Tim Rowlands
Welcome to another edition of the Journal of One-Day Surgery. In this one we present 4 original articles and a report on a recent meeting on emergency care pathways.
This journal has always sought to present articles relevant to the implementation of new techniques in day surgery. Our past President, Dr Anna Lipp, co-authors 2 papers on new developments in urology. Both show how new developments in conjunction with appropriate pathways improve day case efficiency and patient care. The opportunity for enhanced tariff is attractive.
Regional anaesthesia continues to change the face of surgery. Shoulder surgery is one such area which was previously difficult in this regard. Prasad et al show good results which are sustainable in day surgery reducing the need for overnight stays.
Wright et al present their results of a recent study using the QoR-9 instrument. Whilst limited by size the study did allow a new patient information booklet to be developed. The authors rightly point out the need for further studies.
This edition goes out before the British Association of Day Surgery Annual Scientific Meeting in June 2017. I look forward already to seeing the original abstracts and presentations along with the keynote presentations and workshops put together by the BADS team and hopefully then definitive papers to follow. With the Brexit vote during last years conference and now an upcoming general election imminently I’m sure we’ll have plenty to discuss!
See you in Southport.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6148/272-editorial.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse0
Mary Stocker
I am writing this as preparations for our Annual Scientific Meeting in Southport are well underway. Once again our Conference Secretary has pulled together an inspiring programme which promises a wide variety of topics pertaining to day surgery, including day case neurosurgery and emergency day surgery. If you have not done so already do have a look at the programme on our website; at time of writing there are still places available should you wish to come along and have not already registered.
It has been a busy few months for BADS since I last wrote. We have, in collaboration with Healthcare Conferences, run two one-day conferences, the first focusing on Day Surgery Emergency Surgery. A longer report of this meeting is contained in the Journal, but I would like to thank all our external speakers and BADS Council members for delivering an outstanding meeting which stimulated much discussion and excellent delegate feedback. There is no doubt that having pushed the frontiers of elective surgery over the past 10 years emergency surgery is the next significant challenge for BADS and the work of some units across the country is truly inspiring. If this is an area which your trust is either not yet embracing or finding it difficult to tackle do consider coming to this conference when we re-run it on November 23rd. Last week we ran a third one day meeting on day surgery breast cancer surgery. This is an example of procedures where there is huge variation across the country, the best units achieving day-case rates of 90% with others rates below 10%. Once again we had inspiring presentations and very fruitful delegate engagement in discussions. There is no doubt that by learning from centres of best practice we should all be able to transform our day case outcomes.
Our representatives on the International Association of Ambulatory Surgery (IAAS) have just returned from the 12th International Congress in Beijing. I would like to remind all BADS members that you are members of the IAAS; a link to their website, newsletter, journal and congress details are available on the resources area of the BADS website. I would also like to take this opportunity on behalf of BADS to congratulate Professor Doug McWhinnie, a previous President of BADS, on being appointed President-Elect of IAAS. I would also like to thank Dr Ian Jackson who is standing down shortly as one of the BADS representatives on the IAAS committee. Ian has been a huge advocate of BADS with the IAAS over the years and his work internationally has hugely enhanced the reputation of our national organisation. Ian is irreplaceable, but Mr Kian Chin, our own President-Elect, is game for the challenge and I am sure will prove himself an able successor to Ian. He was voted onto the IAAS General Assembly in Beijing and will, with Doug McWhinnie, act as our representative to the IAAS.
I want to finish by announcing an exciting new venture. Following a survey of our members reported in the previous edition of JODS and detailed discussion by council we have decided to develop a JODS app. This will enable future editions of JODS to be produced for smart phones, tablets or websites. We are in the process of developing this and anticipate that the next edition of JODS will be electronic. The times they are a changing! Do write in and tell us what you think.
That just leaves me to say I hope to see as many of you as possible in Southport in June for two days of stimulating education and networking opportunities.
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse1
Omar Al Kadhi, Kate Manley, Madhavi Natarajan, Anna Lipp, Rachel Morris & Mark Rochester
Norfolk and Norwich University Hospital NHS Foundation Trust, Department of Anaesthesia
Keywords: HoLEP, day case pathway, laser, prostatectomy.
Introduction:
Day case Holmium laser enucleation of the prostate (HoLEP) has been described in the literature as a safe and effective treatment for small volume prostates. Day case surgery for male lower urinary tract symptoms (LUTS) confers significant financial benefits for hospital trusts due to enhanced tariffs. This study investigates the feasibility of performing day case HoLEP for any size prostate and any age of patient.
Methods:
Data was analysed for all patients listed as a day case HoLEP at a single centre over the first 26 months of a new day case service. Intraoperative details, complications, reasons for failed discharges and 6 month International Prostate Symptom Scores (IPSS) were recorded.
Comparison of complications and outcomes are compared with those in the published literature, and reasons for increased length of stay were investigated. Three year follow-up data was collected to determine later complications such as stricture formation and the need for additional surgery for bladder outflow obstruction.
Results:
267 HoLEPs were performed, 76.7% were intended as day case procedures. Of intended day case patients, 82.9% (n=170) were discharged the same day. Complications were recorded in the immediate postoperative period in 9.41%, readmission rate was 2.94% and later complications in 4.11%. Median postoperative IPSS and QoL scores were 2 and 0 respectively.
Conclusion:
Day case HoLEP is a feasible and safe treatment regardless of age or prostate size. Complication and readmission rates compare favourably with those in the published literature. As day case HoLEP attract an enhanced tariff in addition to the benefits of a reduced length of hospital stay, developing a day case service with a dedicated patient pathway is appealing.

Introduction
Lower urinary tract symptoms (LUTS) are estimated to affect more than 40% of males over the age of 50, and a significant proportion are due to the development of benign prostatic hyperplasia (BPH)1. The gold standard management for LUTS associated with BPH has traditionally been transurethral resection of prostate (TURP). This procedure is commonly performed by UK urologists (more than 42,000 per year in England and Wales) and involves resection of prostatic tissue usually using bipolar diathermy via the transurethral route. There is a significant body of literature supporting its use for improving male LUTS from objective measures such as flow rate and also through patient-reported symptom scores such as the IPSS. TURP, although used widely, has associated risks including TUR syndrome and excessive bleeding. In addition, there is a requirement for catheterisation and bladder irrigation post-operatively and increased length of stay (LOS) in the short term, and urethral or bladder neck stricture formation and retrograde ejaculation in the longer term2–4.
Since the 1980s, advances in technology have brought numerous alternatives including photoselective vaporisation of prostate (PVP), interstitial laser coagulation and Holmium Laser enucleation of prostate (HoLEP) to the fore. HoLEP was first described by Gilling et al5 and has been increasingly performed and assessed rigorously in comparison with other techniques for removal of prostate tissue. HoLEP is a minimally invasive technique involving exposure of prostatic capsule through incision and vaporisation of peri-urethral prostate using a Holmium laser through a resectoscope with continuous saline flow, followed by separation of prostatic tissue from the capsule. This tissue is subsequently broken down using an intravesical morcellator in order to extract the tissue from the bladder6. As the procedure does not use electrical current, the irrigant used during HoLEP is non-ionic thereby reducing the risk of extravasation and serum dilution resulting in TUR syndrome which is occasionally seen following prolonged TURP.
HoLEP is a relatively bloodless procedure7 and can be used to treat a broad spectrum of prostate sizes as demonstrated in a study by Kuo8 looking at retrieval tissue of very large prostates of >75g using HoLEP. Although cost analysis place each HoLEP procedure as being more expensive than TURP, cost savings made through reduced rate of blood transfusion, reduced LOS and shorter post-operative irrigation make the two procedures comparable in terms of cost efficiency7. It is increasingly popular and has been proposed as the future ‘gold standard’ as it has similar therapeutic efficacy to TURP, is more versatile and has a favourable side effect profile3,9. In addition to being suitable for any size prostate, it has also been demonstrated that advanced age should not be an issue for performing HoLEP, with a study suggesting that the procedure is safe and effective in patients over 80 years of age10.
Day case HoLEP has previously been described in the literature as a safe and efficacious management of bladder outflow obstruction for small volume prostates of <60ml. To date, several studies have been published examining the safety and success of day case HoLEP in small patient cohorts (n=30–50)11–13. We present the outcomes of a new day case service to demonstrate the efficacy of performing day case HoLEP for any size prostate over a larger patient group (n=205).
Day case urological surgery in the elderly population has gained interest over the years, elderly and medically unfit patients can be treated safely as day cases provided they are cared for in a well organised and equipped day unit. Elderly patients have reported favourable experiences with urological day case surgery14. The current study examines the suitability of day case HoLEP for patients of any age or comorbidity, with appropriate pre-operative preparation and selection.
In the UK, day case surgery attracts an enhanced hospital payment tariff – this incentive was initiated for HoLEP and TURP by the Department of Health (DoH) payment by results (PbR) office in light of increasing demand for shorter inpatient stays due to pressure on resources. In 2011, initial day case target rates for HoLEP were set at 30%. More recently, the 2014/2015 National Tariff system has suggested a target of 60% for resection of prostate by laser15. In light of the additional cost-benefit of day case surgery, this paper also briefly examines the financial implications of performing day case HoLEP when compared to TURP, the current gold-standard.
Methods
A new day case pathway for patients undergoing HoLEP was evaluated at a single centre where over 300 procedures for BPH are performed annually. The day case pathway was commenced in September 2012; all patients regardless of age or prostate volume were listed as day case procedures unless deemed unsuitable following review by a consultant anaesthetist in a preoperative clinic. Patients were excluded on the basis of anaesthetic risk (e.g. severe ischaemic heart disease or valvular disease) or if discharge on the day of surgery was deemed to be unsafe for social reasons. All surgical procedures were performed by one of three consultant urologists experienced in performing HoLEP. Patients were discharged on the day of surgery and underwent a trial without catheter (TWOC) on day 1 postoperatively in the community, facilitated by the Community District Nursing Team. Data was gathered for all intended day case HoLEPs performed over a 26 month period including patient demographics; intraoperative details – type of anaesthesia used, time taken for resection, specimen weight and immediate complications. Reasons for failed day cases and readmission rates were also collected. Factors influencing successful daycases and failed daycases were compared, statistical analysis was performed using Fisher’s exact test and unpaired t-testing. Finally, longer-term outcomes were recorded such as 6-month IPSS scores, and 3 year follow-up to identify complications such as stricture formation, incontinence and the requirement for repeat surgery. A cost-effectiveness analysis of the procedure compared to TURP was performed to evaluate the financial benefits of performing day case HoLEP.
Results
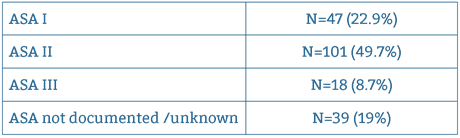
Over the 26 month period, 267 HoLEPs were performed, 76.7% (n=205) were intended as day cases. Median age was 70 years (range 44 – 89 years). American Society of Anaesthesiologists Physical Status Classification distribution is illustrated in Table 1.
27 cases (13.1%) were performed in main theatres and 86.9% (n=179) were performed in the Day Procedure Unit (DPU) theatres. The majority of cases were done under General Anaesthesia (92.23%, n=190) and the remaining 16 cases (7.77%) were done under Spinal Anaesthesia. Mean total intraoperative time was 55.91 mins with a mean enucleation time of 40.34 mins and a mean morcellation time of 15.57 mins. Mean weight of resected prostatic tissue was 32.8g (range 1–190g). Seventeen patients (8.25%) had resected weights of more than 70g.
170 patients were successfully discharged on the day of surgery (82.9%). There were 35 failed day cases – more than a third of these stayed as an inpatient for more than 1 day (range 1–4 days, mean LOS 1.5 days).
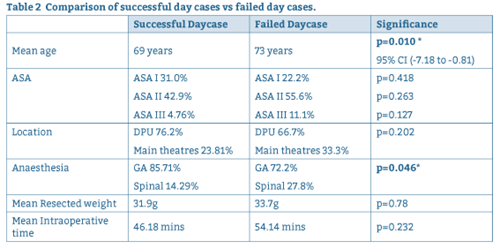
Reasons for failure of discharge on the day of surgery are summarised in Figure 1. Intraoperative factors and patient factors are compared for successful and failed day case procedures in Table 2.
Figure 1: Factors influencing failed discharge on day of surgery.
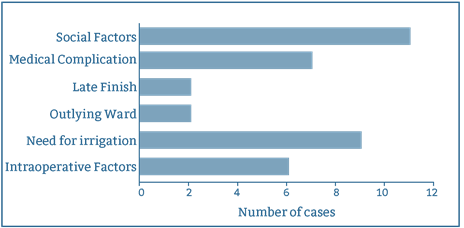
Table 2: Comparison of successful day cases vs failed day cases.
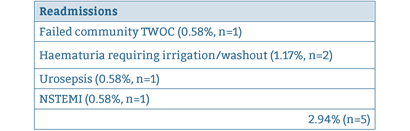
For successful day case procedures, immediate postoperative complication rate was 9.41%, (n=16) and readmission rate was 2.94% (n=5). One patient required a return to theatre for a washout / evacuation of clot from bladder for intractable bleeding. Immediate complications and reasons for readmission are summarised in Tables 3 and 4 respectively:
| Complications (immediate/early) |
| Prostate capsular perforation 2.94%, n = 5) |
| Retained fragment (1.17%, n = 2) |
| Failed TWOC (2.94%, n = 5) |
| Haematuria requiring transfusion (0.58%, n = 1) |
| Sepsis (1.17%, n = 2) |
| NSTEMI postop (0.58%, n = 1_ |
| 9.41% (n = 16) |
Table 3: Summary of Immediate /Early Postoperative Complications.
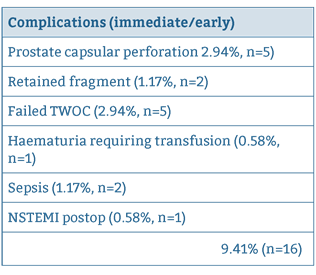
Table 4: Summary of postoperative readmissions to hospital.
Later complications such as requirement for repeat surgery and stricture formation rate are summarised in Table 5. For late complications, follow up was carried out at a median of 3.2 years (range 2.18 – 4.4 years).
Table 5: Summary of late complications.
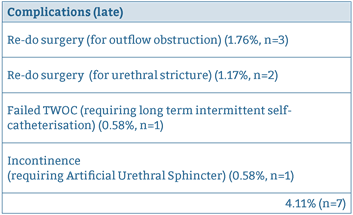
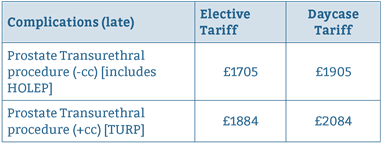
Table 6: Tariffs for HoLEP sand TURP.
Telephone follow up was conducted at 6 months and IPSS scores were collected. Of all patients contacted, a 69.7% response rate was recorded (n=143). Of the 143 patients contacted, median IPSS score was 2 "Mildly symptomatic" (range 0 – 25) and median bother / quality of life score was 0 (quality of life is assigned a score of 0 – 6, the higher score denoting greater dissatisfaction with symptoms).
Tariffs for HoLEP and TURP are summarised in Table 615. The average length of stay at our institution for TURP is 2.5 days; with the cost of an inpatient stay approximately £228 per day. Over 205 cases, it is calculated that TURP would generate a total of income £1135 per case when taking into account costs of hospital stay, compared to an income £1905 per case for day case HoLEP. This is a saving of £770 per case, which over 205 cases translates to £157,850.
Discussion
There is a significant body of evidence to suggest the HoLEP is at least equivalent, if not superior to TURP, the current gold standard. HoLEP has out-performed TURP in meta-analyses of weighted mean difference in Qmax (peak urinary flow rate) compared pre and post-operatively, and was significantly better than TURP in time spent with catheter in-situ, LOS and blood loss16–17. These findings were confirmed in a systematic review which reported that improvements to QMax and IPSS following HoLEP were significantly superior compared to TURP7. The disadvantages described with the use of HoLEP are that it requires specialist training and, hence, is not as accessible as TURP. It also requires a longer operative time, although tends to be used for larger prostates and hence efficiency of operative time related to prostatic tissue removed is comparable6,18. Despite this, HoLEP is desirable as it offers no recorded incidence of TUR syndrome5.
The results of this study suggest that day case HoLEP is indeed safe and efficacious for any age of patient and any size of prostate, provided appropriate pre-operative assessment and preparation of suitable patients is conducted. Our results compare favourably to those reported in the literature for complications, readmission rates and day case rates11–13. Outcomes such as symptom scores at 6 month telephone follow up and longer term complication rates are equivalent to TURP, in addition to a comparable mean intraoperative time2.
The achieved day case rate of 83% is more than satisfactory in light of the Department of Health (DoH) 2014/2015 National Tariff system suggested target of 60%. Performing HoLEP as a day case procedure confers significant financial benefits for an institution and enables main theatres to be used for other surgical cases which may be more in need of such a facility. Whilst the initial outlay for the laser equipment itself might be costly, the vast majority of urological units in the UK will already possess a laser suitable for HoLEP. nterest is growing in 50W HoLEP surgery given its lower capital cost 19. Whilst intraoperative time is slightly longer for HoLEP compared to TURP7, the financial cost of this is more than outweighed by the increased tariff and reduced bed occupancy afforded by day case surgery. It should also be noted that green light laser and bipolar TURP can also be done as day case procedures, however repeat surgery rates are higher for those surgeries when compared to HoLEP9.
The British Association of Day Surgery (BADS) Dataset of Procedures (Urology section) illustrates actual day case rates achieved in hospitals in England for 201520. The top 5% of hospitals achieved rate of 60%, however the top 25% achieved only 26% day case rates. The high day case rates from the current institution are largely attributed to the defined day case pathway, which ensures that appropriate patients are identified and that cases are, where possible, performed in a designated Day Procedure Unit.
Factors associated with failed day cases appear to include longer operative times, larger prostate size, increasing ASA grade, and location of procedure (in Main Theatres rather than the Day Procedure Unit). Mean age and proportion of spinal anaesthesia vs general anaesthesia were found to be statistically significantly higher in failed day cases when compared to successful ones. Factors which delay discharge such as intraoperative or anaesthetic complications are often unavoidable, however a designated day case pathway can be employed to optimise other influences, such as the location of surgery and post-operative recovery and the selection of suitable patients who have adequate support at home following discharge. The main reason for failed day cases appears to be due to lack of social support following discharge. At our institution, for a short period at the initiation of the day case pathway, pre-assessment appointments were conducted by two separate teams of nurses. Patients who were assessed by inpatient pre-assessment teams (as opposed to outpatient pre-assessment clinics) may not have adequately checked whether social circumstances were appropriate for same-day discharge – this reaffirms the importance of having a clearly defined pathway of care for a given procedure.
Effective team-working between surgeons, anaesthetists and the Day Procedure Unit nursing team is vital to ensuring the smooth running of the day case pathway, to enable appropriate pre-operative assessment and counselling of patients prior to their surgery, and to facilitate timely discharge post-operatively. We suggest that HOLEP should be assumed to be a day case pathway unless reasons are identified at surgical or nurse pre-assessment that indicate this is not likely to be possible. Achieving high day case rates for patients with any age and any size prostate is both feasible and safe and offers significant financial benefits for hospital trusts.
References
- Trueman P, Hood SC, Nayak USL, Mrazek MF. Prevalence of lower urinary tract symptoms and self-reported diagnosed "benign prostatic hyperplasia", and their effect on quality of life in a community-based survey of men in the UK. BJU Int. 1999;83(4):410–5.
- Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of Transurethral Resection of the Prostate (TURP)-Incidence, Management, and Prevention. Eur Urol. 2006;50(5):969–80.
- Razzak M. BPH: HoLEP—a steep learning curve but better for patients. Nat Rev Urol [Internet]. Nature Publishing Group; 2012;10(2):66–66. Available from: http://www.nature.com/doifinder/10.1038/nrurol.2012.236
- Chen YB, Chen Q, Wang Z, Peng YB, Ma LM, Zheng DC, et al. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year follow up. Journal of Urology. 2013: 217–22.
- Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology 1996;47(1):48–51.
- Bostanci Y, Kazzazi A, Djavan B. Laser Prostatectomy : Holmium Laser Enucleation and Photoselective Laser. 2013;15(1):1–10.
- Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al. Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement. Health Technol Assess. 2008;12(35).
- Lai M-C, Kuo Y-C, Kuo H-C. Intravesical hyaluronic acid for interstitial cystitis/painful bladder syndrome: a comparative randomized assessment of different regimens. Int J Urol [Internet]. 2013 Feb [cited 2014 Jul 21];20(2):203–7.
- Michalak J, Tzou D FJ. HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century. Am J Clin Exp Urol. 2015;3(1):36–42.
- Clyne M. BPH: Age not an issue for HoLEP. Nat Rev Urol. 2013 May;10(5):249. 1. Epub 2013 Apr 9.
- Larner TRG, Agarwal D, Costello AJ. Day-case holmium laser enucleation of the prostate for gland volumes of <60ml: early experience. BJUI. 91(1), (61–64).
- Cynk M, Georgiadis G, Moore E, Appleby J, Griffiths R, Hale J. Day-case holmium laser enucleation of the prostate. Journal of Clinical Urology 2015;8(4):268–273.
- Gabbay G et al. [Holmium laser enucleation of the prostate as a day case surgery: prospective evaluation of the first 30 patients]. Prog Urol. 2015;25(1):34–9.
- Briggs TP, Anson KM, Jones A, Coker BJ, Miller RA. Urological day case surgery in elderly and medically unfit patients using sedoanalgesia: what are the limits? Br J Urol. 1995 Jun;75(6):708–11.
- 2014/2015 National Tariff Payment System, Department of Health Gateway Reference 00883, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/300547/2014-15_National_Tariff_Payment_System_-Revised_26_Feb_14.pdf
- Aho TF. Holmium laser enucleation of the prostate: a paradigm shift in benign prostatic hyperplasia surgery. Ther Adv Urol 2013; 5(5):245–253.
- Hoffman RM, MacDonald R, Wilt TJ. Laser prostatectomy for benign prostatic obstruction. Cochrane Database Syst Rev. 2004;(1):CD001987
- Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007;94(10):1201–8.
- Khan F, Saleemi MA, Taneja S, Alam A, Al-Sheikh M, Nunney I, Aho T An Emerging Holmium laser enucleation of the prostate reality: 50-watt holium laser enucleation of the prostate surgery outcomes from a single unit. UK Journal of Urology. Apr 2016; (195)4s (570) (abstract only).
- BADS Directory of Procedures, National Dataset (Calendar Year 2015), British Association of Day Surgery, 2015.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6144/272-khadi.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse2
Mark Rochester Consultant Urological Surgeon and Service Director
Anna Lipp Consultant Anaesthetist and Clinical Lead Day Surgery
Urology, Norfolk and Norwich University Hospital, Colney Lane, Norwich UK
Aims & Objectives
Aims
Introduce an ambulatory surgical treatment option for men with lower urinary tract symptoms (LUTS) from benign prostate hypertrophy (BPH), guided by NICE recommendations1.
Objectives
- Increase theatre capacity and reduce pressure on inpatient beds, thereby reducing pressure on waiting times
- Offer greater treatment choice to men requiring surgery for LUTS from BPH
- Reduce complications from existing surgical intervention for LUTS from BPH
Context
NNUH is a large teaching hospital with a busy Urology department. It has a local catchment area of over 800,000 patients and a large elderly population. It performs 350– 400 bladder outlet obstruction procedures each year, and has significant and increasing pressure on waiting times for urological procedures, especially for cancer, where volume is high.
There is an urgent need to free up theatre capacity and inpatient beds. The current standard of surgical care offered to men with LUTS from BPH at NNUH is either transurethral resection of the prostate (TURP) or holmium laser enucleation of the (HoLEP). NNUH performs around 150 TURP procedures each year, with an average length of stay of 3 days. It performs a similar number of HoLEP procedures each year, and patients are normally discharged the same day with a catheter.
TURP and HoLEP are both performed under a general or spinal anaesthetic and take up an average of 56 and 72 minutes of theatre time (patient turnaround time) respectively. While both TURP and HoLEP are effective at relieving the symptoms of LUTS, they can be associated with significant post-operative complications, including bleeding, infection and incontinence, which can prolong length of stay and delay recovery, and can also require further intervention, Permanent side effects can include sexual dysfunction and urinary incontinence.
TURP and HoLEP also necessitate the use of a catheter after the procedure (often for several days after a TURP) increasing the risk of urinary tract infection UroLift presented an opportunity to employ an ambulatory and minimally invasive procedure to treat a large proportion of patients who require surgery for LUTS from BPH. In addition to reducing the length of stay and theatre time, UroLift is also associated with a significantly reduced risk of permanent side effects and serious complications, compared with TURP and HoLEP.
Urolift can be performed under local anaesthesia(LA) which both avoids risks of general anaesthesia and has significantly reduced costs. Local anaesthesia can be administered by the surgeon, avoiding requirement for an anaesthetist and the costs of drugs and equipment required for a general anaesthetic. If a suitably equipped procedure room is available, procedures under LA could potentially be performed there freeing up operating theatres with GA capacity for other procedures.
NICE suggests that UroLift will help improve productivity through reduced post-discharge follow-up both in primary care and outpatient settings. UroLift also does not require the patient to be catheterised, therefore reducing the risk of catheterisation-associated UTI. As a short, ambulatory procedure, performed under a local anaesthetic, UroLift provided the opportunity for more efficient use of the Day Procedure Unit at NNUH.
Methods
In January 2015, a business plan was developed and taken through usual Trust business planning process. The focus of the business case was reduction in inpatient bed days, theatre hours, waiting times and cost savings.
A particular point of interest was savings that could be made from the avoidance of fines for waiting time breaches. UroLift was approved by the New Procedures Committee in August 2015, and by the Divisional Board in October 2015, following funding negotiation with commissioners.
NNUH offers a ‘one-stop’ urology clinic, which provides comprehensive assessment of patients with urological symptoms. At this clinic, a history is taken, the patient is examined and prostate symptoms are assessed using the International Prostate Symptom Score (IPSS) questionnaire. Flow rate and residual volume are measured and patients with LUTS undergo a flexible cystoscopy to determine suitability for different surgical options.
Once a full assessment is complete, patients are counselled on the different treatment options and patient information sheets are provided. Patients leave the clinic with a management plan, which may include surgery as an option.
The first patients to be treated with UroLift were identified through a series of four dedicated one-stop LUTS clinics, which were run over November and December 2015. Clinical training for UroLift and case observation took place and in January 2016 the first UroLift procedures were performed.
Patients requiring surgery for LUTS are offered a choice of surgical options, which now include UroLift. The majority of patients requiring surgical intervention for their BPH symptoms would be clinically eligible for UroLift, however some patients would not be considered suitable due to the size of their prostate (over 100ml) or the presence of an obstructive median lobe.
UroLift procedures are performed in the Day Procedure Unit. Initially these were performed under a general anaesthetic, but as confidence of the surgeon in the procedure grew, local anaesthetic (instillagel) was offered alone or combined with propofol sedation and this is now routine. The topical local anaesthetic is chilled in the refrigerator to 4ºC and one 11ml syringe delivered after consent has been taken in the preoperative bay, 10 minutes before the procedure. Patients are encouraged to hold the tip of the penis to prevent the gel from leaving the urethra until they arrive in theatre. Two to four UroLift implants are used, depending on the size of the prostate. No catheter is used and patients are discharged as soon as they have voided – normally after a couple of hours. No routine discharge medication apart from analgesia is prescribed. Patients are followed up with a symptom score measure and flow rate at 3 months to enable prospective audit of the service.
Results and evaluation
Over 90 patients have been treated with UroLift. In the majority of these patients, local anaesthetic was used and is now routine. The results of a recent audit of the first 12 months of the service are shown in the table below.
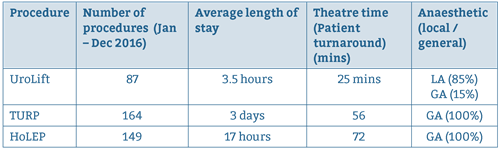
Procedure
In this cohort, the average number of implants required per patient was 2.8. However, during this early part of our learning curve, we tended to recruit patients with smaller prostates, who required fewer implants.
We currently offer UroLift to patients with prostates up to 100ml and requirement overall is up to 4 implants per patient. Complications are very rarely seen and are very minor compared with the number and severity of complications routinely reported with TURP. At the 3 month follow-up, patients had significant improvements in the key clinical parameters, including IPSS, quality of life scores, urinary flow rate (Qmax) and post-void residual volume (RV).
Encouragingly, improvements in the average IPSS mirrored that observed at 3 months in clinical trials with UroLift with a reduction in mean IPSS score from 21.6 to 12.5 and mean bother score from 4.4 to 2.3. The team concluded that UroLift is an effective treatment option for men requiring surgery for LUTS from BPH. The UroLift procedure is straightforward and easy to learn, without requirement for additional resources apart from the UroLift implants themselves. It can be easily performed under a local anesthetic, enabling quick turnaround in theatre.
Procedure time (patient turnaround time) is 25 mins, and 7-8 cases can be done in an afternoon list. Recovery is quick and the side effects and complex complications commonly associated with other surgical interventions are avoided. Unlike other surgical options for LUTS, UroLift is a true ambulatory procedure, where patients are discharged without a catheter after only a few hours and require minimal follow-up.
Analysis of the cases performed to date concluded that UroLift is a cost effective treatment, compared with other surgical options, and we expect it to provide significant efficiency and productivity savings by reducing inpatient bed stay, theatre time and follow-up. For the future role of UroLift, the team are considering moving the procedure out of the day unit into an ambulatory setting, which would relieve pressure on the Day Procedure Unit. Also the procedure may lend itself to a ‘see and treat’ pathway whereby patients are assessed and treated in the same day, which would provide further efficiency savings.
Key learning points
- Commence funding discussions with commissioners as early as possible and involve department Business Manager for support and in development of business case.
- The business case should take into consideration that most men with lower urinary tract symptoms (not in retention) and obstructing flow rate are candidates for UroLift. These men will have a prostate size of <100ml and will have no significant median lobe. The average number of implants required is less than 4, however, many patients require 2 or 3. Occasionally, with a large prostate, 5 or 6 implants are required
- Training should follow the manufacturer’s rigorous format to ensure best clinical outcomes.
- Surgeons may want to perform initial cases under a general anaesthetic until they are confident with the procedure. After this, the procedure can easily be performed under a local anaesthetic, or light sedation if required.
- Data collection and audit is very important to demonstrate patient outcomes and benefits, as well as efficacy savings.
- Assessment of patients is best carried out in a one-stop clinic, with access to cystoscopy, in order to limit patient visits.
Reference
1 https://www.nice.org.uk/guidance/conditions-and-diseases/urological-conditions/lower-urinary-tract-symptoms
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse3
Ganesh Prasad. ST5 Trauma and Orthopaedic Surgery, Nottingham University Hospitals NHS Trust, Nottingham UK
Paul Townsley Consultant Anaesthetics, Nottingham University Hospitals NHS Trust, Nottingham UK
Benjamin WT Gooding Consultant Shoulder and Elbow Surgeon, Circle Nottingham NHS Treatment Centre, Queen’s Medical Centre Campus, Nottingham UK
Arthroscopic shoulder surgery with overnight admission is commonplace due to concerns about pain relief in the first 24 hours and perceived need for clinical and physiotherapy assessment after an anaesthetic block has worn off. With an aim to assess the safety and effectiveness of same day discharge for arthroscopic shoulder surgery done on afternoon lists, we retrospectively analysed 140 cases in a 27 month study period. All patients underwent surgery awake under regional anaesthesia. Patients were reviewed by our physiotherapist and discharged irrespective of return of motor and sensory function. There were no re-admissions during the study period and no overnight calls. Arthroscopic repair requiring post-operative immobilisation was performed in 44 (31%) cases (28 rotator cuff repair, 13 stabilisation and 3 long head of biceps tenodesis). The cost saving for this cohort of 140 cases compared with overnight admission was £56,000 (based on the NHS estimate of a £400 overnight bed stay). This study demonstrates that awake ambulatory arthroscopic shoulder surgery with regional anaesthesia and same day discharge is safe and efficient, even if surgery is performed in the afternoon with discharge into the evening.
Introduction
Arthroscopic shoulder surgery with overnight post-operative admission is commonplace, particularly for patients having repair procedures such as rotator cuff repair. This is often due to concerns about pain relief1 and a requirement for clinical and physiotherapy assessment once the effect of an anaesthetic regional nerve block has worn off. Evidence also suggests the readmission rate is higher for those undergoing this type of surgery later in the day2. In our unit, arthroscopic shoulder surgery patients including those having repair procedures are discharged the same day, even if performed on an afternoon list.
The aim of this study was to assess the safety and efficiency of same day discharge for arthroscopic shoulder surgery performed awake under regional anaesthesia on afternoon operating lists.
Methods
We performed a retrospective analysis of a prospectively collected database of all shoulder surgery done on afternoon operating lists in a single institution (Circle Nottingham NHS Treatment Centre) by the senior author over 27 months from October 2013. Patient electronic records and episode duration were gained from the trust NOTIS software. We analysed the type of operation, type of anaesthesia, duration of patient stay, incidence of readmission in the 24 hours following surgery and the incidence of emergency telephone advice sought in the 24 hours following surgery.
Results
140 arthroscopic shoulder surgeries were performed on afternoon operating lists during the study period. Arthroscopic repair requiring post-operative immobilisation was performed in 44 (31%) cases (28 rotator cuff repair, 13 stabilisation and 3 long head of biceps tenodesis). All patients underwent surgery under regional anaesthesia and were either awake or received conscious sedation. All patients were discharged irrespective of return of motor and sensory function after being reviewed by a physiotherapist. All patients were discharged with multimodal analgesia to take when the regional block wore off. The analgesia regimen used consisted of regular paracetamol, a regular non-steroidal anti-inflammatory and either dihydrocodeine or oral morphine as required. They were given an advice sheet and contact details in case of any concerns or an emergency. During the study period, there were no re-admissions and no overnight calls to our physiotherapist.
The mean episode duration from admission to discharge was 4hrs 30mins. The cost saving for this cohort of 140 cases compared with overnight admission was £56,000 (based on the NHS estimate of a £400 overnight bed stay).
Discussion
There has been an exponential growth in the volume of arthroscopic shoulder surgery and various anaesthetic techniques have been utilised to provide effective anaesthesia and post-operative analgesia. The Interscalene Block has emerged as the most effective anaesthetic technique for shoulder surgery3 and is widely employed as the anaesthetic of choice in various centres in the UK4.
Saeed et al published that the time of surgery is a significant risk factor in predicting overnight admission to hospital following daycase arthroscopic shoulder surgery2. Majority of patients in this study group had a general anaesthetic (GA) with local infiltration around the arthroscopy portals and into the shoulder joint. Post-operative pain (62.1%) and poor recovery from GA (27.6%) were cited to be the two most common reasons of delayed discharge. Patients undergoing arthroscopic shoulder repair on afternoon operating lists under regional anaesthesia have previously been admitted overnight due to concerns about pain relief and the need for assessment after the block has worn off, especially for those undergoing repair procedures requiring limb immobilisation.
This study demonstrates that awake ambulatory arthroscopic shoulder surgery with regional anaesthesia and same day discharge does not lead to readmissions, even if surgery is performed in the afternoon, with discharge into the evening.
We believe that the factors which contribute to successful daycase ambulatory shoulder repair surgery service are:
- Regional anaesthesia performed awake or with conscious sedation.
- An appropriate take home analgesia regimen.
- Early physiotherapy assessment and advice prior to discharge from hospital.
- Comprehensive patient information delivered in person and reinforced with a take home advice leaflet.
References
- Day-Case Surgery: Anesthetic Challenges. Kathryn E McGoldrick. Ambulatory Surgery. 2012; 17(3): 47–49.
- Does the time of day-case shoulder arthroscopic surgery influence the rate of unplanned admissions? Saeed Z, Radwan R, Trickett R, Pullen H. The Journal of One-Day Surgery. 2014; 24(4): 100–102.
- Current Concepts in Anaesthesia for Shoulder Surgery. Sulaiman L, MacFarlane RJ, Waseem M. Open Orthop J. 2013; 7: 323–328.
- Setting up an upper limb regional anaesthesia service for day surgery – a practical guide. www.daysurgeryuk.net/handbooks.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6142/272-prasad.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse4
Kirsty Wright Anaesthetics, Ninewells Hospital
Jaqualyn Fisher. Anaesthetics, Ninewells Hospital
Christina Beecroft Consultant Anaesthetist, Ninewells Hospital
Lawrence Li Anaesthetics, Ninewells Hospital
Department of Anaesthesia, Victoria Hospital, Kirkcaldy KY2 5AH
Introduction: A good post-operative recovery after day surgery is hard to define. However, the 9 item quality of recovery (QoR-9) score takes a number of factors into consideration and has been validated in day surgery. Pain relief contributes to this and also features prominently in many day surgery guidelines. This pilot study aimed to evaluate the adequacy of pain relief and quality of recovery in a Scottish population.
Method: Adult patients under-going day surgery (including general surgical, urological, gynaecological and orthopaedic procedures) were recruited over a ten-week period. Procedural data was collected from the anaesthesia and recovery charts. Patients were also asked to complete a QoR-9 questionnaire and analgesia requirements on postoperative days (POD) 1 and 3.
Results: 63 patients were recruited and 42 (66.6%) returned their completed questionnaires. Of these, 39 (93%) were given instructions regarding postoperative analgesia. On POD 1 and 3, 37 (88%) and 28 (66.5%) patients respectively, found their analgesia to be effective. The average QoR-9 scores were 15.5/18 on POD 1 and 15/18 on POD 3.
Discussion: Pain is universally ranked highly in importance in post-operative recovery amongst patient groups. However, these results confirm recovery after day surgery may be multifactorial. While there is room for improvement within the management of postoperative analgesia within our population, future research and improvement work can focus on what factors can be improved to contribute to a good postoperative recovery after day surgery.
Introduction
The number and complexity of day case procedures are increasing1, and effective pain management remains fundamental in the perioperative care and discharge planning for day surgery patients. Guidelines on the provision of day surgery services have been published by a number of organisations including the Association of Anaesthetists of Great Britain and Ireland (AAGBI)2 and the Royal College of Anaesthetists (RCOA)3, which reinforces the importance of providing clear instructions on post-operative pain management plans for the patient. Regular audit and review of current practice in each day surgery unit should be encouraged to assess adherence to local protocols and ensure a high quality service.
Post-operative pain remains one of patients’ main concerns, and good pain relief has implications on the quality of recovery as it allows earlier mobilisation, reduced complications, fewer interventions by primary care and earlier return to work with physical, psychological and economic benefits. Uncontrolled pain can result in both emotional and physical suffering in the short term, and also increases the risk of developing chronic pain4. Residual discomfort has been reported in some cases up to 4 weeks postoperatively5.
Pain clearly plays an important part in patient recovery. However, the assessment of pain remains subjective, and in itself does not describe the impact on quality of life. It is clear that good postoperative recovery depends on more than the return of physiological parameters to normal, and includes functional ability, cognitive recovery and patient satisfaction. The lack of a ‘gold standard’ definition of quality of recovery and the qualitative nature of these parameters make this inherently difficult to objectively measure. The Quality of Recovery 9 (QoR-9) score has been shown to be useful for assessing overall patient recovery6. This was developed by surveying 4 main populations (patients, relatives, medical and nursing staff), and asking them to rate 61 postoperative features. The 9 most highly ranked items were subsequently included in the index score. Each item was then allocated a score of 0–2, giving a maximum score of 18. It has been validated and used in assessing recovery in patients after both major and day case surgery6,7.
We conducted a pilot study to evaluate the adequacy of pain relief and quality of recovery in a Scottish population. As part of the study, we reviewed the adherence of local practice to guidelines on post-operative instructions.
Method
The study protocol was approved by the local research ethics board. Adult patients under-going general surgical, urological, gynaecological and orthopaedic surgery as day case procedures within NHS Tayside were recruited. As this was a pilot study, we aimed to recruit patients over a ten-week period. Informed consent was obtained from all participants.
Information on the type of procedure, anaesthetic, perioperative analgesia requirements (including recovery) and postoperative pain scores were collected by the research team on the day of surgery. Participants were then asked to complete a questionnaire on postoperative days (POD) 1 and 3 to assess their analgesia requirements, pain and QoR-9 scores. These were returned by post after completion. Participants were followed-up by telephone to encourage return rate.
Results
Sixty-three patients were recruited over the ten-week period. Of these, 42 (66.6%) returned their completed questionnaires and were included in subsequent analysis. The patient demographics are shown in Table 1.
Forty out of 42 patients (95%) were discharged home on the day of surgery as planned. One patient lived alone and one patient required supplemental oxygen postoperatively, preventing discharge on the same day.
Discharge
Thirty-six (86%) patients were discharged home with analgesia. Eight (22%) received simple analgesia only (paracetamol +/- ibuprofen) and 28 (78%) received simple analgesia and a weak opioid (Tramadol or codeine). Of the 42 patients who returned their questionnaires, thirty-nine (93%) were given instructions regarding postoperative analgesia for discharge. This information came from 4 different sources: anaesthetists (7, 18%), surgeon (7, 18%), recovery nurse (18, 46%) and ward nurse (31, 79.5%). Fourteen patients (36%) received information from more than one person. Twenty patients (51.5%) received verbal information only, 2 patients (5%) received written information only and 17 patients (43.5%) were given both verbal and written information.
Pain Scores
Pain scores were collected in the post-anaesthetic recovery, and from patient questionnaire on POD 1 and 3 (Table 2).
On POD 1, 30 patients (71.5%) were using their analgesia regularly and 37 patients (88%) found their discharge analgesia to be effective. Two patients (5%) sought further advice regarding their pain management. One patient contacted their GP, the other patient did not report the source of the advice on the questionnaire. On POD 3, 28 patients (66.5%) were using regular analgesia and 31 patients (74%) found this to be effective. Three patients (7%) sought further advice, one contacted their GP, one contacted NHS 24 and one contacted both their GP and NHS 24.
Quality of Recovery Score
The QoR-9 questionnaire was also completed on POD1 and POD3 (Table 3). The mean score on day 1 is 15.5/18 and 15/18 on day 3.
Discussion
The RCOA recommends a number of targets regarding best practice in managing postoperative pain and analgesia in day case surgery8. These include: 100% of patients discharged with both verbal and written instructions regarding analgesia, fewer than 5% reporting ‘severe’ pain and the majority (85%) reporting ‘none’ or ‘mild’ pain in the first 48 hours. Our results show that in this patient group, none of these 3 targets were achieved, indicating significant room for improvement of postoperative pain management within our service.
We examined the QoR-9 score as a tool to objectively assess the quality of postoperative recovery in our population. The maximum potential score available is 18, with a score of 17 or greater indicating a good recovery and a score of 15 or less indicating a poor quality of recovery6. In our study the QoR-9 was low on both POD1 and POD3 after surgery, indicating a poor quality of recovery which persisted. This had been demonstrated in previous studies where QoR-9 scores returned to their pre-operative values between postoperative days five to seven after major surgery7,9. It is interesting to note however, that while overall pain scores improved from day 1 to day 3, the QoR-9 score remained low. This confirms that amongst our patient group, other factors may play a role in a patient’s perception of the quality of their recovery. Subsequent to the development of the QoR-9 score, and more detailed QoR-40 questionnaire has been designed10. This has been more extensively studied and validated. However, as participants were being asked to complete the questionnaire on two separate days postoperatively, the QoR-9 score was deliberately chosen so as not to over face the participants and encourage completion.
Postoperative quality of recovery is multifactorial, and the contributing factors are ranked varyingly dependant on the group of individuals asked6. Arnberger et al found that pain was universally ranked highly, and therefore of importance in recovery, by the three main groups (doctors, nurses and patients/relatives). However, an interesting difference between patient and doctor groups was the ranking of support from others (including doctors, nurses and family members), with a consistently higher importance placed by patients on this compared with doctors. This is reflected in our results, with lack of support from others contributing to the low QoR-9 scores. However, the phrasing of the question regarding support within the QoR-9 survey is important. It simply asks whether the support from others is present, but not if it is required. The withdrawal of support could reflect the increasing independence of the patient by postoperative day 3, rather than a need which is not being met. Further clarification of this is required.
This pilot study was limited by small numbers and lack of statistical analysis. For example, we are unable to assess whether certain operations contributed to the low QoR-9 scores over others. Another confounding factor was the relatively low return rate of the questionnaires. This could simply be due to non-compliance with the participants, or that only those who felt able to completed the questionnaire and so were more likely to reflect a good recovery. Nonetheless, areas for improvement within our service can be identified. As a result, a patient information leaflet containing information and instructions on discharge analgesia has now been developed and put into clinical practice. Furthermore, our results suggest that quality of recovery may be slow despite the common perception that recovery from day case surgery may be rapid. This has potential for socioeconomical impact particularly in young patients where return to work is delayed or more support is required from carers after surgery. We did not explore whether patients or their carers were off work for longer than expected. Further studies are required to assess the correlation between types of anaesthetic (such as regional versus general) and the quality of recovery after day surgery.
Competing Interests: None declared
Acknowledgements
The authors would like to thank Dr Jenny Parsons, Ninewells Hospital.
References
- BADS Directory of Procedures: 5th edition. BADS, June 2016.
- Verma R et al. Day case and short stay surgery: 2. Anaesthesia 2011;66:417–434.
- Guidelines for the provision of anaesthetic services: Anaesthesia services for day surgery 2015. RCoA London 2015.
- Postoperative pain management. http://www.esiaeurope.org/Postoperative Pain management.pdf
- Brattwall M et al. Patients’ assessment of 4-week recovery after ambulatory surgery. Acta Anaesthesiol Scand 2011;55(1):92–98.
- Myles PS et al. Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesth Analg 1999;88:83–90.
- Arnberger M et al. Evaluation of physical and mental recovery status after elective liver resection. Eur J Anaesthesiol 2009;26:559–565.
- Raising the standard: a compendium of audit recipes (3rd Edition). Section 5: Day surgery services. RCoA London 2012.
- Wu CL et al. Correlation of postoperative pain to quality of recovery in the immediate postoperative period. Reg Anesth and Pain Med 2005;30(6):516–522.
- Myles PS et al. Validity and reliability of a postoperative quality of recovery score: the QoR-40. British Journal of Anaesthesia 2000;84(1):11–15.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6143/272-wright.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse5
Most of us who are regularly involved with managing patients requiring urgent and emergency care are well aware that many of the procedures required would be well suited to management on a day case basis. However this rarely happens and many patients wait sometimes several days, recurrently fasting and occupying much needed in-patients beds both before and after their surgery. The organisation of pathways for these urgent cases is considerably more challenging than that required for planned elective care but in a few centres considerable experience has already been gained in delivery of urgent care and the Ambulatory Emergency care Network has been established to support these developments.
The session started with presentations on the key elements of day surgery pathway and criteria for suitability for day surgery management presented by Anna Lipp and Theresa Hinde form BADS Council. This session addressed the specific challenges posed by patients presenting with acute conditions requiring assessment , preparation and surgery in a short time frame. The particular benefits of day surgery for elderly and frail patients were discussed and the importance of not excluding patients on basis of arbitrary limits such as BMI or ASA grade was emphasised.
Doug McWhinnie, a former president of BADS, reviewed the progress of emergency day surgery looking at where we have come from and what has been achieved to date. A well recognised urgent day surgery programme for general surgery has been developed in Bath under the leadership of Sarah Richards, a Consultant General Surgeon and she delivered an inspiring account of the process they followed to establish their Emergency Surgical Ambulatory Care Unit. She described how their unit now functions including the use of an innovative "virtual ward" which can avoid need for admission in many cases and limit it considerably in others.
The afternoon sessions included a presentation from James Brown an upper GI surgeon at the Northumbria Specialist Emergency Care Hospital. This innovative approach to managing the increasing burden of urgent surgery in a hospital designated solely for urgent care was impressive.
Andrew Mitchell, an advanced nurse practitioner from the Ambulatory Emergency Care Network described what lessons could be learned from the experiences gained in managing urgent presentations in medicine, focussing on leadership from senior doctors, team working and ready access to diagnostic and other specialty support services.
Finally a series of presentations illustrated established pathways from centres around the country , including upper limb trauma from Rotherham , by Alex Kocheta; the abscess pathway followed in Torbay presented by Mary Stocker, and two examples of management of ERCP after miscarriage from Jane Montgomery( Torbay) and Kim Russon (Rotherham).
There was lively discussion and contributions from the multi disciplinary audience who were keen to benefit from the access to experts in various aspects of day case and urgent surgery, and evaluation of the day has been so over whelming positive that it is likely a similar event will be run again in the future. Watch out for dates.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6145/272-meeting.pdf
Cite this article as: https://bads.co.uk/for-members/journal-of-one-day-surgery-jods/?id=1103#collapse6