalence, Incidence, and Associated Risk Factors. Reviews in Urology. 2010. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2931286/
- Renal and ureteric stones: assessment and 5 management. NICE England. Feb 2017. URL: https://www.nice.org.uk/guidance/gid-ng10033/documents/final-scope
- Turney B, Noble J. Trends in urological disease. BJU international. August 2011. URL: https://www.researchgate.net/publication/51612180_Trends_in_urological_disease.
- Turk C, Knoll T, Petrik A. Guidelines on Urolithiasis. European Association of Urology. 2015. URL: http://uroweb.org/wpcontent/uploads/22-Urolithiasis_LR_full.pdf.
- Ho A, Sarmah P. Ureteroscopy for stone disease: expanding roles in the modern era. Central European Journal of Urology. 2017. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5510346/
- Rukin N, Siddiqui Z. Trends in Upper Tract Stone Disease in England: Evidence from the Hospital Episodes Statistics Database. Urology internationalis. URL: https://www.ncbi.nlm.nih.gov/pubmed/27694759.
- Cui, X., et al. Comparison between extracorporeal shock wave lithotripsy and ureteroscopic lithotripsy for treating large proximal ureteral stones: a meta-analysis. Urology, 2015.
- MacLennan S., et al. What are the benefits and harms of ureteroscopy (URS) compared with shock wave lithotripsy (SWL) in the treatment of upper ureteral stones in children and adults? PROSPERO International prospective register of systematic reviews, 2015. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015023769
- Hong, Y.K., et al. Ureteroscopic lithotripsy using Swiss Lithoclast for treatment of ureteral calculi: 12-years experience. J Korean Med Sci, 2009.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6006/butterworth.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1287#collapse2
Author:
Dr Natalie Smith Torbay and Southern Devon NHS Trust, Torbay Hospital, Torbay, United Kingdom
Dr Jane Montgomery, Consultant Aneasthetist, Torbay and Southern Devon NHS Trust, Torbay Hospital, Torbay, United Kingdom
Abstract
Introduction: The British Association of Day Surgery (BADS) has national recommendations for the percentage of operations which could be day case. Over the last 10 years the recommended rates for major ear surgery have increased. In 2007 suggested day surgery rate for mastoid surgery was 0% this is now 70%1. We audited our day surgery rates for major ear operations against current recommendations and assessed outcomes including post-operative pain, nausea scores, unplanned admissions and patient satisfaction.
Method: Using electronic record systems, we identified all patients who had primary tympanic, stapes and mastoid surgeries between January 2013 and July 2017.
Results: 202 patients underwent major ear surgery. We have been above the BADS recommended day surgery rates in all groups since 2014. There were 2 unplanned admissions, for pain and dizziness. Reports of mild post-operative pain were comparable across all procedures and years. Most patients had no post-operative nausea or dizziness. 6% of patients complained of mild post-operative nausea and only one patient reported moderate dizziness. All patients would recommend our unit, being satisfied or very satisfied with their experience.
Conclusion: We have demonstrated excellent outcomes for these patients and will continue to offer a day surgery pathway as the norm for the majority of patients.
Introduction
Torbay Hospital in Torbay and South Devon NHS Trust, has a purpose-built day surgery unit. The number of operations completed as day surgery is increasing, currently operating on over 9000 cases per annum (2). The British Association of Day Surgery (BADS) has national recommendations for the percentage of operations which could be day case. Over the last 10 years the recommended rates for major ear surgery have increased. In 2007 suggested day surgery rate for mastoid surgery was 0% this is now 70% (1). We wanted to know how we are doing against the BADS recommendation and how we compare to the rest of the country. We audited our day surgery rates for major ear operations, primary mastoid, tympanic and stapes procedures between January 2013 and July 2017. We also assessed secondary outcomes including post-operative pain, nausea scores, unplanned admissions and patient satisfaction.
Method
Patients were identified using Torbay Hospital’s electronic record system. This system is used to collect all individual data. All patients are telephoned on the first post operative day and answer a semi structured questionnaire about post operative symptoms and their satisfaction with our service. Using this electronic record all patients having primary major ear surgery between January 2013 and July 2017 could be identified. This group was divided according to their primary operative code for further analysis.
Our primary outcome measure was the day surgery rate for each procedure. The yearly rates were reviewed to assess for any improvement during the study period.
Secondary outcome measures of unexpected admission and post-operative complications were reviewed according to primary procedure and year of completion.
Article continues after ad.
Results
During the study period January 2013 to July 2017 our unit completed 83 primary tympanic procedures, 73 primary mastoid procedures and 46 primary stapedectomy procedures. A total of 202 primary major ear procedures.
Primary outcomes
BADS Directory of Procedures recommends the percentage of each operation that should be completed as day surgery (1). They also produce a table of how each the top 5%, 25% and 50% of hospitals are performing for each procedure (4).
BADS recommends that 70% of all primary mastoid surgery is completed as day surgery (1). During the study period we completed between 5 and 18 primary mastoid surgeries per year. Initially, in 2013 our hospital was completing 71% of cases as day surgery increasing to 100% in 2017.
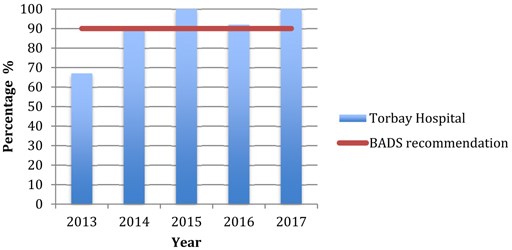
Our hospital completes between 3 and 13 primary stapes surgeries every year. BADS recommends 90% to these to be completed as day surgery (1). Our hospital has been achieving this since 2014.
Completing all primary tympanic surgery as day surgery since 2013 our hospital is significantly better than the BADS recommendation of 95% as day surgery (1). Our hospital completed more than the recommended as day surgery despite the number of cases doubling per annum during the study period.
FIGURE 1: Percentage of Primary Mastoid Procedures completed as day surgery.
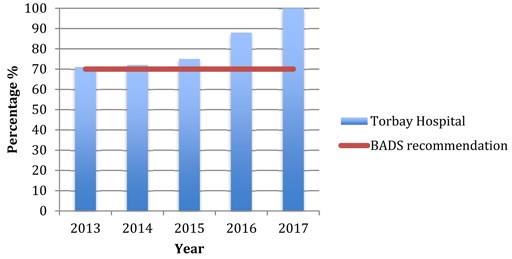
FIGURE 2: Percentage of Primary Tympanic Procedures completed as day surgery.
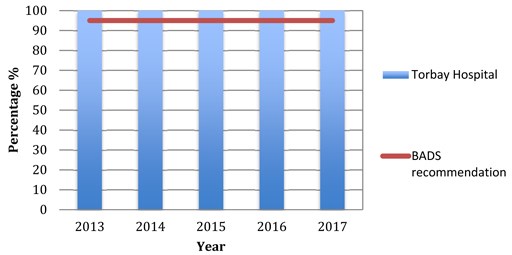
FIGURE 3: Percentage of Primary Stapes Procedures completed as day surgery.
Secondary outcomes
We were unable to contact 20% of patients on day one post operatively so can not report the secondary outcomes for these patients
Post operative complications such as nausea, dizziness and pain whilst usually innocuous can be very distressing for patients and affect their whole experience.
Nausea and vomiting is a complication that patients often worry about, with procedures on the ear increasing the patients’ risk. Postoperative nausea and vomiting was a rare complication, the numbers in this study are very small. We found that the vast majority of patients across all procedures reported no nausea or vomiting. No patient in the study reported severe symptoms. With the patients having Stapes or mastoid procedures no one complained of moderate symptoms with approximately one patient per year reporting mild symptoms. The patients having tympanic procedures had the highest reported severity of nausea with two cases experiencing moderate symptoms. These patients did not require admission.
Post-operative reports of pain varied between types of surgery. Mastoid and tympanic procedures reported more pain than patients having stapes procedures. Of the patients having stapes procedures a third reported mild pain but no one reported moderate or severe during the study period. Both tympanic and mastoid procedures have some cases which reported moderate pain, with one patient who had a mastoid procedure requiring admission.
Any patient having an operation on their inner ear is at risk of dizziness postoperatively. We found that mild dizziness following any major ear procedure was frequent but more severe symptoms were rare. In this study only one patient reported moderate dizziness following a mastoid procedure in 2014. This patient did not require admission.
Information is given to all of our patients on discharge on how to contact help if needed. They are given the units contact details as well as out of hours services. During the study period only one patient contracted the day surgery unit after discharge. This was for advice only and didn’t require any medical intervention.
Unexpected admission rates are important as it can highlight a problem with the service. We have had two unexpected admissions during this study. A stapedectomy patient was admitted due to dizziness and a mastoid patient for pain. Both patients were admitted in 2016.
Discussion
British Association of Day Surgery produce a dataset along side the directory of procedures. This shows the percentage of each of procedure being completed as day surgery by the top 5%, 25% and 50% of hospitals in the country (4). Using this data set we could review our own progress.
From the data 50% of hospitals are completing 27% or more of their primary mastoid procedure as day surgery and the top 5% completing over 85% as day surgery (4). Our hospital has shown significant improvement over the study period now being in the top 5% in the country. The top 5% of hospitals are completing 100% of primary stapes procedures as day surgery4, our hospital is in this group having completed all the cases as day surgery since 2015. Similarly the top 5% of hospitals are completing all of their primary tympanic procedures as day surgery. Like the other procedures our hospital is in the top 5%. Being in the top 5% nationally for all primary major ear procedures is a great success for our unit.
Acute postoperative pain is one of the most common forms of acute pain (3). Our hospital has guidance for peri-operative analgesia according to operation type. During the study we only had one patient admitted due to pain and only a few reporting moderate symptoms. This shows that the analgesia prescribed peri-operatively is suitable for the majority of patients.
As part of continuing improvement all patients are asked post discharge if they are satisfied with the service they received and whether they would recommend our day surgery unit. All patients in this study would recommend our day surgery unit. The patient satisfaction documentation support this will documentation says patients were either very satisfied or satisfied with our unit.
Our audit has shown that we were unable to contact 20% of our patients on day one post operatively. We are unsure why this is such a high percentage. Patients are contacted using the telephone number supplied by the patient pre-operatively. This system needs to be reviewed to reduce the number of uncontactable patients to ensure their safety and to allow completion of hospital journey paperwork for auditing.
Conclusion
We are meeting all of BADS recommendations for major ear procedure being completed as day surgery. Nationally we are in the top 5% of all hospitals for major primary mastoid, tympanic and stapes procedures. Although the numbers are too small for statistical analysis we can see that the occurrence of postoperative complications is low. We need to continuously review our service to maintain this high standard of care and meet the BADS recommendations.
References
- British Association of Day Surgery BADS Directory of Procedures 5th Published June 2016.
- torbayandsouthdevon.nhs.uk/services/day-surgery-unit
- Carr DB, Goudas LC, Acute pain, Lancet 1999:353;2051-8
- British Association of Day Surgery BADS Directory of Procedures National Dataset (Calendar Year 2015)
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6008/smith.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1287#collapse3
Authors
Dr William Ward FY1 Doctor
Email: will.ward@nhs.net
Mr David Bunting Consultant Upper GI Surgeon
Email: davidbunting@nhs.net
Abstract
Introduction: All patients undergoing a surgical procedure in the UK should have documentation of the operative details in the medical notes. The Royal College of Surgeons of England (RCSEng) “Good Surgical Practice” document details 21 standards that should be met. This audit aimed to measure how accurately these guidelines are followed in our trust within a defined patient group.
Methods: We identified all patients undergoing day-case laparoscopic cholecystectomy between 1.11.2017 and 31.11.2017 from the electronic operative database ‘Theatreman’. Operative records filed in the patient notes were analysed to see how many of the 21 criteria described in the ‘Good Surgical Practice’ document were adhered to. For each criterion, adherence was deemed good if met in >50% patients and was deemed poor if met in <50% patients.
Results: 29 patients were identified. One set of notes could not be obtained, leaving 28 for the final analysis. One criterion was deemed not applicable in this patient group leaving 20 criteria against which we measured our performance. Adherence to the 20 criteria was deemed excellent in 9 (45%); good in 6 (30%) and poor in 5 (25%).
Conclusions: Standards for operative note documentation are not being consistently met. Results were presented to the departmental clinical governance meeting. The authors made the following recommendations and planned to perform a re-audit in 6 months’ time.
- all notes should be typed on a proforma that includes all RCSEng guidelines
- all surgeons should familiarise themselves with RCSEng guidelines
- a laminated copy of the guidelines should be displayed in every theatre.
Introduction
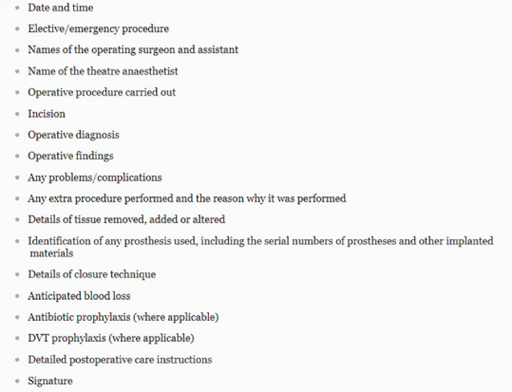
All patients undergoing a surgical procedure in the UK should have documentation of the operative details in the medical notes. The Royal College of Surgeons of England (RCSEng) “Good Surgical Practice” document details a number of standards/criteria that should be met (1), see Figure 1.
FIGURE 1: Criteria recommended by the Royal College of Surgeons of England for documentation in the operative note.
At North Devon District Hospital (NDDH), headed paper with a coloured corner tab is used to document the operative note. These proformas include headings such as ‘date’, ‘surgeon name’ and ‘anaesthetist’. They don’t, however, include headings for every detail that should be included. It has been observed that there is a wide variation in the standard of detail recorded in operative notes. This audit aimed to measure how accurately the guidelines are followed in our day-surgery unit within a defined patient group.
Methods
We identified all patients undergoing day-case laparoscopic cholecystectomy (Operation Procedure Code J18) between 1.11.2017 and 31.11.2017 from the electronic operative database ‘Theatreman. Approval was gained from the local Clinical Audit and Effectiveness department. Operative records filed in the patient notes were analysed to see how many of the criteria described in the ‘Good Surgical Practice’ document, were adhered to. The document lists 18 criteria (Table 1), however, it also states in separate text the importance of including patients’ details and notes being legible. In addition, we separated documentation of date and time, creating a total of 21 criteria to measure against. For each criterion, adherence was deemed excellent if met in 100% cases, good if met in >50% patients and poor if met in <50% patients. Results were tabulated and a cumulative score for each individual criterion was calculated. This enabled an analysis of performance against each of the recognized criteria in the guideline.
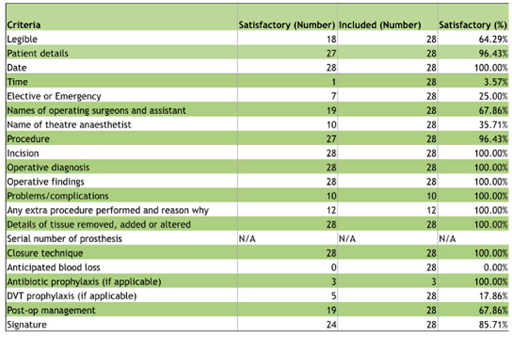
TABLE 1: Compliance of operative note records with guidelines for documentation of 21 criteria defined in the
Royal College of Surgeons of England ‘Good Surgical Practice’ document.
Results
A total of 29 patients identified from the database. One set of notes could not be obtained, leaving a sample size of 28 for the final analysis.
The operation we audited (laparoscopic cholecystectomy) does not require the insertion of any prosthetic material, therefore, the inclusion of this criterion was deemed not applicable for the purposes of this audit, leaving 20 audit standards to measure against, see Figure 2.
FIGURE 2: Proportion of operative note records (as percentage) compliant with guidelines for documentation of
21 criteria defined in the Royal College of Surgeons of England ‘Good Surgical Practice’ document.
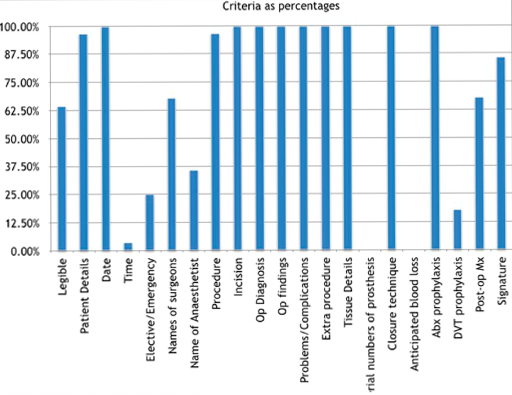
Of the 20 recommendations, adherence was deemed excellent in 9 (45%). These included date, incision, operative diagnosis, findings, problems/complications, extra procedures, closure technique, antibiotic prophylaxis, and details of tissue added, removed or altered. Adherence was good in 6 criteria (30%). These include legibility, patient details, names of surgeon and assistant, procedure, post-op management, and signature. Adherence was deemed poor in 5 criteria (25%). These were: documentation of time of day, elective or emergency status, name of theatre anaesthetist, anticipated blood loss, and DVT prophylaxis. Time of day and anticipated blood loss were particularly poorly documented with inclusion in 4% and 0% records respectively. No operative notes were compliant with all criteria.
Article continues after ad.
Discussion
This audit comparing the standard of documentation in operative notes with national guidelines showed adherence to guidelines was suboptimal for most criteria measured. No operative records were 100% compliant. Notable, those criteria that were particularly poorly documented, often did not have any heading on the proforma. Inclusion of these headings into the proforma would ensure better adherence to the guidelines. It was also noticed that there is a difference in headings on the standard operation note proforma and the day surgery operation note proforma. A universal proforma would help to improve documentation.
Typed notes demonstrated better adherence to the guidelines than handwritten notes. Types notes were used by individual surgeons having created their own templates. None of the typed notes, however, included a signature, rather the surgeon’s name was typed, which was deemed non-compliant with the guidelines.
With regards to legibility, our results may include error whereby some of the recommendations may have been included but illegible. Typed notes would eliminate this error.
Some criteria would only be included if required depending on particular operative factors such as the occurrence of any intraoperative complications. Where these are not stated it has been assumed no complication occurred and the documentation is accurate. It was noted that some surgeons documented specific details such as whether or not bile and/or stones were spilled during the procedure. It’s not clear whether the absence of such events should be specifically recorded, although this would ultimately be best practice and help with further auditing.
Quality improvement interventions
- Results have been presented to the directorate clinical governance meeting
- Laminated copies of the guidelines have been displayed in consultants’ offices and in each operating theatre
- Re-auditing is planned in 6 months.
Conclusions
This audit has shown that surgeons are frequently including the majority of the recommendations set out by the RCSEng for documentation of the operative note. However, there is significant room for improvement which could be achieved by adopting typing operation notes using a template with headings for each of the criteria recommended by the RCSEng. Similar results could be achieved by adopting the use of specific software applications used to generate operative notes based on templates, however, this is likely to require significant investment in computing hardware, software and training.
References
- Royal College of Surgeons of England (2014) Good Surgical Practice. Royal College of Surgeons of England. https://www.rcseng.ac.uk/-/media/files/rcs/standards-and-research/gsp/gsp-2014-web.pdf?la=en
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6009/ward.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1287#collapse5
Authors
John Guirguis Anatomy Demonstrator/Surgical Trust Doctor
Jonathan Hobson Consultant ENT Surgeon
Department of Otolaryngology, University Hospital of South Manchester
Contact details:
John Guirguis Newcastle University, Framlington Place NE2 4HH
Email: johnguirguis@doctors.org.uk
Keywords: Tonsillectomy, Adenotonsillectomy, Day, Day case, Surgery, Rate
Abstract
Aims: 85% of tonsillectomies should be completed as day case operations. This rate was 33% in the University Hospital of South Manchester (UHSM) in April 2015.This study will focus on identifying factors that could be contributing to this low rate, in order to decrease length of stay following tonsillectomy.
Methods: Tonsillectomies were accessed from April 2015, October 2014 and April 2014, with patient details recorded. The case notes were then requested and a pro forma made to include a variety of information regarding the patient and operation.
Results: A total of 62 patients had tonsillectomies completed across the 3 months of the study. 8 were not included. The day case rate was 31% in April 2015, 50% in October 2014, and 65% in April 2014. In total, 27 patients were managed as day cases (50%).
Patients under the age of 6 had a low day case rate of 29%. 68% of bilateral tonsillectomies were completed as day cases, in contrast to 21% of adenotonsillectomies.
64% of operations done in the morning were completed as day cases, in comparison to 22% performed in the afternoon. Operations done as day-case averaged 25.6 minutes, while overnight stay averaged 31.4 minutes. 10% of patients with sleep apnoea, and 20% of patients with complications, were managed as day cases.
Conclusion: The day case rate of tonsillectomies performed at UHSM are significantly below the required standards of 85%. Several contributing factors were identified: younger patients, afternoon operations, type of procedure (adeno-tonsillectomy), prolonged duration of surgery, sleep apnoea, and complications.
Introduction
Day surgery is best described as 'the admission of selected patients to hospital for a planned surgical procedure, returning home on the same day' (1).
The British Association of Day Surgery (BADS) has produced a Directory of Procedures recommended to be done as day-case operations, with over 200 operations covered (4). The desired day case rates of each procedure are also included - with tonsillectomies given a target rate of 85% (2,4). The figure below outlines the benefits of day surgery over an inpatient stay (3).
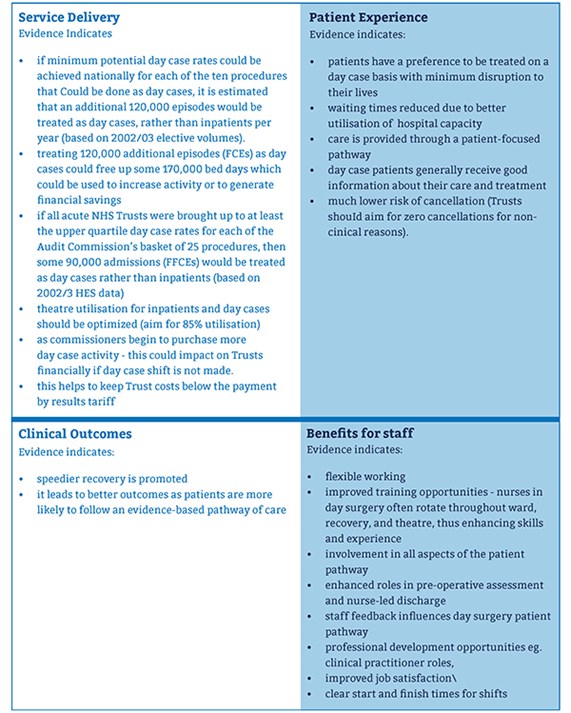
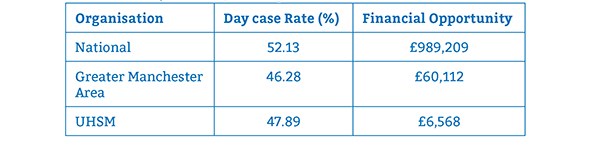
Table 1 shows the average day case rate of tonsillectomy across the UK, the Greater Manchester Area, and UHSM, over the year 2014/2015. As shown by the figures, each organisation is well below the 85% target rate, proving there is room for improvement. The financial opportunity indicates how much money could be saved if the trust(s) achieved a day case rate in line with the percentile for the top quarter of the year. If 85% was achieved, potentially even more could be saved for each organisation. £11,206 could be saved at UHSM if rates of 90% were achieved (2).
TABLE 1: The average day case rate of tonsillectomy across the Nation, the Greater Manchester Area, and
UHSM, over the year 2014/2015.
Tonsillectomy is one of the most common operations completed in the UK. Although the number of these procedures performed has decreased significantly since the 1930s - where 100,000 tonsillectomies were performed on school children, the incidence has started to rise again since the 1990s (5). In 2012, around 31,000 tonsillectomies were performed; 18,000 of these were done on children. This resulted in a cost of £51m across England. There is a lot of variation in the numbers across the UK (6). In the UK, there are more than 35 million work or school days lost annually (5).
The objective of this study is to look into decreasing the length of stay for patients who undergo tonsillectomy. Tonsillectomy should be done as a day case operation, meaning the patient should be discharged home on the same day of the surgery. The British Association of Day Surgery has set a target of 85% of tonsillectomies to be completed in this manner4. The day case rates in the University Hospital of South Manchester (UHSM) have dropped from 60% in April 2014 to 33% in April 2015.
To ascertain why this is the case, 3 separate months ranging from April 2014 to April 2015 will be looked at, focusing on how many tonsillectomies were completed and how many were managed as day case operations. This will allow clarification of these proportions and investigate why the rate has been falling.
Methods
Permission was given to access all the operations completed in ENT theatres on the computer. The procedures completed in the three months of the study were looked at; recording each tonsillectomy done, the date of the operation, and the name and hospital number of the patient receiving the surgery. Information was also collected regarding the surgeon and the duration of the surgery.
The search returned a total of 62 patients who underwent tonsillectomies over the three months - 16 patients from April 2015, 28 from October 2014, and 18 from April 2014. After recording the basic information of each operation, each individual patient was looked at in more detail to find out if the surgery was completed as a day case, and if any reasons were provided in the event of an inpatient stay.
In order to retrieve the patient cases, ENT secretaries kindly requested the data needed. The patient notes were then accessed and worked through one month at a time, recording a variety of fields relevant to the study. This information was maintained on a spreadsheet accordingly. The data kept note of is as follows:
- Demographics: age, gender, weight (kg), BMI
- First half of postcode
- Procedure (adeno- or tonsillectomy), any additional procedures
- Surgeon and duration of operation
- Details of operation: date, day, time
- Details of discharge: date, time
- Problems during/after operation (e.g. failure to pass urine)
- Relevant PMH
- Day case?
The information was analysed in each field in order to find out whether there was any association in a particular field with the procedure being completed as a day case. Each patient case was also analysed in detail to see if there was a specific reason for an overnight stay.
Some patient notes could not be acquired as they were being used for other reasons at the time. After recording the information required for each patient, 8 patients had still not been looked at - 3 for April 2015, 4 for October 2014, and 1 for April 2014. Unfortunately, we were unable to acquire the remaining patient cases over the duration of the study.
Descriptive statistics and demographics were reported as figures and percentages. Categorical variables were compared using Fisher's Exact Test with two-sided probability and Mann-Whitney U Test as appropriate, using Past3 (Palaeontologica Electronica, Oslo) statistical software for analysis. Significance was set at P<=0.05.
This method had both advantages and disadvantages. The advantages include:
- The hospital information required was achieved in reasonable time due to the electronic database of operations, and the kind help of the ENT secretaries.
- Low cost as data was collected within the hospital.
- The patient cases are well organised and allowed the information to be collected following the same pattern.
The disadvantages are:
- 8 patient details are missing for the report.
- Lack of documentation in some case notes.
Results
A total of 62 patients have had tonsillectomies over the 3 months of the study - 16 in April 2014, 28 in October 2014, and 18 in April 2014. Data is missing for 8 of the patients, therefore, the results will focus on 54 patients with the remaining 8 to be added at a later date.
As discussed earlier, a target of 85% of tonsillectomies should be completed as day cases. UHSM provided details of the falling day case rate at the hospital: 33% in April 2015, 50% in October 2014, and 60% in April 2014. Table 2 represents the number and percentage of procedures done as day cases. In total, 27 of the 54 operations were completed as day cases - 50%.
TABLE 2: Day surgery rates across the three months included in the study. Shown as numbers and percentages.
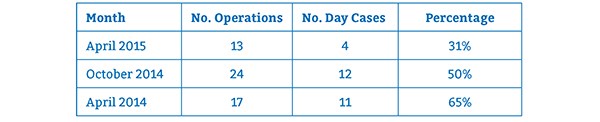
Table 3 considers the patient's age in relation to the day case rate. It demonstrates a high proportion of patients under the age of 6 were admitted and required inpatient stay. It is important to state that within the trust, day case operations are unsuitable for patients under 15kg in weight, or with BMI <5th or >95th percentiles. 4 patients from this age group were under 15kg and therefore unsuitable for day surgery. However, 1 was managed as a day case and went home the same day.
The day case rate increased at the 6-12-year-old group, but drops from 78% to 38% at the 12-18-year-old group. If considering all of the paediatric patients together (those under the age of 18), the day case rate was 42%, lower than the figure of 69% for adults.
TABLE 3: Day surgery rates across the three months included in the study. Shown as
numbers and percentages.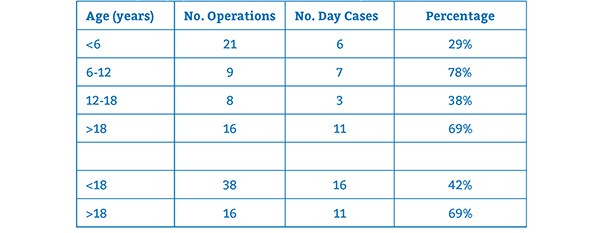
35 of the 54 tonsillectomies were performed on females, which resulted in 20 being completed as day cases (57%). From the remaining procedures done on males, 7 were day cases - a percentage of 37%.
Data was collected on the BMI and weight of each patient; however, this will not be discussed in this study. There was no connection between the postcode of the patient and day case rate at UHSM. Across each postcode area recorded: Manchester, Cheshire, Stockport, Warrington; there was a mixture of tonsillectomies completed as day cases and requiring inpatient stay.
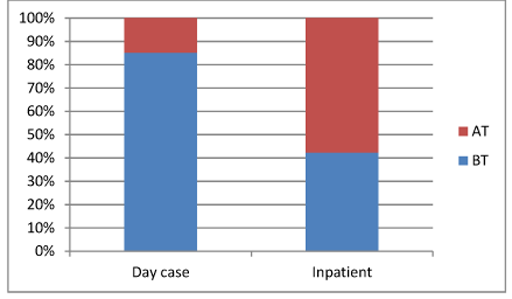
The results show that out of the 54 tonsillectomies performed, 34 were bilateral tonsillectomies (BT), 19 were adenotonsillectomies (AT), and one unilateral tonsillectomy was performed on the left side. Adenotonsillectomy is the same as a tonsillectomy with the addition of the adenoids (pharyngeal tonsils) extracted. Adenoidectomy and tonsillectomy are some of the most frequently performed operations suitable for day surgery, and are completed together in around one third of patients4,5.
Of the 34 bilateral tonsillectomies, 23 were completed as day cases - a percentage of 68%; however, just 4 adenotonsillectomies - 21% - were managed in this way. These variables were compared using Fisher's Exact Test with two-sided probability. The results represent a significant difference, with P value 0.002 (significance P<=0.05). The left tonsillectomy required admission, but this may have been due to a neck lump excision on the right side being completed at the same time.
Figure 2 shows the management of the two procedures weighed up against each other. The day case rate of BTs stands out against ATs.
FIGURE 2: The outcome of bilateral tonsillectomies (BT) against adenotonsillectomies (AT).
This shows the proportion of both operations done as day cases against the proportion that required
inpatient stay.
In some cases, additional procedures were also performed during the same anaesthetic for the tonsillectomy. These ranged from grommets to various endoscopies. 11 tonsillectomies had an extra procedure done. Only 3 of these were completed as day cases (27%). These patients were therefore more likely to be kept overnight.
It was difficult to draw any conclusions on day surgery rates relating to the operating surgeon. The numbers being discussed for each surgeon were generally too few to be reliable. The majority of operation notes state for the patient to go home the same day if well.
The duration of operation for patients managed as day cases and those managed as inpatients was considered. The average duration for day case operations was 25.58 minutes, while operations that resulted in overnight stay averaged 31.44 minutes. Every operation performed was listed and ranked within the two groups and compared using a Mann-Whitney U Test. This provided a z score of -0.99 and a P value of 0.32 (significance P<=0.05), showing no significant difference in day case rate according to the operation time.
In order to find out if the timing of the operation affected the day case rate, the day of the procedure was looked at, in addition to whether it was performed in the morning or afternoon.
8 tonsillectomies were done on Monday, 3 on Tuesday, 12 on Wednesday, 23 on Thursday, and 8 on Friday. No significant trend was found to the results.
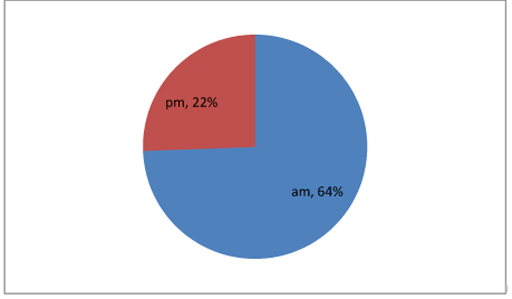
Focusing on when the operation was done, the number of procedures done in the morning and afternoon were counted before calculating what proportion of them were completed as day cases.
36 tonsillectomies were done in the morning, with 23 of them managed as day cases - 64%. On the other hand, just 4 out of 18 tonsillectomies done in the afternoon were managed as day cases - 22%. Using Fisher's Exact Test, these figures represent a P value of 0.008 (significance P<=0.05), confirming a significant difference in day case rates depending on the time of day. Figure 3 displays these percentages in a pie chart.
FIGURE 3: Day surgery rate in relation to the timing of the operation - morning against afternoon.
As mentioned previously, the trust will consider admitting patients who undergo tonsillectomies with a background of sleep apnoea. To see if this was the case, the management of each patient with a history of sleep apnoea was looked at, excluding patients with sleep disordered breathing. The results showed that 10 patients had a history of sleep apnoea, and just one of these was managed as a day case - 10%.
2 patients had a history of heart problems - 1 with an AVSD associated with Down's Syndrome, and the other with CHD and a bicuspid aortic valve. Both of these patients were kept overnight.
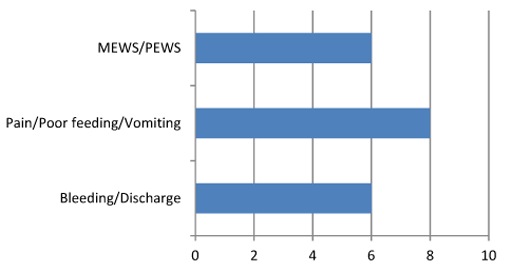
Any problems experienced by the patients were well documented by the nurses, including both surgical and non-surgical problems. Non-surgical problems recorded included any bleeding or discharge, refusal to take in fluids or food, nausea and vomiting, excessive pain, and any changes to the patient's MEWS/PEWS score.
20 patients had one or more of these problems documented with 4 going home on the day of the operation - 20%. Figure 4 looks at the surgical problems encountered.
FIGURE 4: Post-op complications. 4 of these 20 patients went home the same day.
7 patients presented at later dates due to complications - 13%. 5 of these were managed as day cases. Of the 7 patients, 2 were admitted within 24 hours of the operation. 4 patients were admitted due to post-op bleeding (7.4%), with 2 being taken to theatre for surgical arrest of the bleeding (3.7%). The remaining 3 patients suffered post-operative infections causing a sore throat, fever, and vomiting. These patients were managed with antibiotics.
As shown earlier, the most recent month of April 2015 had a day case rate of 31%. We aim to determine if the factors identified above that contribute to a low day case rate, were more prominent within this month. 13 tonsillectomies were done in April 2015, with 4 completed as day cases.
4 were performed on patients under the age of 6, all being managed as inpatients; and 2 in the 12-18-year-old bracket, with both being staying overnight. 5 of the 13 operations were adenotonsillectomies, all resulting in inpatient stay. 3 patients also had additional procedures done, resulting in admission for the night.
The average duration of the operation over the month was 28.69 minutes - dropping to 26 minutes for the day cases, but rising to 29.88 for the inpatients. 6 out of 7 of the tonsillectomies done in the afternoon resulted in an overnight stay, whereas out of the 6 procedures done in the morning, half were managed as day cases.
Out of the 13 patients, 6 had 'problems' documented by nurses, and 3 had a history of sleep apnoea. All of these patients were managed as day cases. No patients were readmitted in this month due to any complications.
Discussion
The British Association of Day Surgery has identified a target of 85% of tonsillectomies to be completed as day cases (4). In April 2015, UHSM completed 33% of tonsillectomies as day cases. The results reflect reasons of why some procedures were not completed as day cases and areas in which the day case rate could be improved.
The age of the patient represents one of these areas. 29% of tonsillectomies done on children under the age of 6 were completed as day cases, much lower than the percentages shown for the other age groups. Identifying these patients and planning accordingly could increase the number of procedures done as a day case.
There is a significant difference in the day case rates regarding the type of operation done. 68% of patients who underwent bilateral tonsillectomies were discharged the same day, compared to 21% for those who had adenotonsillectomies. Both of these figures are short of the target, however, with adenotonsillectomies, there is huge room for improvement and by identifying patients undergoing this procedure, better planning can be made in order to improve the day case rate.
Additional procedures done during the same anaesthetic as the tonsillectomy also result in a larger proportion of inpatient stays for patients. Focusing on these patients and providing appropriate care may also help improve the day case rate.
Another factor influencing the day case rate is the time of the operation. The results show that tonsillectomies done in the morning are much more likely to be completed as day cases than tonsillectomies done in the afternoon. The corresponding day case rates are 64% and 22% respectively. By planning ahead and aiming to complete more tonsillectomies in the morning, the day case rate could be improved.
The study does not take into account each individual surgeon's rate of day case surgery, as the number of cases carried out by each surgeon are too small to provide any significant conclusion. Therefore, a study looking into this further may be needed.
For the 10 patients with a history sleep apnoea, just 1 managed to go home the same day of the operation. The guidelines are not clear on how these patients should be managed, but this could be looked at further in order to increase day case rates.
One study looked into the safety of day case tonsillectomy in patients with sleep apnoea (7). In 165 patients with sleep apnoea and no other co-morbidities, there were 37 complications. These were grouped into surgical (bleeding), medical (dropped saturations) and social (pain and poor feeding). Surgical and social rates were similar to those in patients without sleep apnoea. 10 patients had complications specific to sleep apnoea (desaturations) - 6.1%.
This study concluded that patients with sleep apnoea and no other co-morbidities can be safely managed as day cases. It suggests the patient should be monitored for desaturations for 6 hours postoperatively before being discharged the same day7. However, further studies within UHSM looking into sleep apnoea are required before creating safe Trust guidelines.
Patients with documented problems while in recovery and following the surgery were more likely to be kept in as inpatients. One study shows that patients undergoing day case surgery had better sleep, oral intake, and less pain during the first postoperative night (8). However, this study also indicates that the patients kept overnight would have found day case surgery less tolerable. Following a questionnaire 2 weeks post-op, 92% of patients revealed they preferred tonsillectomy completed as a day case8.
Social and non-surgical factors for the reduction in day case rates were not investigated in this study as the case notes did not provide this information. A separate study into these reasons may be beneficial to further improve the day case rate.
The results of this study showed no significant difference in relation to the duration of the surgery. It is difficult to discuss how to improve the day case rates in patients with documented problems, as it is subjective. However, with reassurance and good quality care, the day case rate could possibly be improved further.
Many papers have looked into the safety of tonsillectomies being performed as day cases and encouraged it due to complication and readmission rates being low in general (9). Postoperative haemorrhage rates have ranged from 0.14 to 8.5% in a variety of papers (10). 7.4% of the patients in this study were readmitted due to haemorrhage.
Conclusions
Day surgery has several benefits. The majority of patients have positive experiences as they spend the night at home in a more comfortable environment, while staff also benefit from the clear pathway in place. Day surgery provides healthcare with the opportunity to save money in bed occupancy and nursing care. At UHSM, £6,568 could be saved by increasing the day case rate to 75%, with potentially more being saved if the target of 85% was met. Day surgery is a safe way to provide high quality care in the most cost-efficient way, improving clinical outcomes.
This study showed that we are significantly below the required standards, and day-case rates have been falling over the past few years. Several factors that could well be contributing to this were identified. Those factors are as follows:
- Age of the patient
- Time of the operation
- Type of procedure
- Additional procedures done
- Surgeon performing the surgery
- Background of sleep apnoea
- Complications
Each factor requires further investigation using a larger number of patients to identify ways in improving each factor separately. By focusing on each factor, it may be possible to increase the day case rate and achieve the 85% target in the future.
References
- NHS Institute for Innovation and Improvement. Treating Day Surgery as the Norm. http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/day_surgery_-_treat_day_surgery_as_the_norm.html (accessed 10/06/2015)
- NHS Institute for Innovation and Improvement. Better Care, Better Value Indicators. http://www.productivity.nhs.uk (accessed 10/06/2015)
- Department of Health NHS Modernisation Agency. 10 High Impact Changes for Service Improvement and Delivery, 2004. http://www.ogc.gov.uk/documents/ Health_High_Impact_Changes.pdf (accessed 10 ⁄ 06 ⁄ 2015)
- British Association of Day Surgery. BADS Directory of Procedures, 3rd edn. London: BADS, 2009.
- Lock, C; Wilson, J; Steen, N; Eccles, M; Mason, H; Carrie, S; Clarke, R; Kubba, H; Raine, C; Zarod, A; Brittain, K; Vanoli, A; Bond, J. North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel nonrandomised preference study, Health Technol Assess. March 2010;14(13):1-164
- Commissioning Guide: Tonsillectomy, 2013, ENTUK, RCS Advancing Surgical Standards. https://www.rcseng.ac.uk/healthcare-bodies/docs/published-guides/tonsillectomy (accessed 13/06/2015)
- Youshani, A, S; Thomas, L; Sharma, R, K. Day case tonsillectomy for the treatment of obstructive sleep apnoea syndrome in children: Alder Hey experience. Int J Pediatric Otorhinolaryngology, Feb 2011; 75(2):207-10
- Soreide, A, K; Olofsson, J; Tonsillectomy - day surgery or hospitalization? Tiddsskr Nor Laegeforen. 1999 April 20;119(10):1423-7
- Ahmad, Z; de Silva, N; Morton, R, P; Wood, A. Safety of day-stay tonsillectomy. J. Otolaryngol. Head Neck Surg. April-June 2010 62(2):158-161
- Verma, A; Nabhani, S, A; Al-Khabori. Adult tonsillectomy and day case surgery. J. Otolaryngol. Head Neck Surg. October-December 2007 59, 341-345
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6010/guirguis.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=1287#collapse6