Dave Bunting
2020 was a difficult year for all with the Covid-19 pandemic having the greatest impact on our health service in many years, not to mention the negative effects is has had on the education of children and young people and the lasting effect it will have on businesses and our economy. Never in recent years has the health service had to learn to adapt so quicky and to such a great extent. When I wrote the last editorial of 2020, I hoped that we might by now be seeing some positive effects of widespread coronavirus vaccination. I feel this is starting to be the case and whilst there are fears that current vaccines may not offer full protection to the new Covid variants, as I write this, I have learned the UK has successfully vaccinated over 12 million of its most vulnerable people and looks to be able to reach its target of having offered a first vaccine dose to all of its highest risk patients by mid-February. As we emerge from this era and find new ways of safely providing surgical care during the ongoing pandemic, day surgery units are going to play a huge part in restoring our elective and urgent care services in an effort to keep up with ongoing demand and deal with the inevitable waiting list backlog that has developed in most specialties.
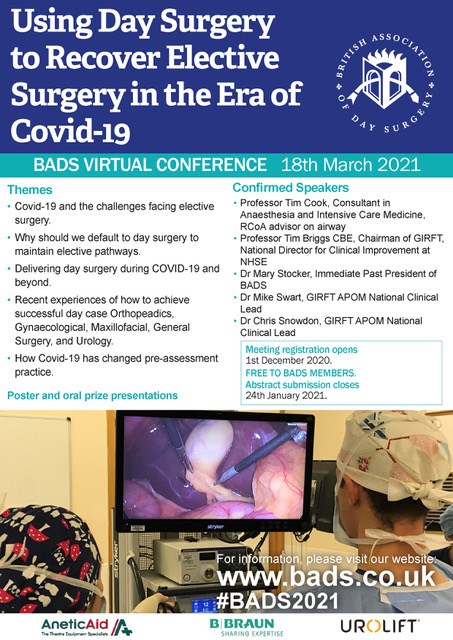
The BADS Virtual Conference will be taking place next month on Thursday 18th March and will focus on how day surgery can be used to recover elective surgery in the Covid-19 era. Importantly, it will be delivered free of charge to all current BADS members so please register by following the link on the BADS homepage:
https://daysurgeryuk.net/
All presented material, including video recordings of invited speakers’ lectures and oral prize presentations, will be available online for participants to access free of charge for three months following the conference.
In this edition of JODS, three updated ‘How I do it’ day case guides are presented, this month with an orthopaedic theme. They include guides on Day Case Total Hip Replacement, Day Case Total Knee Replacement and Day Case Anterior Cruciate Ligament Reconstruction.
Please keep your submissions to the Journal coming in and remember – JODS still offers citable peer-reviewed publication with no author processing fees. Author guidelines and submission instructions can be found in this edition of the journal.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49085/311-ed.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse0

Kim Russon
I hope you are all safe, well and managed to get some rest over the Christmas period. Unfortunately, 2021 has not started in a way we would have ideally wished, with Covid19 numbers rising and Mr Johnson announcing that the NHS should move to alert level 5 and that the country would begin another national lockdown. Thankfully, the lockdown seems to be working, and hospital Covid19 numbers appear to be stabilising and hopefully will soon start to fall. The NHS is still under tremendous pressure and in many hospitals elective surgery has had to stop again. This causes great concern as we are already aware of growing waiting lists with over 80,000 patients known to have been waiting over 1 year for surgery and over 4 million unreferred patients. It has been reported that even if elective surgery returns to 110 or 120% of pre-covid levels it may take years to “catch up”.
Day surgery continues to be recognised as a potential solution and in centres where Covid-secure pathways have been developed, day surgery has been able to carry on. As I mentioned in November, the GIRFT Elective surgery recovery and transformation programme promotes day surgery pathways and is hoped to be able to rolled out nationally. At the recent BADS/HCC Day case general surgery conference we heard Ms Stella Vig describe how by utilising day surgery pathways, Croydon University Hospital achieved greater than 100% of activity as compared to pre-covid activity to help tackle its growing waiting lists due to the impact of Covid-19 pandemic.
BADS is delighted to announce that we are continuing our collaboration with Health Care Conferences (HCC) to bring you one day speciality focussed conferences where teams achieving successful day surgery share their knowledge and pathways to enable other centres to learn how to deliver similar services.
- Daycase Major Knee Surgery –25th March 2021
- Day Case Total Hip Replacement –29th April 2021
- Day Surgery in Gynaecology – 20th May 2021
- Day Case General Surgery During Covid19 18th June 2021
- Breast Surgery as Day Surgery 7th Sept 2021
- Day case Urology Date TBC
We also have our BADS annual conference next month with great speakers and an excellent programme which we hope will assist hospitals to recover elective surgery using day surgery pathways. If you haven’t already registered then please do soon. Registration is free for BADS members and if you are not available on the 18th March then the recording will be available afterwards for 3months for non-BADS members and 1 year for BADS members.
During this continued time of pressure, both on our working lives and home lives it is important to consider our wellbeing. BADS council took a moment during our recent council meeting for #coffeeandagas which is an Association of Anaesthetists campaign to help wellbeing and promote better teamwork. Please look after yourselves and each other.
I look forward to welcoming you all to the BADS conference 18th March 2021.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49083/311-pres.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse1
See the 2021 Virtual Conference programme here:
https://daysurgeryuk.net/media/352338/bads_2021_virtual_prog-22.pdf
Click the image below to find out more about the virtual conference on our website.
Conference registration is FREE for BADS members.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49081/2021-virtual-prog-60221.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse2
Claire Blandford, Consultant Anaesthetist
David Isaac, Consultant Orthopaedic Surgeon,Torbay & South Devon NHS Foundation Trust, Devon.
Patient Selection
-
Symptomatic knee pathology requiring TKR
-
Engaged with day case pathway
-
No unstable medical co-morbidity requiring in-patient management
-
No high dose opioid based analgesia /chronic pain regimen pre-operatively
-
Suitable social support
Pre-online Preparation
From booking:
- Pt counselled to expect DC procedure
- Nurse led pre-assessment process completed
- Participation in ‘joint-school’ patient education programme
On the day:
- Listed first on theatre list (ideally)
- Withhold ACE inhibitor/ A2RB drug on day of and day before surgery
- Carbohydrate drink 2hrs pre-op
- Pre-medication:
- Paracetamol 1g
- Ibuprofen 1600mg SR (if not contraindicated)
- Oxycodone MR 10mg (5mg dose if age >70)
Anaesthetic Technique
Spinal:
-
3 – 3.4ml hyperbaric 2% Prilocaine
-
NO intrathecal opioid
Sedation:
- Aim to minimise/ avoid. If required then low dose Propofol TCI with capnomask.
Local Anaesthesia:
- Ultrasound guided saphenous nerve block (0.25% levobupivacaine up to 20mls) + Surgical infiltration (ensure maximal LA dose not exceeded with combined technique)
Antiemetics: (dual agents as standard)
-
Dexamethasone 6.6mg IV
-
Ondansetron 4mg IV
-
Intra Operative Care
Goal directed:
-
Normothermia: proactively warm patient with forced air blanket (commence pre-op) & fluid warmer
-
Normovolaemia: IV fluids 1000-2000mls (warmed)
Blood Conservation:
-
Tranexamic Acid 1g IV start of case + further 1g at end of case (dose reduced for eGFR<50 and or weight <50kg)
-
Cell salvage collection routinely
Antibiotic Regimen:
-
Teicoplanin (slowly in 100mls n/saline) & Gentamicin [weight adjusted doses]
-
Thromboprophylaxis: mechanical- foot pump used intra-operatively & until mobilisation. Dalteparin 5000units (weight adjusted) sc pre-discharge.
Key recovery priorities:
-
Manage any PONV aggressively
-
Commence oral fluids
-
Fortisip 200ml drink
Surgical Technique
-
Parapatellar approach
-
Tourniquet only inflated for cementation
-
Local Infiltration of Anaesthetic to divided tissue, periosteum and subdermal fat layers. 80 ml 0.125% levobupivacaine or 40mls 0.25% levobupivacaine according to individual surgeon’s preference.
-
Careful wound closure in layers to include continuous absorbable suture to skin, plus tissue glue
Take Home Medication
-
Paracetamol 1g qds
-
Ibuprofen 400mg-600mg po qds 5/7 (if no contraindication) + PPI cover (Lansoprazole 15mg)
-
Oxycodone MR 10mg po bd for 5 post op doses (*5mg if age >70) with reinforced non continuation of this via discharge summary (automated process)
THEN step down on Day 3 to: Codeine 30-60mg po qds OR Tramadol 50-100mg qds if codeine intolerant for 3/7.
Ondansetron 4mg po tds 2/7
Macrogols 1 sachet po bd 5/7
Dalteparin 5000units sc od for 2/7 (+ sharps bin) then step down onto:
Aspirin 150mg po od 14/7
unless other anticoagulation plan in place eg warfarin/clopidogrel/ DOAC then usually restart this day 1 post op
Post Operative Care
-
Patient fulfils all standard daycase discharge criteria and demonstrate satisfactory mobilisation/ transfer abilities commensurate with safe discharge
-
X-ray taken pre-discharge and reviewed by surgeon
-
Day 1 nurse led telephone call from DSU
-
In-house ‘orthopaedic outreach’ nursing team visit patient in community; days 1,5,10 & 14 to support. Tasks include wound reviews, medication assistance, performing post op blood tests/ vital signs monitoring.
-
Direct telephone access to this service for patients
Organisational Issues
-
Theatre listing – patient needs first (or possibly 2nd) slot on a list
-
Consider your facilities estate resources to build your pathway; location of clean air theatres & day case discharge facilities.
-
Working hours of MDT support staff eg: physios may not align with time of patients discharge
-
Post-operative support for patients; diverse ways this may be able to be provided. Bespoke solution to your unit may be needed.
Common Pitfalls
-
Short acting spinal technique required to ensure full offset of sensory/motor block to allow adequate time for mobilisation. If unanticipated complications/ delays occur duration of block may become an issue.
-
All staff need to be ‘on message’ so that the patient has confidence in the daycase pathway
-
First mobilisation hypotension – we have found the ‘fortisip’ drink invaluable in reducing this, alongside good hydration and dual antiemetic regimen
Anticipated Day case Rates
- Not all patients will be suitable for daycase management.
- Estimates indicate approx. 20% of a waiting list cohort may be DC suitable
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49087/311-hidi-blandford-2.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse4
Claire Blandford, Consultant Anaesthetist
Mike Kent, Consultant Orthopaedic Surgeon
Torbay & South Devon NHS Foundation Trust, Devon
Patient Selection
-
Symptomatic hip pathology requiring THR
-
Engaged with day case pathway
-
No unstable medical co-morbidity requiring in-patient management
-
No high dose opioid based analgesia /chronic pain regimen pre-operatively
-
Sufficient social support
-
Suitable social support
Pre-operative Preparation
From booking:
-
Pt counselled to expect DC procedure
-
Nurse led pre-assessment process completed
-
Participation in ‘joint-school’ patient education programme – Face to Face education sessions with nursing team and physiotherapist, video presentation, comprehensive information booklet
On the day:
-
Listed first on theatre list (ideally)
-
Withhold ACE inhibitor/ A2RB drug on day of and day before surgery
-
Carbohydrate drink 2hrs pre-op
Pre-medication:
- Paracetamol 1g
- Ibuprofen 1600mg SR (if not contraindicated)
- Oxycodone MR 10mg (5mg dose if age >70
Anaesthetic Technique
Spinal:
-
3 – 3.4ml hyperbaric 2% Prilocaine
-
NO intrathecal opioid
Sedation:
- Aim to minimise/ avoid. If required then low dose Propofol TCI with capnomask.
Local Anaesthesia:
-
Surgical Infiltration 0.25% levobupivacaine 50mls (40mls if patient weight <60kg)
-
Antiemetics: (dual agents as standard)
Antiemetics: (dual agents as standard)
-
Dexamethasone 6.6mg IV
-
Ondansetron 4mg IV
Intra Operative Care
Goal directed:
-
Normothermia: proactively warm patient with forced air blanket (commence pre-op) & fluid warmer
-
Normovolaemia: IV fluids 1000-2000mls (warmed)
Blood Conservation:
-
Tranexamic Acid 1g IV start of case + further 1g at end of case (dose reduced for eGFR<50 and or weight <50kg)
Cell salvage collection routinely
Antibiotic Regimen:
-
Teicoplanin (slowly in 100mls n/saline) & Gentamicin [weight adjusted doses]
-
Thromboprophylaxis: mechanical- foot pump used intra-operatively & until mobilisation. Dalteparin 5000units (weight adjusted) sc pre-discharge.
Key recovery priorities:
-
Manage any PONV aggressively
-
Commence oral fluids
-
Fortisip 200ml drink
Surgical Technique
General
- Standard THR as per surgeon’s usual technique
- Techniques/implants allow for full weight bearing as soon as feasible
Intraoperative
- Meticulous haemostasis, use of cell salvage, aim to retransfuse if threshold reached
- Infiltration of high volume/low concentration local anaesthetic into surgical field (capsule/released muscles depending on approach/fascia lata/deep dermal)
- Abductors/Short External Rotators repaired with non-absorbable transosseous sutures depending on approach
- Meticulous multi layer closure with Vicryl absorbable sutures, Skin closure with moncryl and topical skin glue, Opsite dressing
Postoperative
- Patients mobilised by physiotherapist as soon as ready
- Relaxed dislocation precautions
Take Home Medication
-
Paracetamol 1g qds
-
Ibuprofen 400mg-600mg po qds 5/7 (if no contraindication) + PPI cover (Lansoprazole 15mg)
-
Oxycodone MR 10mg po bd for 5 post op doses (*5mg if age >70) with reinforced non continuation of this via discharge summary (automated process)
THEN step down on Day 3 to: Codeine 30-60mg po qds OR Tramadol 50-100mg qds if codeine intolerant for 3/7.
Ondansetron 4mg po tds 2/7
Macrogols 1 sachet po bd 5/7
Dalteparin 5000units sc od for 2/7 (+ sharps bin) then step down onto:
Aspirin 150mg po od 28/7
unless other anticoagulation plan in place eg warfarin/clopidogrel/ DOAC then usually restart this day 1 post op
Post Operative Care
- Patient fulfils all standard daycase discharge criteria and demonstrate satisfactory mobilisation/ transfer abilities
- Patient fulfils all standard daycase discharge criteria and demonstrate satisfactory mobilisation/ transfer abilities commensurate with safe discharge
- Check X-ray performed prior to discharge
- Day 1 nurse led telephone call from DSU
- In-house ‘orthopaedic outreach’ nursing team visit patient in community; days 1,5,10 & 14 to support. Tasks include wound reviews, medication assistance, blood tests/ vital signs monitoring.
- Direct telephone access to this service for patients
Organisational Issues
- Theatre listing – patient needs first (or possibly 2nd) slot on a list
- Consider your own facilities/ estate resources to build your pathway; location of clean air theatres & day case discharge facilities.
- Working hours of MDT support staff eg: physios may not align with time of patients discharge
- Post-operative support for patients; diverse ways this may be able to be provided. Bespoke solution to your unit may be needed.
Common Pitfalls
- Short acting spinal technique required to ensure full offset of sensory/motor block to allow adequate time for mobilisation. If unanticipated complications/ delays occur duration of block may become an issue.
- All staff need to be ‘on message’ so that the patient has confidence in the daycase pathway
- First mobilisation hypotension – we have found the ‘Fortisip’ drink invaluable in reducing this, alongside good hydration and dual antiemetic regimen.
Anticipated Day case Rates
- Not all patients will be suitable for daycase management.
- Estimates indicate approx. 20% of a waiting list cohort may be DC suitable
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49088/311-hidi-blandford.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse5
MICHAEL HOCKINGS & MARY STOCKER
(Original article published 2013, updated 2020)
Patient Selection
-
No specific selection criteria
Anaesthetic Techniques
- Short acting general anaesthetic:
We use TIVA with propofol and remifentanil - Saphenous nerve block which provides a slightly less reliable sensory block than a femoral nerve block but has the advantage of no motor block. This is the preferred technique surgically to enable full weight bearing immediately post operatively
30 mls. 0.25% Bupivacaine (reduced to 1mg/kg if under 75kg)
Surgical Technique
- Infiltration of local anaesthetic into the skin around the harvest site of patellar tendon or hamstrings and the arthroscopic portals
30mls of 0.25% Bupivacaine total (reduced to 1mg/ kg if under 75kg)
Peri-operative analgesia
-
Pre-operative: oral paracetamol and ibuprofen
-
Intra-operative: iv fentanyl
-
Post operative: regular paracetamol and ibuprofen
-
Rescue intravenous fentanyl or oral morphine if required
Take Home Medication
-
Paracetamol 500 mg/ codeine 30mg po qds, laxido 1 sachet bd, plus ibuprofen 600 mg po qds
Organisational Issues
-
Surgeon must write x- ray request form before patient leaves theatre
-
Intravenous teicoplanin 400 mg on induction avoids the need for further post operative doses of antibiotics
-
Physiotherapist must be available to see patient preoperatively or immediately post operatively to fit knee brace and aid timely discharge
Anticipated Day case Rates
- 90%
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/51043/how-i-do-it-anterior-cruciate-ligament-1.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse6
Dr Claire Blandford, Consultant Anaesthetist, Torbay & South Devon NHS Foundation Trust
Day case surgery continues to push boundaries and offer huge potential benefit for NHS trusts and patients. However, achieving total joint arthroplasty as a day case procedure is somewhat of a new frontier for many trusts - consequently there has been significant appetite for specific conferences addressing these principles. Following on from a series of well received conference dates in 2018/19, HCUK (Healthcare Conferences UK) partnered with BADS (British Association of Day Surgery) to offer two dates in Autumn 2020, this time utilising virtual platforms due to the limitations of the COVID pandemic.
The days were specifically themed to allow maximal extractable relevance for delegates and aimed to provide a comprehensive review drawn from national experts and shared experience across several centres in the UK. Small group breakouts were included throughout both programmes, along with virtual networking opportunities and an online exhibition. We would also like to thank our sponsors for their contribution to these two events.
Day case Major Knee Replacement (05.10.20)
This conference included anterior cruciate ligament (ACL), uni-compartmental knee (UKR) and total knee replacement (TKR) themes. The conference was chaired by BADS council members and delivered via a Zoom facilitated platform. Dr Kim Russon (Consultant Anaesthetist - Rotherham and president of BADS) chaired the morning sessions. The first speaker was Dr Mary Stocker (Consultant Anaesthetist - Torbay and immediate past president of BADS) who delivered a comprehensive session on optimising day case pathways and key elements of suitability & planning. This was then followed by two centres giving insights into how they had successfully transitioned their services to facilitate day case joint arthroplasty: Rotherham NHS Foundation Trust and Torbay & South Devon NHS Foundation Trust.
The Rotherham team, comprising Mr Alex Anderson (Consultant Orthopaedic Surgeon), Dr Kim Russon (Consultant Anaesthetist) & Ms Kayleigh Wright (Specialist Physiotherapist) presented their work on developing a default to day surgery process for ACLs and how this evolved to facilitate day case UKR surgery. They noted transitioning their discharge location from inpatient ward to dedicated day surgery unit improved their same day discharge rates. This session was then followed by the Torbay team of Dr Claire Blandford (Consultant Anaesthetist), Mr David Isaac & Mr Mike Kent (Consultant Orthopaedic Surgeons) who presented nine years of local experience in achieving day case ACLs and UKR surgery; progressing more recently to include successful day case total hip & knee arthroplasty (>90% same day discharge rates achieved.) The team presented the transformational process undertaken to achieve this and the precise details of their surgical and anaesthetic pathways.
The afternoon session was chaired by Dr Mary Stocker. The first speaker was Dr David Johnston (Consultant Anaesthetist- Belfast) who covered analgesic aspects of knee arthroplasty surgery presenting various local anaesthetic techniques and multimodal strategies. This was followed by Dr Robbie Erskine (Consultant Anaesthetist – Derby) who described a ‘golden combination’ of ultra short-acting spinals with long lasting blocks to facilitate day case surgery. His talk provided a wealth of useful information and the principles he conveyed would also have application to other surgical procedures. We then heard from Dr Stocker again who’s afternoon session really highlighted the critical value of data- not only in uniting teams in shared ownership of outcomes but also as a driver for units to refine process and performance. The final session of the afternoon was delivered by a surgeon/ anaesthetist team from Calderdale; Mr Graham Walsh (Consultant Orthopaedic Surgeon) & Dr Nisha Bhuskute (Consultant Anaesthetist). They presented their data, sharing impressive day case rates in TKR surgery and also showed how they utilise digital technology, including wearable tech directly linking discharged patients with hospital physio services to enhance patient experience.
Perhaps you will join us for the next two meetings on 25th March (Knee) & 29th April (Hip) 2021?
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47605/311-day-case-major-knee-replacement-conferences-report.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse7
Dr Claire Blandford, Consultant Anaesthetist, Torbay & South Devon NHS Foundation Trust
Day case surgery continues to push boundaries and offer huge potential benefit for NHS trusts and patients. However, achieving total joint arthroplasty as a day case procedure is somewhat of a new frontier for many trusts - consequently there has been significant appetite for specific conferences addressing these principles. Following on from a series of well received conference dates in 2018/19, HCUK (Healthcare Conferences UK) partnered with BADS (British Association of Day Surgery) to offer two dates in Autumn 2020, this time utilising virtual platforms due to the limitations of the COVID pandemic.
The days were specifically themed to allow maximal extractable relevance for delegates and aimed to provide a comprehensive review drawn from national experts and shared experience across several centres in the UK. Small group breakouts were included throughout both programmes, along with virtual networking opportunities and an online exhibition. We would also like to thank our sponsors for their contribution to these two events.
Day case Total Hip Replacement (04.11.21)
One month later and we had further ascended the lower limb to reach the hip joint as the focus for the day’s presentations. The morning was chaired by Mr Ed Dunstan (Consultant Orthopaedic Surgeon – Fife & BADS council member) and the afternoon was chaired by Dr Mary Stocker; who also delivered the first talk of the morning reprising her well received & highly informative session on optimising day case pathways. The next speaker was Mr Hiren Divecha (Consultant Orthopaedic Surgeon – Wigan) who presented the pathway by which they as a team had undertaken their first day case total hip replacement (THR). This session also included a personal account from one of Mr Divecha’s first patients who wholeheartedly endorsed his experience and provided a true insight into the physical & psychological benefits of day surgery to patients. The final session of the morning shared the experience of a surgeon/ anaesthetist team from Torbay; Mr Mike Kent (Consultant Orthopaedic Surgeon) & Dr Claire Blandford (Consultant Anaesthetist). They presented their work on enhanced recovery pathways, how they designed and introduced a day case hip replacement pathway to their trust and the refinements to process undertaken since.
The programme had a further 4 sessions in the afternoon. Mrs Hilary Young (Advanced Nurse Practitioner) presented the Northumberland experience. Long recognised as a high-volume centre with low lengths of stay she introduced a new patient education app they had developed and discussed ways that effective teamwork & messaging enables early confident discharge. Hilary specifically highlighted the critical importance of early mobilisation in breaking the cycle of poor mobility/↑pain/↑medication/↑side effects/↓mobility. Dr Stocker also spoke in the afternoon delivering valuable advice on measurement and utilisation of data to achieve results. We then heard from Mr Ed Dunstan who described ‘The Scottish Journey’ discussing how their pathways have evolved over time, championing positivity in the NHS and sharing the splendid patient feedback their pathway has generated. His talk was complimented by Mr Steve Young’s session (Consultant Orthopaedic Surgeon – Warwick) who shared insights of development in their unit spanning 15 years+, raised consideration of how we define ‘failure’ and ‘success’ and proposed six key focal areas for delivering successful outcomes in this field.
In summary these two days brought together experts and enthusiasts from across the United Kingdom to share ideas and learning. We heard from many centres who are all achieving excellent outcomes and whilst certainly there are some common core principles in achieving successful day case joint arthroplasty there is also much diversity of practice & ‘local bespoking’ too - which does draw to mind the lyrics of an 80’s pop song (if you’ll forgive the bracketed inclusion) “it ain’t (just) what you do, it’s the way that you do it”.
Perhaps you will join us for the next two meetings on 25th March (Knee) & 29th April (Hip) 2021?
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47606/311-day-case-major-hip-replacement-4th-november-2020-joint-bads-hcuk-conferences-report.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse8
Vanessa Cubas, General Surgery Trainee West Midlands, BADS Council Member
Friday 4th of December 2020 saw a joint British Association of Day Surgery (BADS) and Healthcare Conferences UK (HCUK) one- day conference titled “Daycase General Surgery During COVID-19”. This virtual conference is a modification of the previously successful “Developing your Daycase General Surgery Service”. It saw delegates and presenters from across the UK come together from different clinical backgrounds for what promised to be an educational and thought provoking day appropriate for the current climate in view of COVID-19.
The meeting was chaired by BADS council members: Mr David Bunting, Consultant Upper GI Surgeon from North Devon District Hospital, and Ms Vanessa Cubas, General Surgery Trainee. The first session was delivered by Dr Kim Russon, Consultant Anaesthetist and BADS president. Dr Russon presented a comprehensive overview of the day surgery pathway from GP referral to discharge from hospital and recovery at home, including appropriate patient selection. Importance was placed on dedicated facilities separate from inpatient beds to enable expertise to be developed in managing day case patients. Quality improvement was introduced as a way of widening the inclusion criteria for day case surgery including those who live alone, the older population, the obese, and more complex surgical procedures. It was also an opportunity to introduce the new Sixth Edition of the BADS Directory of Procedures, Model Hospital Tool and BADS Directory of Procedures National Dataset 2020.
The next part of the morning session introduced the current effects of COVID-19 on elective surgery and day surgery pathways. This session was presented by Professor Doug McWhinnie, President of the International Association of Ambulatory Surgery (IAAS) and Consultant Surgeon. This was further supplemented by a session by Mr Arin Saha, Consultant Upper GI surgeon and National lead for The Surgical Ambulatory Emergency Care Network, who discussed Same Day Emergency Surgery (SDEC). This remains a hot topic across the NHS. Properties of high-functioning surgical ambulatory units were discussed, challenges currently encountered, options of integration of SDEC units with the Think 111 pilot and the future in view of COVID-19. Dr Ian Jenkins, Past President of BADS and IAAS and Consultant Anaesthetist, provided the anaesthetic perspective of the challenges encountered in ambulatory surgery care.
Just before lunch Mr Charles Hendrickse, Consultant Colorectal Surgeon, discussed the setting up of an extremely successful dedicated COVID-19 free unit for elective surgery for University Hospitals Birmingham.
Following lunch, Mr Graham Lomax (Deputy National Delivery Director), held a session on the Getting it Right the First Time (GIRFT) national programme that addresses national variation on day case services. He also discussed the London recovery of elective surgery in view of COVID-19, the proposed general surgery pathways and the importance of a collaborative approach with managers and clinicians to optimise outcomes.
Ms Stella Vig, Consultant Vascular surgeon, gave a session on Croydon Health Services NHS Trust experience on “Cold” site operating and the importance of defaulting to day surgery in the new COVID-19 era and protecting cold/green site pathways. Ms Vig’s unit has been so successful that they have achieved over 100% activity compared to 2019. This was complemented by Senior Charge Nurse Catherine Jack from Queen Margaret Hospital Fife who discussed the units plans to continue with elective surgery during the second wave and gave her valuable experience on encouraging staff wellbeing during this difficult time.
Following afternoon coffee, Mr David Bunting talked about improving day case laparoscopic cholecystectomy rates and the North Devon experience with the Royal College of Surgeons’ Cholecystectomy Quality Improvement Collaborative (Chole-QuIC) project. Additionally, tips and advice on how to maintain a “Hot Gallbladder” service in the COVID -19 era was discussed. This was followed by Mr Paul Super, Consultant Upper GI Surgeon from the Heart of England Foundation Trust in Birmingham talking about day case fundoplication and anti-reflux surgery. Nationally, the day case rate for anti-reflux surgery is about 15%, however the rate at Heartlands is in excess of 80%, with an overwhelmingly positive patient feedback. Mr Super outlined the patient pathway and general principles for day case hiatal surgery that have enabled the unit to achieve these impressive results.
A big thank you to all the speakers and all those involved in organizing a successful day conference, and to all the delegates who attended and contributed to the discussion on the day.
Due to excellent feedback from this meeting, it is being held once again on Friday 4th of June 2021.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47610/311-bads-hcuk-conference-daycase-general-surgery-during-covid19.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse9
K Kennedy1, J Appiah-Ankam2, BVS Murthy3
1 Specialist Registrar in Anaesthetics, Royal Liverpool and Broadgreen University Hospitals, Liverpool
2 Consultant Anaesthetist, Royal Liverpool and Broadgreen University Hospitals, Liverpool
3 Consultant Anaesthetist, Royal Liverpool and Broadgreen University Hospitals NHS Trust, and Honorary Associate Professor of Health and Life Sciences, University of Liverpool, Liverpool
Corresponding author: Prof. BVS Murthy, Consultant Anaesthetist, Preoperative Assessment Unit, Broadgreen Hospital, Thomas Drive, Liverpool L14 3LB
Email: Burra.Murthy@rlbuht.nhs.uk
Abstract
Introduction: Shoulder surgery is known to be extremely painful and yet it has become successful as a day case procedure due to the routine use of brachial plexus blocks. Recent work has delineated that patients may be experiencing pain following discharge once the brachial plexus block has worn off. A service evaluation was undertaken to assess the incidence of post-operative pain in the first 48 hours and patient satisfaction in patients undergoing day case arthroscopic shoulder surgery.
Methods: This prospective qualitative service evaluation was conducted between January 2019 and June 2019 in patients undergoing day case arthroscopic shoulder surgery on Mondays and Wednesdays with a telephone follow-up interview on Wednesdays and Fridays.
Results: In the immediate post-operative period, out of 50 patients, 48 had good pain relief with no pain; 2 patients (4%) required additional analgesia in recovery or on the day-case unit. During the 48-hour follow up we found that 11 patients (30%) reported severe pain and 12 patients (33%) reported moderate pain at rest. Overall, the mean patient satisfaction score was 8.43. Satisfaction scores were higher for patients experiencing mild to moderate pain compared to severe pain at 48 hours post-operatively (P > 0.05).
Conclusion: We appreciate that patients’ experiences of pain could be improved. We hope to make our post-operative pain protocols more robust and to ensure all patients receive a comprehensive written patient education leaflet about their postoperative pain management.
Keywords: shoulder surgery; day surgery; pain; satisfaction
Introduction
Over the past 40 years, surgery has undergone significant developments leading to widespread change to day case (ambulatory) procedures. This has only been possible with the introduction of new surgical techniques, advances in anaesthesia, and the collection and publication of comparative data, with financial incentives for hospitals to do so.1 In 2013-14, 60.7% of finished consultant episodes involved some form of procedure or intervention, with 95.2% of day case episodes involving a procedure or intervention.1 As per the NHS quality and service improvement tools ‘the patient must be admitted and discharged on the same day, with day surgery as the intended management’: it should be the norm rather than the exception.2
The development of shoulder arthroscopy has bought it into the realms of day case surgery. Although shoulder surgery is known to be extremely painful, it has become successful as a day case procedure due to the routine use of brachial plexus blocks, allowing for reduced opiate doses.3 With increasing use of regional blocks and multimodal analgesia, day case shoulder surgery has been widely adopted across the NHS and has been the norm at our Trust since 2014. Even though it had become a norm for the staff, we wanted to identify the impact on patient related outcomes with this change. We therefore conducted a prospective qualitative service evaluation to understand the patients’ needs, views, expectations, and satisfaction on day case arthroscopic shoulder surgery.
Methods
At a large tertiary University Teaching Hospital in the Northwest of England, we conducted a service evaluation of patients undergoing day case arthroscopic shoulder surgery on Mondays and Wednesdays between January 2019 and June 2019. This service evaluation was approved by the hospital audit department, and no ethical approval was sought due to the non-interventional nature of the work. During their preoperative assessment, all patients were given a leaflet with the details of the various methods of postoperative pain relief that would be offered following shoulder surgery including interscalene brachial plexus block (ISB), oral analgesia etc. During the assessment on the day of surgery, all patients were consented to both anonymised data collection and a post-operative telephone follow up interview.
In the intraoperative phase, anaesthetists were requested to complete a data sheet about preoperative analgesics, ISB details (including time of the block, and volume and concentration of local anaesthetic), any other intraoperative analgesia given, antiemetics used and the volume of intravenous fluids administered. In the recovery ward and day case unit, staff were requested to complete the data sheet with the pain score on admission and at discharge, and any analgesia or antiemetics given. In our unit, we routinely provide one week supply of oral analgesics (codeine and paracetamol) for post-operative pain relief as take-home medication. Occasionally, if the patient is experiencing more pain, we tend to prescribe tramadol and / or non-steroidal anti-inflammatory medication.
After 48 hours i.e., on Wednesday and Friday, a telephone follow-up interview was conducted by the day case unit staff about the patients’ pain management, their experience, sleep disturbance, nausea and vomiting (PONV) and their satisfaction. The overall satisfaction with their pain management was assessed using a visual analogue scale (0 = not happy at all and 10 = extremely happy).
Results
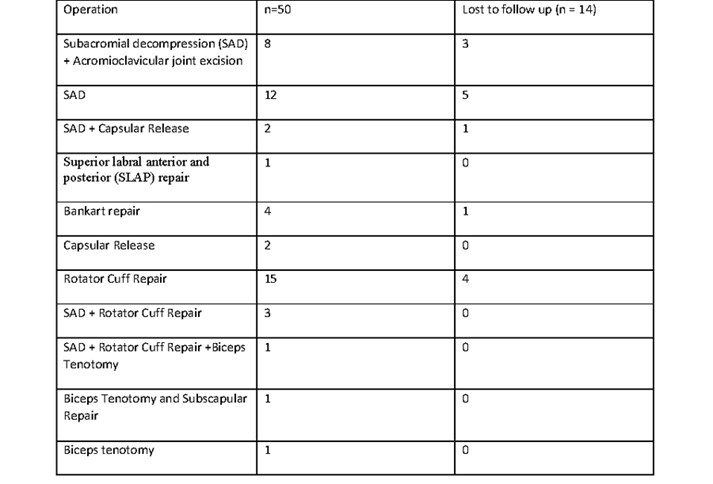
We were able to collect the data from 50 patients (32 males, 18 females) during their hospital stay. The patient ages ranged from 21-77 years (mean 52 years, and median 56 years). The details of various surgical procedures performed on the shoulder are listed in Table 1.
Table 1: The number patients having various surgical procedures and patients who were not contactable f
or a 48-hour postoperative follow up interview.
Intra-operative pain relief
94% of the ISB were performed with ultrasound and use of a peripheral nerve stimulator, the remaining cases were performed using ultrasound alone. The agent used for regional anaesthesia was levobupivacaine mainly with a strength of 0.375% (27 patients), however some anaesthetists used 0.25% (19 patients) or 0.5% (4 patients). The volume used ranged between 12-35 ml with a median of 20 ml. 45 patients received adjuvant dexamethasone (6.6 mg), of which 31 received it intravenously and the rest perineurally.
The range of intraoperative analgesics used was diverse with 34 patients receiving paracetamol, 19 had paracetamol combined with fentanyl or alfentanil, and 11 patients received alfentanil alone. Other analgesic techniques included a combination of those described with adjuncts of joint infiltration, magnesium or morphine/oxynorm. Only six patients received non-steroidal anti-inflammatory drugs (NSAIDs).
Post-operative pain relief
We noted a low incidence of immediate post-operative pain in our cohort with only 2 patients (4%) requiring additional analgesia in recovery or on the day case unit. Of these two patients, one had moderate pain following a subacromial decompression (SAD) and one had severe pain following a rotator cuff repair. The patient who had had a cuff repair and was in severe pain in recovery then complained of no pain on arrival to the ward following morphine 2 mg intravenously in recovery.
Table 2: Pain scores in first 48 hours following their surgery.
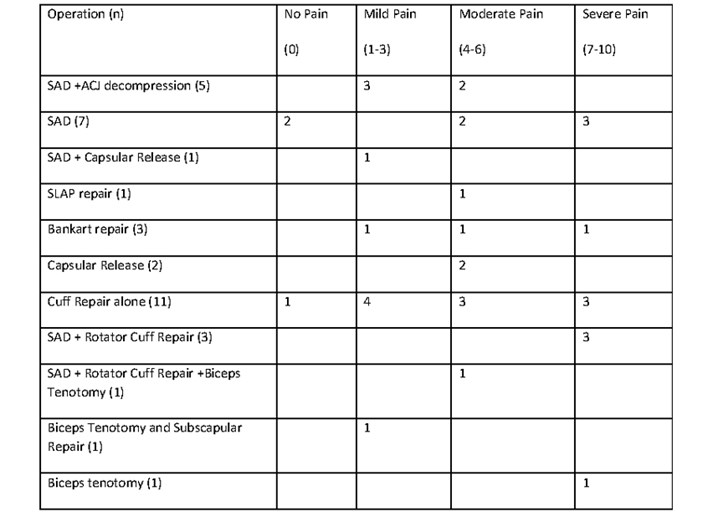
At our 48-hour post-operative follow up, we were able to contact 72% of patients (22 males + 14 females) to assess their experience, their post-operative pain relief, and their satisfaction. The mean duration of block in these patients was 20.5 hours (median 21 hours, mode 24 hours). As demonstrated in table 2, the pain experienced was variable and did not appear to correlate with the surgical procedure. However, cuff repairs did represent half of the patients in severe pain at 48 hours.
In this cohort, 11 patients (30%) reported severe pain and 12 patients (33%) reported moderate pain at rest within the first 48 hours (Table 2). Sleep disturbances were experienced by 25 patients on the day of operation due to pain, discomfort and pins and needles. During the follow up only 6 patients had problems with PONV, 3 were female.
Table 3: Mean, median and mode patient satisfaction scores about their pain relief at rest within first 48 hours of surgery.
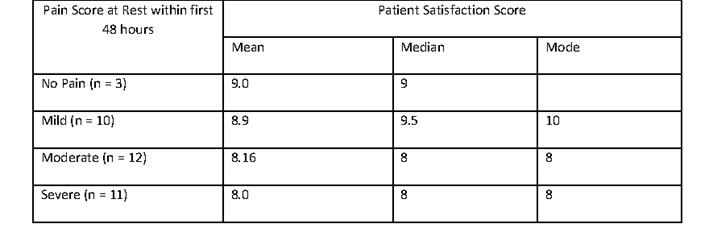
Patient satisfaction
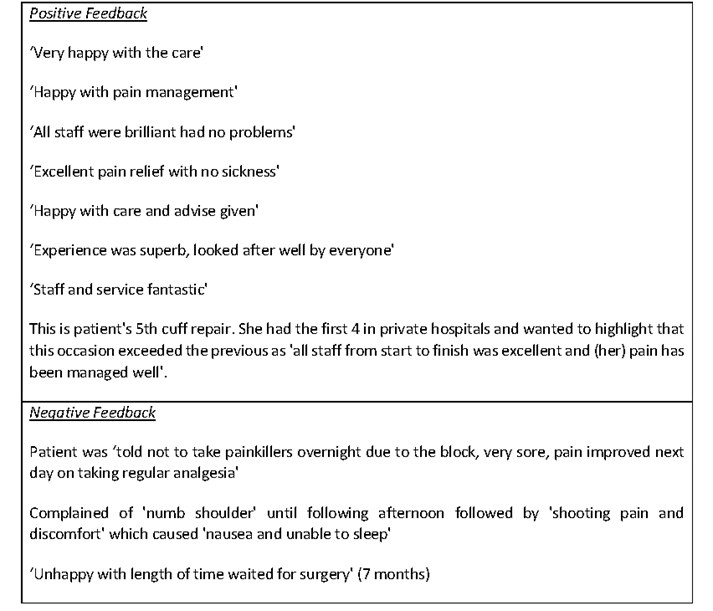
Overall, the mean patient satisfaction score was 8.43 (range 5-10, median 8). Satisfaction scores were higher for patients experiencing mild to moderate pain compared to severe pain (P > 0.05) at 48 hours post-operatively (table 3). The patient who scored 5 had a block duration of 25 hours but severe pain at rest and on movement at 48 hours. She was discharged on paracetamol, NSAID and codeine, but was receiving gabapentin preoperatively. Thirty patients (80%) felt the length of stay was about right. All the additional comments provided by patients on their experience are listed in Table 4.
Table 4: Additional patients’ comments about their experience.
Discussion
With advances in surgical techniques and anaesthetic skills, increasingly arthroscopic shoulder surgery is becoming a day case procedure. Postoperative pain management after shoulder arthroscopy is a critical factor in recovery, rehabilitation, and patient satisfaction. Even with these advances, optimal pain relief remains a challenge due to considerable individual variations in the level of pain experienced.4
The success of ISB in 48 patients led to a low incidence of pain (96%) in the early postoperative period within the cohort. Of the two patients, one had moderate pain (SAD) and one had severe pain (cuff repair) in recovery, which settled quickly with a small dose of morphine (2 mg) which suggests it was unlikely to be related to block failure. The benefits of regional anaesthesia for facilitating day case surgery are widely described in the literature.5,6,7 We have not been able to accurately identify why some blocks lasted longer than others. However, we did find that three patients who did not receive any supplementary dexamethasone (intravenously or perineurally), due to other comorbid reasons, had short duration of blocks (8, 10, 17 hours respectively). It is well-established that duration of a single shot ISB can be prolonged by adjunct therapy with dexamethasone.8, 9
Follow up
Our audit has demonstrated that 20 hours of excellent postoperative analgesia may not be sufficient in some day case shoulder surgical procedures, as observed by Wilson et al.5 Regrettably we noted a 30% an incidence of severe pain at 48 hours which is higher than we have seen in previous service evaluations at our trust – 20% in 2015 and 11% in 2012 - when we conducted a follow up telephone interview at 24 hours. In a survey of postoperative analgesia following ambulatory surgery, Rawal et al found 35% of day surgery patients experienced moderate to severe pain during the first 48 hours at home in spite of analgesic medications.10 At present our routine protocol is to send patients’ home with paracetamol and codeine, but in selected cases with moderate to severe pain to send them home with additional analgesia such as tramadol or a NSAID as tolerated or indicated. In view of these audit findings, perhaps it is time to modify our protocol about take home medications.
Our patient reports of pain were diverse, and it is difficult to decipher any correlation between pain and the surgical procedure. However, cuff repairs did represent 6 of the 11 patients (54%) in severe pain in the first 48 hours despite paracetamol, codeine and NSAID, the regimen recommended in the PROSPECT guidelines for rotator cuff repair surgery.11 It is possible these are more painful procedures and would benefit from enhanced analgesia such as oramorph for 3-5 days after surgery.
Oral take home analgesia is currently the only option for day case surgery and single shot ISB only works for short periods. It is possible that our patients’ pain scores may be significantly improved if we were able to instigate a protocol to facilitate a brachial plexus catheter and continuous local anaesthetic infiltration at home. Russon and colleagues described the provision of continuous brachial plexus blocks at their Trust and noted it to produce good analgesia in 90% of their patients.12 Although this would require robust patient selection and coordination with district nursing teams, this looks to be a promising way to improve postoperative pain management and patient satisfaction.
Sleep
It is known that disturbed sleep post-operatively can negatively affect a patient’s recovery.13 In our cohort, pain satisfaction scores were affected by patient experience of poor sleep due to significant pain. How do we improve patient’s post-operative sleep? Perhaps the answer also lies in provision of regional anaesthetic catheters and home local anaesthetic infusions.
Post-operative Nausea and Vomiting
We have previously found an incidence of post-operative nausea and vomiting of 2.87% in patients undergoing any day case surgery at our unit.14 Within the cohort we followed, we noted a lower incidence of PONV (1.67%) that may be due to the lower emetogenic nature of orthopaedic surgery, the higher proportion of males in our cohort and frequent administration of dual antiemetic therapy.
Length of stay
We noted that most patients (80%) were happy with the length of stay which suggests that not only does day case surgery have an economic benefit to the NHS, but patients also prefer day case surgery.2
Patient Satisfaction
Patient satisfaction is a complex outcome to assess and is likely to be related to a number of variables within the patient journey. Some factors contributing to satisfaction in day case surgery are modifiable like managing pre-operative expectations and optimising patient experience of pain.15 Our pain satisfaction scores were not as low as may be expected for the prevalence of severe pain in our patient cohort. Obviously, patients with lower pain scores had higher satisfaction scores and vice versa; as demonstrated in Table 3, although there was no statistically significant difference in the means (P > 0.05).
Patients most frequently commented on pain and it is clearly a focus for patient satisfaction at our Trust (Table 4). While most patient comments in our study were positive and suggested a good patient experience, some were clearly dissatisfied with their pain experience. Overall, we feel the overriding patient positivity is attribute to our day case staff and demonstrates our protocols are benefiting patient satisfaction. Nevertheless, in view of some patients experiencing pain, it is clear we need to address any deficiencies in our protocols. As anaesthetists, our ability to influence surgical outcomes is limited. However, we are able to optimise analgesia for our patients and ensure plans are communicated to patients appropriately. If we are able to minimise the distress caused by post-operative pain, and manage patient expectations well preoperatively, we should be able to have a positive impact on overall satisfaction with day case shoulder surgery.15
Limitations & Conclusion
The provision of day case shoulder surgery at out Trust is well established and dependent on excellent team working between the pre-operative assessment team, anaesthetists, surgeons, and day-case ward nurses. As previously noted in the literature, we have identified that patient satisfaction appears to correlate extensively with patient experience of pain.15 While we appreciate patients’ experiences of pain could be improved, we are pleased to have found relatively high pain satisfaction scores and positive feedback from our patients. Taking into account our findings from this audit, we hope to make our post-operative pain protocols more robust and to ensure all patients receive a comprehensive written patient education leaflet about their postoperative pain management including instructions on taking oral pain killers before their block wears off. This will empower them to play their part in the recovery period and may enhance further patient satisfaction in our service.
Acknowledgements
We would like to thank all the patients, the anaesthetists, recovery, and day case staff for their assistance with data collection during the course of this service evaluation.
Conflicts of Interest: The authors have no potential conflicts of interest to declare.
References
- Appleby J. Day case surgery: a good news story for the NHS.BMJ. 2015 Jul 29;351:h4060. doi: 10.1136/bmj.h4060.
- Same day elective care – treat day surgery as the norm. Online library of Quality, Service Improvement and Redesign tools - NHS Improvement. https://improvement.nhs.uk/documents/2160/same-day-elective-care.pdf
- Conroy BP, Gray BC, Fischer RB, Del Campo LJ, Kenter K. Interscalene block for elective shoulder surgery.Orthopedics. 2003; 26(5):501-3.
- 4.White PF. Pain management after ambulatory surgery – where is the disconnect?Can J Anaesth 2008; 55(4): 201-207
- 5.Wilson AT, Nicholson E, Burton L, Wild C. Analgesia for day-case shoulder surgery.Br J Anaesth. 2004; 92:414-5.
- 6. Joshy, S., Menon, G. & Iossifidis, A. Inter-scalene block in day-case shoulder surgery. Eur J Orthop Surg Traumatol 2006;16: 327–329.
- 7.Sadashivaiah J, Ghatge S. 11. Interscalene Brachial Plexus Block for Post Shoulder Surgery Pain Relief in Day-Case Patients.Regional Anesthesia & Pain Medicine 2008; 33: e
- 8.Pehora C, Peason AME, Kaushal A, Crawford MW, Johnston B. Dexamethasone asan adjuvant to peripheral nerve block. Cochrane Database Syst Rev 2017 Nov 9; 11: CD011770. doi: 10.1002/14651858.CD011770.pub2
- 9.Cummings KC 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, Sessler DI. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine.Br J Anaesth 2011; 107(3):446-53.
- Rawal N, Hylander J, Nydahl PA, Olofsson I, Gupta A. Survey of postoperative analgesia following ambulatory surgery.Acta Anaesthesiol Scand1997; 41: 1017-22.
- Toma O, Persoons B, Pogatzki-Zahn E, Van de Velde M and Joshi GP. PROSPECT guidelines for rotator cuff repair surgery: systemic review and procedure specific postoperative pain management recommendations.Anaesthesia2019; 74: 1320-1331.
- RussonK, Sardesai AM, Ridgway S, Whitear J, Sildown D, Boswell S, Chakrabarti A, Denny NM, Postoperative shoulder surgery initiative (POSSI): an interim report of major shoulder surgery as a day case procedure. Br J Anaesth 2006; 97: 869-873.
- Su X, Wang DX. Improve postoperative sleep: what can we do?Curr Opin Anaesthesiol. 2018; 31: 83-88.
- Mayhew D, Swaraj S, Murthy BVS. Nausea and Vomiting in Daycase Surgery - a Quality Indicator. Journal of One Day Surgery 2017; 26(3): 9-17.
- Jaensson, M., Dahlberg, K. & Nilsson, U. Factors influencing day surgery patients’ quality of postoperative recovery and satisfaction with recovery: a narrative review. Perioper Med 2019; 8: 3. https://doi.org/10.1186/s13741-019-0115-1.
Table 1: The number patients having various surgical procedures and patients who were not contactable for a 48-hour postoperative follow up interview.
Table 2: Pain scores in first 48 hours following their surgery.
Table 3: Mean, median and mode patient satisfaction scores about their pain relief at rest within first 48 hours of surgery.
Table 4: Additional patients’ comments about their experience.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49086/311-murthy.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse10
Click on the image to be taken to the HCUK page about the conference.
Download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47601/hcc_bads-day-case-knee-25_03_2021.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse11
Click on the image to be taken to the HCUK page about the conference.
Download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47596/hcc_bads-day-case-hip-april-29_04_2021.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse12
Click on the image to be taken to the HCUK page about the conference.
Download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47823/hcc_bads-day-case-hip-april-29_04_2021.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse13
Click on the image to be taken to the HCUK page about the conference.
Download the pdf from the link at the bottom of the page.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47598/hcc-bads-covid-19.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse14
General Guidelines
The Journal of One-Day Surgery considers all articles of relevance to day-surgery and short-stay surgery. Articles may be in the form of original research, review papers, audits, service improvement reports, case reports, case series, practice development and letters to the editor. Research projects must clearly state that ethics committee approval was sought where appropriate and that patients gave their consent to be included. Patients must not be identifiable unless their written consent has been obtained. If your work was conducted in the UK and you are unsure as to whether it is considered as research requiring approval from an NHS Research Ethics Committee (REC), please consult the NHS Health Research Authority decision tool at http://www.hra-decisiontools.org.uk/ethics/.
Articles should be prepared as Microsoft Word documents with standard line spacing and normal margins. Submissions must be sent by email to the address below.
Copyright transfer agreement and submission
As of 7th November 2019, the JODS copyright transfer agreement must be downloaded from the resources section (tab) via the BADS website:
https://daysurgeryuk.net/en/resources/documentation/
Each named author should complete and sign a copy. Scanned copies/legible photos should be sent via email together with the main manuscript to the JODS editor: davidbunting@nhs.net
Any source of funding should be declared, and authors should also disclose any possible conflict of interest that might be relevant to their article.
Submissions are subject to peer review. Proofs will not normally be sent to authors and reprints are not available.
Manuscript preparation
Title Page
The first page should list all authors (including their first names), their job titles, the hospital(s) or unit(s) from where the work originates and should give a current contact address for the corresponding author.
The author should provide three or four keywords describing their article, which should be as informative as possible.
Abstract
An abstract of 250 words maximum summarising the manuscript should be provided and structured as follows: Introduction, Methods, Results, Conclusions.
Main article structure
Manuscripts should be divided into the following sections: Introduction, Methods, Results, Discussion and References. Tables and figures should follow, with each on a separate page. Each table and figure should be accompanied by a legend that should be sufficiently informative as to allow it to be interpreted without reference to the main text.
All figures and graphs are reformatted to the standard style of the journal. If a manuscript includes such submission, particularly if exported from a spreadsheet (for example Microsoft Excel), a copy of the original data (or numbers) would assist the editorial process.
Copies of original photographs, as a JPEG or TIFF file, should be included as a separate enclosure, rather than embedding pictures within the text of the manuscript.
Tables, Figures and Graphs
Please submit any figures, graphs and images as separately attached files rather than embedding non-word files into the word manuscript document. Tables constructed in MS Word can be left in their original MS Word file including the manuscript if this is where they were drawn.
Figures and graphs can be presented in colour but try to avoid 3-d effects, shading etc. Figures and graphs may be redrawn if the quality is not in keeping with the Journal. Please make it clear within the manuscript text where you would like tables, graphs or images to be placed in the finished article with the use of a brief explanatory legend in the manuscript file where you wish the item to be placed, e.g.
Table 1. Patient demographic details.
Figure 1. Proportion of procedures performed as a day-case each year between 2005 and 2018.
Photographs
Photographs can be provided as jpg or tiff files but should be included as a separate enclosure, rather than embedded within the text of the manuscript. This ensures higher quality images. However, we will accept images within Word documents, but image quality might suffer!
References
Please follow the Vancouver referencing style:
- References in the reference list should be cited numerically in the order in which they appear in the text using Arabic numerals, e.g. 1, 2, 3, 4 etc.
- The reference list should appear at the end of the paper. Begin your reference list on a new page and title it 'References.'
- Cite articles in the manuscript text using numbers in parentheses and the end of phrases or sentences, e.g. (1,2)
- Abbreviate journal titles in the style used in the NLM Catalogue: https://www.ncbi.nlm.nih.gov/nlmcatalog?Db=journals&Cmd=DetailsSearch&Term=currentlyindexed%5BAll%5D
- The reference list should include all and only those references you have cited in the text. (However, do not include unpublished items such as correspondence).
- Check the reference details against the actual source - you are indicating that you have read a source when you cite it.
- Be consistent with your referencing style across the document.
Example of reference list:
- Ravikumar R, Williams J. The operative management of gallstone ileus. Ann R Coll Surg Engl 2010;92:279–281.
- Dybvig DD, Dybvig M. Det tenkende mennesket. Filosofi- og vitenskapshistorie med vitenskapsteori. 2nd ed. Trondheim: Tapir akademisk forlag; 2003.
- Beizer JL, Timiras ML. Pharmacology and drug management in the elderly. In: Timiras PS, editor. Physiological basis of aging and geriatrics. 2nd ed. Boca Raton: CRC Press; 1994. p. 279-84.
- Kwan I, Mapstone J. Visibility aids for pedestrians and cyclists: a systematic review of randomised controlled trials. Accid Anal Prev. 2004;36(3):305-12.
- Barton CA, McKenzie DP, Walters EH, et al. Interactions between psychosocial problems and management of asthma: who is at risk of dying? J Asthma [serial on the Internet]. 2005 [cited 2005 Jun 30];42(4):249-56. Available from: http://www.tandf.co.uk/journals/.
Mr David Bunting
Editor, Journal of One Day Surgery
British Association of Day Surgery
Consultant Upper GI Surgeon
North Devon District Hospital
[These guidelines were last revised on 03.02.2021]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/47611/311-author-guidelines.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods?id=2169#collapse15